Differences in Cervical Sagittal Alignment Changes in Patients Undergoing Laminoplasty and Anterior Cervical Discectomy and Fusion
Article information
Abstract
Objective
Anterior cervical discectomy and fusion (ACDF) and laminoplasty (LP) are the most commonly performed procedures for degenerative cervical spondylosis. Cervical sagittal alignment (CSA) has recently been studied as an important predictor of clinical and radiological outcomes. The data from previous studies are insufficient for analysis using the recently designed CSA parameters, T1 slope (T1s), and T1s minus cervical angle (T1sCA).
Methods
We retrospectively collected data from patients who underwent ACDF and LP from January 2013 to May 2016. The CSA parameters included CA, sagittal vertical axis, T1s, and T1sCA. T1sCA values were used to evaluate the preoperative cervical balance (T1sCA>20°: imbalance). Clinical results were evaluated using the neck disability index (NDI) and recovery rate (RR) according to the Japanese Orthopedic Association scoring system.
Results
We analyzed the data of 72 patients (ACDF, n=39; LP, n=33). Imbalance on ACDF was associated with an increase in CA (balance: preoperative [PRE], 15.64° → follow-up [F/U], 15.74°, p=0.953; imbalance: PRE, −1.14° → F/U, 8.045°, p=0.008), whereas balance on LP was associated with a significant decrease in CA (balance: PRE, 16.26°→ F/U, 11.59°, p=0.009; imbalance: PRE, 5.36°→ F/U, 2.38°, p=0.249). No significant difference was found in the RR and NDI changes in the ACDF group based on balance, but a significant difference was found in RR in the LP group (balance: 61.65%±19.88%, imbalance: 46.90%±15.71%, p=0.046).
Conclusion
We found a significant difference in postoperative alignment in cases of ACDF and LP according to preoperative cervical sagittal balance. The postoperative clinical results of the LP group were more affected by F/U alignment than by the degree of alignment change.
INTRODUCTION
Interest in cervical sagittal alignment has been recently increasing because the preoperative characteristics of these factors can predict postoperative cervical alignment and clinical outcomes [1-3]. Because these parameters are of significance in predicting the changes that occur when the balance between gravity and force of extension from the posterior neck muscle is disturbed, these factors have been predominantly studied in laminoplasty (LP), a procedure that severely invades the posterior neck muscular-ligament complex [4-8]. Because anterior cervical discectomy and fusion (ACDF) does not damage the posterior neck muscular-ligament complex, studies regarding the influence of preoperative parameters are limited; however, several studies have focused on preoperative C2–7 cervical angle (CA) [9-12]. Recently, Kwon et al. [13] approached post-ACDF cervical alignment using T1 slope (T1s) and sagittal vertical axis (SVA). Further studies using preoperative parameters are expected to increase. The effect of the preoperative parameters of ACDF and LP on postoperative alignment and clinical outcome has been studied, focusing on the same disease group or similar levels [14-20]. However, these studies do not contain much of the new alignment parameters and concepts of cervical sagittal balance. In addition, the results of typical surgery (short level ACDF and multilevel LP) that are most commonly performed are rather unknown.
In this study, to evaluate the effect of preoperative sagittal parameters on typical cervical surgery, we aimed to evaluate the effect of preoperative sagittal parameters through comparison of radiologic clinical results of each operation, not a comparison of the 2 surgeries.
MATERIALS AND METHODS
1. Patient Population
1) ACDF group
Between January 2013 and May 2016, data from 76 patients who underwent ACDF for cervical spondylosis at a single institution were collected. The inclusion criteria were as follows: (1) patients who required surgery because of uncontrolled symptoms even after 6 weeks of treatment; and (2) 1- or 2-level ACDF using a stand-alone cage (n=54). The exclusion criteria were as follows: (1) patients whose T1S could not be measured (short neck, unable to maintain a routine standing position) (n=5); (2) patients with a history of previous cervical surgery (n=8); and (3) patients who underwent follow-up less than 1 year (n=2). Ultimately, we enrolled 39 patients and 53 segments for analysis. The ACDF was performed as follows. All patients underwent surgery using the standard Smith-Robinson anteromedial left-sided approach. We performed bilateral uncinated process resection, even in patients with unilateral symptoms, to eliminate remnant osteophyte regrowth. After complete decompression, a stand-alone PEEK cage (CORNERSTONE-PSR, Medtronic Sofamor-Danek, Memphis, TN, USA) was filled with demineralized bone matrix and applied under fluoroscopy. We attempted to position the cage in the anterior edge of the upper vertebra to prevent subsidence. After Caspar distractor release, a manual pullout test confirmed the stability of the segments. All patients were instructed to wear a soft collar for 2 months postoperatively.
