Cervical Epidural Abscess: Rare Complication of Bacterial Endocarditis with Streptococcus Viridans: A Case Report
Article information
Abstract
Although many patients with infective endocarditis (IE) complain of joint, muscle, and back pain, infections at these sights are rare. The incidence of spinal abscess in cervical spine complicating endocarditis is very rare. Although the surgical management is the mainstay of treatment, conservative treatment can get success in selected patients. We report a patient with cervical epidural abscess due to Streptococcus viridans endocarditis. Both epidural abscess and IE were managed conservatively with intravenous antibiotics for 8 weeks, with recovery. It is important to remind spinal epidural abscess can occur in those patients with bacterial endocarditis.
INTRODUCTION
Spinal epidural abscess is a surgical emergency that requires immediate decompression7). The common causes of epidural abscess are surgical interventions in the spinal canal and spread from nearby bone or soft tissues2). Conservative management of epidural abscess is reserved for patients with poor surgical risk or patients without any neurological deficit2). The association between spinal epidural abscess and infective endocarditis (IE) has rarely been described3). In fact, only eleven cases of vertebral osteomyelitis complicating streptococcus viridans endocarditis have been previously reported, and of these, only three were located in the cervical spine. The authors present a case of cervical epidural abscess associated with streptococcus viridans endocarditis.
CASE REPORT
A 44-year-old man was admitted with severe posterior neck pain radiating to both shoulder of 13 days duration, and which had aggravated 4 days before admission. His symptoms were further aggravated by a cervical epidural block. He had been transferred from other hospital. He developed high-grade fever on the day of hospitalization. On examination, he was febrile (38℃), with a pulse rate of 110/min and blood pressure of 120/60mmHg. Chest auscultation revealed coarse crepitations in the left infrascapular area. Neurological examination revealed no motor weakness or sensory loss. Investigations showed a total leukocyte count of 12,860/µl, ESR 23mm/hr, and CRP 24.96mg/dl. Renal and liver function tests were normal. Chest X-ray showed no active lesion in either lung or heart enlargement. He was already treated by the triple antibiotics (ceftriaxone, vancomycin, rifampin) before admission. But intravenous antibiotics were changed to ceftriaxone and gentamycin, because one initial blood culture grew Streptococcus viridans. The patient had a previous history of heart disease some 10 years before admission. Magnetic resonance imaging (MRI) of the cervical spine showed the highly enhanced epidural mass on C3-4 and no paraspinal abscess (Fig 1), and transesophageal echocardiography (TEE) depicted the small mobile vegetation on the tricuspid valve side, and an underlying subaortic ventricular septal defect (VSD) lesion (Fig 2). We planned the conservative treatment except in case of developing the neurologic deficit or increasing epidural abscess on follow-up MRI. And we decided to continue the intravenous antibiotics for 8 weeks when his pain improved within 2 weeks of admission. Follow-up MRI of the cervical region after four weeks of intravenous antibiotics treatment showed resolution of the epidural abscess, but newly developed discitis and osteomyelitis. And follow-up echocardiography at four weeks showed no change in the vegetation. MRI taken after four months of treatment revealed complete resolution of discitis and osteomyelitis (Fig 3). The patient was well at his 6-month follow-up, and symptoms almost completely subsided.
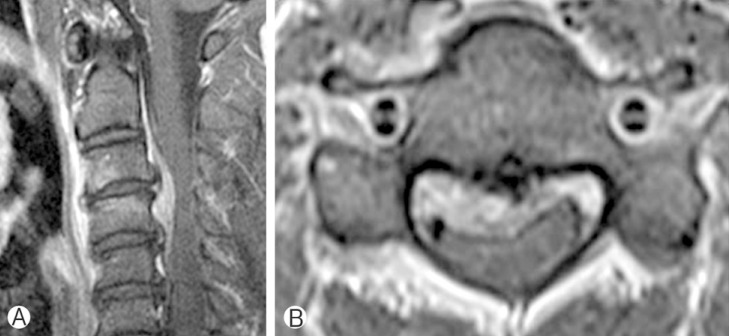
(A) A T1-weighted sagittal MR image after intravenous gadolinium injection showing an epidural abscess located adjacent to the anterior aspect of spinal cord and extending from C3 to C4. (B) A T1-weighted axial MR image with enhancement showing marked compression of the anterior spinal cord at this site.
