Isolated Painless Foot Drop due to Cerebral Infarction Mimicking Lumbar Radiculopathy: A Case Report
Article information
Abstract
Although they usually originate from peripheral problems, foot drop is caused by lesions affecting the neural pathway related to dorsiflexor muscles, whether of central or peripheral origin. We present a patient with sudden isolated foot drop caused by a small infarct in the primary motor cortex mimicking a peripheral origin. This report indicates that patients presenting isolated foot drop should be managed carefully and the possibility of both central and peripheral causes should be considered. To our knowledge, this is the first report of sudden isolated foot drop caused by a cortical infarction mimicking lumbar radiculopathy.
INTRODUCTION
Isolated foot drop of a single leg is the weakness of the dorsiflexor muscles of the foot, and this usually arises painlessly due to peripheral neuropathy, such as peroneal nerve damage or radiculopathy. Here, we introduce a case presenting sudden isolated foot drop caused by a small cerebral cortical infarction in the anterior cerebral artery territory, which mistaken for a condition from radiculopathy.
CASE REPORT
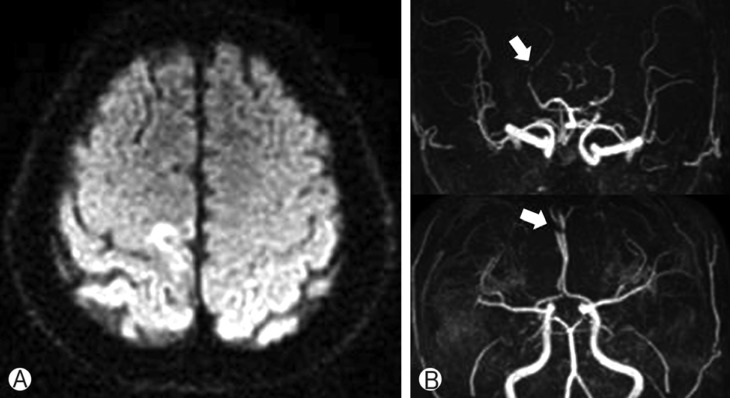
A 71-year-old man visited hospital with lower back pain, paresthesia, and weakness in his left foot that had been present for one week. When presented in clinics, the paresthesia had disappeared, but he still could not move his left ankle. The sensory exam was normal, as were his deep tendon reflexes (DTR), superficial reflexes, and pathologic reflexes. In the neurologic exam, he was alert and oriented, and his cranial exam responses were intact. Previously, he had undergone surgery for a varicose vein in his right leg ten years ago and endoscopic surgery for a gastric adenoma three years ago. He did not have a history of peripheral neuropathy or systemic diseases, such as hypertension or diabetes. A lumbar spine magnetic resonance imaging (MRI) showed a ruptured disc, which was compressing the nerve root on the left side of L4/5, and degenerative spondylosis in L5/S1 (Fig. 1). The electromyography (EMG) and nerve conduction study (NCS) showed decreased amplitude and prolonged latency in the left peroneal and tibial compound muscle action potential and normal sensory findings. This means that there was lumbar radiculopathy in L4/5 (Fig. 2). The brain CT and plexus MR did not show any specific findings. With several days of daily rehabilitation physiotherapy, his lower back pain partially improved, while his motor power was not recovered. A follow-up NCS and EMG did not show any changes. Surgery for decompression and fusion in the lumbar spine was performed. After the surgery, the weakness still did not change. At postoperative day 8, the deep tendon reflex was increased on the left ankle and ankle clonus was noticed. The whole spine MRI and brain MRI were immediately executed, and they revealed a small area of restricted infarction in the right parietal cortex with anterior cerebral artery (ACA) and posterior cerebral artery (PCA) stenosis on the left side (Fig. 3). For a detailed stroke investigation, electrocardiography and echocardiography were performed, and the results showed no specific problems. The patient was treated with a daily antiplatelet and adjuvant physiotherapy for foot drop. A month later, his motor deficit had improving, up to grade III.

Cervical magnetic resonance image (A) and brain computed tomography (B) did not show any specific lesion for left foot drop. Lumbar magnetic resonance images (C and D) revealed lumbar disc herniation and compression of the nerve root on the left side of L4/5, and degenerative spondylosis in L5/S1.

The nerve conduction study revealed decreased muscle action potential in the left peroneal region (arrow). This finding indicates the presence of lumbar radiculopathy.
DISCUSSION
Cerebral impulses are conducted via the corticospinal tract to target muscles, and this enables us to move our extremities. An arising problem in this pathway is being unable to move the extremities, which is called paresis. Isolated foot drop of a single leg is the weakness of the dorsiflexor muscles of the foot, and this usually arises painlessly due to peripheral neuropathy, such as peroneal nerve damage or radiculopathy17). Isolated painless foot drop is also caused by central origin, but this is rare, and there are only several reports of acute infarction mimicking peroneal neuropathy45910). Painless foot drop due to lumbar disorder is also uncommon13). These cases of painless foot drop were reported to be caused by lumbar disc disorder and treated surgically. These reports are cases presenting sudden isolated foot drop caused by a small cerebral cortical infarction in the anterior cerebral artery territory.
Our patients presented lower back pain and leg weakness. The results of the examination for the lumbar spine were consistent with the peripheral cause of foot drop, including weakness below the level of the ankle, and the lumbar spine MRI, NCS, and EMG included initial and follow-up results except the lack of sensory deficit or disappearing of paresthesia in the dorsal surface of the left foot. After surgery for lumbar disorder, hyperactive DTR rather than motor improvement was observed. This prompted us to evaluate the brain with MRI, which revealed a late subacute stage of infarction in the right paracentral lobule and the parietal medial cortex. This lesion is considered consistent with the somatotopic ankle and toe topography in the motor homunculus. The MR angiography showed PCA and ACA stenosis.
Anterior cerebral artery territory is most commonly reported to affect leg monoparesis268). In our patient, ACA infarction via artery-to-artery embolism was considered the main cause of the acute foot drop, although the exact pathogenesis of the stroke was unclear.
Unlike previously reported cases, this patient showed similar symptoms, but had a peripheral lesion in the lumbar spine with a simultaneous central lesion in the primary motor cortex. In this case, the lesion of the upper motor neuron was masked by the lower motor neuron lesion. Physicians could be confused when diagnosing this condition. As far as we are aware, this is the first report of isolated foot drop caused by a cortical infarction that was masked by a peripheral lesion.
CONCLUSION
In conclusion, central nervous system lesions that also affect the monoparesis of the extremities have to be considered, especially when atypical findings for peripheral lesions are present.
ACKNOWLEDGEMENT
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.