2) LP group
We retrospectively reviewed the medical records of 64 patients who underwent open-door LP for cervical spondylotic myelopathy and ossification of the posterior longitudinal ligament between January 2013 and May 2016. The exclusion criteria were as follows: (1) less than three levels of LP (n=3); (2) with trauma, tumor, and infection (n=15); (3) patients whose T1S could not be measured (short neck, unable to stand) (n=6); and (4) patients who underwent follow-up less than 1 year (n=7). Finally, we enrolled 33 patients for analysis. The LP was performed as follows. All patients underwent expansive opendoor LP with a plate fixation system (CENTERPIECE, Medtronic Sofamor-Danek). If the stenotic lesion invaded the C2 or C7 level of the cervical spine, we carefully performed partial hemilaminectomy at C2 or C7 level. Postoperatively, all patients were instructed to wear a soft neck collar for 2 months, with the aim of preventing postoperative kyphosis.
3) Compliance With Ethical Standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of Institutional Review Board (IRB) of the Pusan National University Yangsan Hospital (approval number: 05-2018-013). The study protocol was approved by the IRB of Pusan National University Yangsan Hospital, which waived the requirement for informed consent due to the retrospective nature of this study.
2. Radiological Evaluation
All radiological assessments were performed at 1-month intervals by an independent observer who was experienced in spinal diseases. The mean values were calculated and used for statistical analysis. Lateral standing plain radiographs were obtained in patients in a neutral standing position facing forward at the following time points: preoperative (PRE), immediately after surgery, 7 days postoperatively (POST), every 3 months after surgery, and at the latest follow-up (F/U) examination. Lateral standing flexion/extension plain radiographs were obtained PRE and every 3 months starting at 6 months after surgery. We measured CA, SVA, and T1S using commercial software (Marosis 5.0, INFINITT Healthcare, Seoul, Korea) (Fig. 1), and described the measurement method applied in Table 1. Range of motion (ROM) was defined as the extension angle minus the flexion angle. Alignment of C2–7 CA≥0 was defined as lordosis. After the cervical spine compensated for the T1S by cervical lordosis, the additional angle required to restore the cervical sagittal angle to the horizontal line was defined as T1s minus CA (T1sCA) (T1sCA=T1s−CA) (Fig. 1). T1sCA values were used to evaluate the PRE cervical sagittal balance (T1sCA≤20°, balance; >20°, imbalance) [21].
Measurements of radiological parameters, including neutral lateral image (A), flexion lateral image (B), and extension lateral image (C). SVA, sagittal vertical axis; CA, C2–7 cervical angle; T1sCA, T1s minus CA; Flex, flexion.
3. Clinical Evaluation
Clinical evaluations included neck disability index (NDI) and modified Japanese Orthopedic Association (JOA) score [22]. The evaluations were performed PRE and POST and at follow-up. The recovery rate was calculated based on the following formula (Hirabayashi method): recovery rate (RR JOA) (%)=(POST JOA–PRE JOA)/(full score–PRE JOA)×100 [23].
4. Statistical Analysis
The Shapiro-Wilk test was used to confirm normality of the data (p>0.05). Data were presented as the number of subjects in each group or mean±standard deviation. Each independent variable was compared between the 2 groups using the independent-sample Student t-test, and by 1-way analysis of variance (ANOVA) for continuous variables. The Chi-square test and Fisher exact test were used for categorical variables. Pearson correlation analysis was used to investigate for relationships among CA, T1S, SVA, and T1SCA. We describe the strength of the correlation using the absolute value of r, as recommended by Evans [24]. Repeated-measures (RMs) ANOVAs were performed to investigate longitudinal trends. Multiple linear regression analysis was performed by stepwise method. Values of p<0.05 denoted a significant difference. All analyses were performed using IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA).
RESULTS
1. Patient Characteristics and Surgical Techniques
The LP group was significantly older than the ACDF group (LP, 60.94±11.66; ACDF, 51.08±9.40; p<0.001). Other variable, such as sex, body mass index (BMI), and F/U loss rates were not statistically significant. Operative levels and disease entity for each group are shown in Table 2.