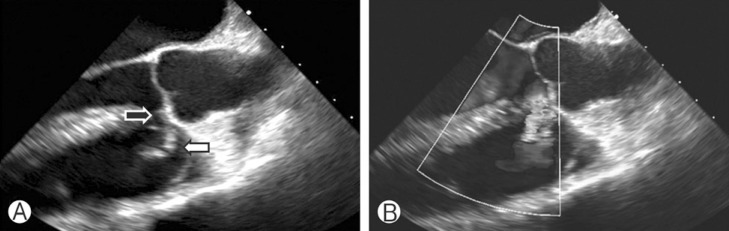
(A) Transesophageal echocardiograph showing the underlying subaortic ventricular septal defect (black arrow) lesion and the small mobile vegetation on the tricuspid valve side (white arrow). (B) The Doppler image demonstrating shunt flow from the right to the left ventricle.
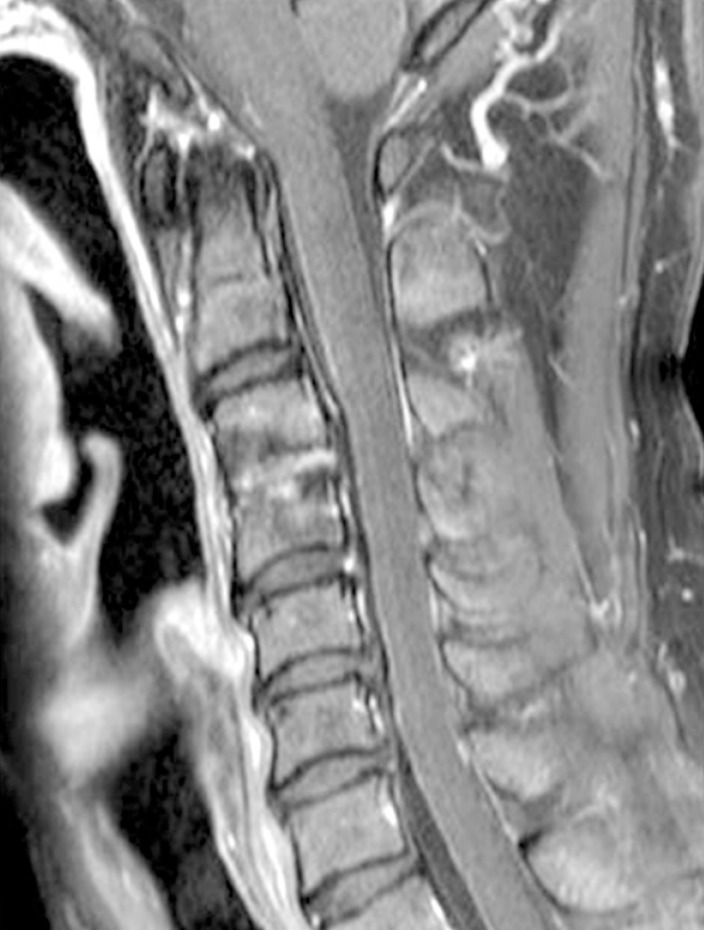
Gadolinium-enhanced T1-weighted sagittal MR image of the lesion after 4 months of antibiotic therapy showing the cervical epidural abscess had significantly decreased in size. However, the presence of a hyperintense and contrast-enhanced disc space and vertebral body suggested discitis and osteomyelitis.
DISCUSSION
Spinal epidural abscess is a rare clinical condition with an estimated incidence of 0.2-1.2/10,000 hospital admissions in the western world4). Its usual causes are intervention in the spinal canal (lumbar puncture, any surgery), hematogenous spread from skin and soft tissues, direct extension of vertebral osteomyelitis, abdominal abscess, infection of the mediastinum, and rarely IE. In fact, 14-22% of epidural abscess cases are associated with spine surgery or a percutaneous spine procedure18). Blunt trauma possibly precedes symptoms of spinal epidural abscess in 15-35% of cases14). The most common causative organism, Staphylococcus aureus, is present in up to 70% of all spinal epidural abscesses, and is followed by Streptococcus species, which account for approximately 7% of spinal abscesses18). Mycobacterium tuberculosis, fungal species, and parasitic organisms are exceptionally rare causes of spinal epidural abscess.
In the present case, although he had been treated by acupuncture and epidural block, we thought the origin of the cervical epidural abscess was not iatrogenic, but rather IE, because his symptom started before these treatments. In addition, the patient already had an underlying subaortic VSD.
The initial result of blood culture on our case was Streptococci viridans. The three most common organisms responsible for IE are Streptococci viridans, Staphylococcus aureus, and Coagulase negative Staphylococci22). Streptococci viridans is the most common causative organism and accounts for 50% of IE cases.
As was observed in our case, cervical abscess could be originate from embolic involvement of aortic valve endocarditis by hematogenous spread3). However, IE can develop without a valve anomaly. Bayer et al.5) reported that, 18% of septicemia patients without a cardiac anomaly may have echocardiographic evidence of endocarditis.
A MEDLINE search of IE revealed an incidence of vertebral osteomyelitis of 6.5% among 1,099 IE patients6,9,11,21). Although Streptococcus viridans is the most common causative organism, Staphylococcus aureus is the most common organism to cause vertebral osteomyelitis subsequent to IE. In a literature review, in 11 (23%) of 48 patients with vertebral osteomyelitis due to endocarditis Streptococcus viridans was identified as the causative organism. The viridans group stretocococci involved the 6 major groups: the S. mutans group, S. salivarius groups, S. anginosus group, S. mitis group, S. sanguinis group and S. bovis group13). Table 1 summarizes the 12 reported cases of Streptococcus viridans endocarditis with vertebral osteomyelitis, including one present case (Table 1). However, vertebral osteomyelitis has only been previously reported in 3 cases (25%) in the cervical spine.
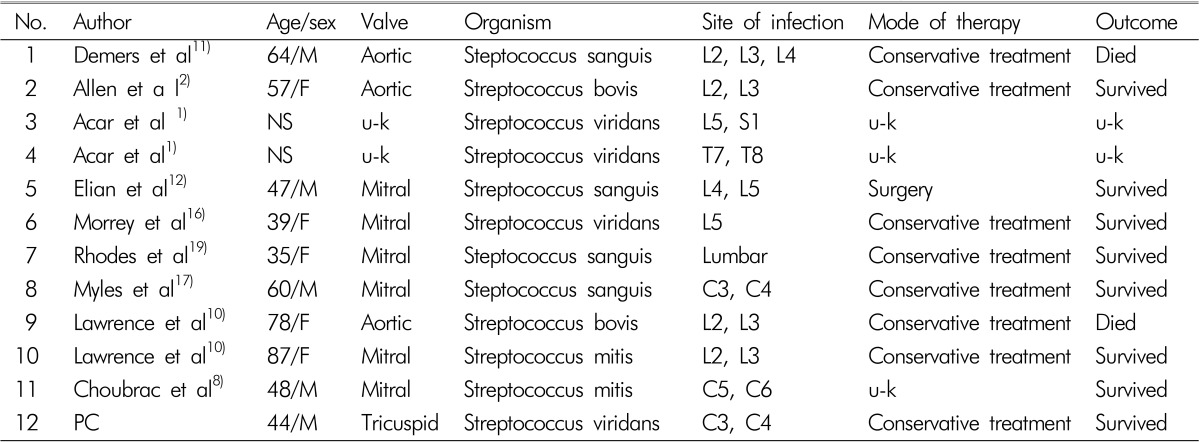
Clinical summary of vertebral osteomyelitis complicating infective endocarditis caused by streptococcus viridans
The treatment of spinal epidural abscess usually consists of decompressive laminectomy and debridement with antibiotics20). However, many cases have been managed conservatively15). Conservative management is reserved for poor risk patients with concomitant medical problems, patients with an extensive epidural abscess (from the cervical to lumbar region), patients with complete paralysis lasting for more than three days, and patients with no neurological deficit7). In our case, conservative management was adopted because he was neurologically intact. As is shown by Table 1, the majority of patients with a spinal abscess caused by Streptococcus viridans endocarendocarditis improved after conservative treatment (Table 1).
In our opinion, spinal epidural abscess with Streptococcus viridans endocarditis is usually benign course. So if the culture proven Streptococcus viridans or patients have the history of cardiac valve anomay, generally IE should be confirmed by echocardiography and epidural abscess could be cured by conservative treatment.
CONCLUSION
Spinal epidural abscess rarely accompanies IE. When encountered Streptococci viridans is the most common causative organism, and accounts for 50% of IE cases. It is important to be aware of the possibility of a spinal epidural abscess accompanying Streptococci viridans endocarditis. But in general, it could be treated by the conservative treatment. Conservative treatment is a good first line treatment in selected patients.