2. Radiological Outcomes
1) Preoperative radiologic parameters for all patients
The distribution of CA, T1s, SVA, and ROM in all patients were 11.42°±9.96°, 27.07°±5.89°, 21.87±10.96 mm, and 38.37°±11.80°, which met the normal distribution by Kolmogorov-Smirnov test (p>0.05). The correlation analysis of cervical sagittal parameters with age was not statistically significant, except for the weak negative correlation of ROM (r=-0.286, p=0.02).
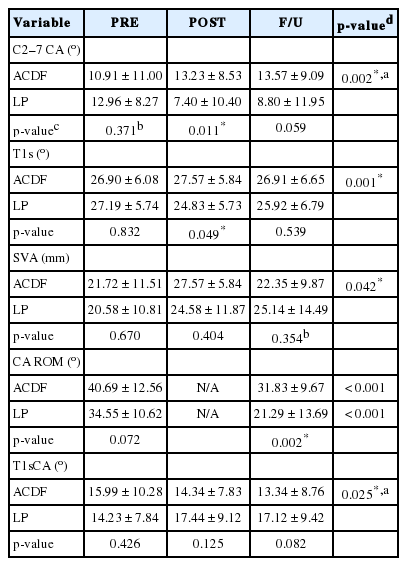
2) Comparative analysis of radiologic parameter between the ACDF and LP groups
The measured values of the cervical sagittal parameters of the 2 groups are summarized in Table 3. Independent t-test was performed for comparison between the 2 groups at each PRE, POST, and F/U time points. PRE: All parameters between the 2 groups were not statistically different. POST: CA, T1s showed a statistically significant difference (CA, p=0.011; T1s, p=0.049). FU: CA and T1sCA were close to statistical significance (CA, p=0.059; T1sCA, p=0.082), and CA ROM was significantly different (p=0.002). The result of RM-ANOVA is shown in Fig. 2. The longitudinal trend in all parameters were significantly different between the groups (CA, p=0.002; T1s, p=0.001; SVA, p=0.042; T1sCA, p=0.025). A paired t-test was performed to evaluate the difference between PRE-POST, and PRE-FU. For ACDF, PRE–POST SVA and PRE–FU ROM showed significant differences. In the case of LP, all measurements, except for PRE–POST T1sCA, showed statistical significance (Fig. 2). Paired t-test was performed based on cervical balance (PRE T1s-CA≤20°, balance; >20°, imbalance) for each group to evaluate the alignment change based on cervical balance (Figs. 3, 4).
The mean value of cervical sagittal alignment parameters (A, C2–7 CA; B, T1 slope; C, SVA; D, T1sCA) according to ACDF and LP. ACDF, anterior cervical discectomy and fusion; LP, laminoplasty; C2–7 CA, C2–7 cervical angle; SVA, C2–7 sagittal vertical axis; T1sCA, T1 slope minus CA; PRE, preoperative; POST, postoperative day 7; F/U, last follow-up image. *p<0.05, statistical significance according to time point.
The mean value of cervical sagittal alignment parameters (A, C2–7 CA; B, T1 slope; C, SVA; D, T1sCA) of ACDF according to balance (T1sCA ≤ 20°, balance; T1sCA > 20°, imbalance). ACDF, anterior cervical discectomy and fusion; C2–7 CA, C2–7 cervical angle; T1s, T1 slope; SVA, C2–7 sagittal vertical axis; T1sCA, T1 slope minus CA; PRE, preoperative; POST, postoperative day 7; F/U, last follow up image. *p < 0.05, statistical significance according to time point.
The mean value of cervical sagittal alignment parameters (A, C2–7 CA; B, T1 slope; C, SVA; D, T1sCA) of laminoplasty according to balance (T1sCA ≤ 20°, balance; T1sCA > 20°, imbalance). C2–7 CA, C2–7 cervical angle; T1s, T1 slope; SVA, C2–7 sagittal vertical axis; T1sCA, T1 slope minus CA; PRE, preoperative; POST, postoperative day 7; F/U, last follow up image. *p < 0.05, statistical significance according to time point.
(1) Balance ACDF group: A significant increase was found in SVA POST, but decreased at FU. No statistical significance was found between PRE–FU SVA. (2) Imbalance ACDF group: CA and T1sCA significantly changed in POST, and these changes persisted in F/U. (3) Balance LP group: CA, SVA, and T1sCA significantly changed in POST, and these changes persisted in F/U. (4) Imbalance LP group: T1s decreased significantly in POST, but in FU, and no significant difference was found with PRE.
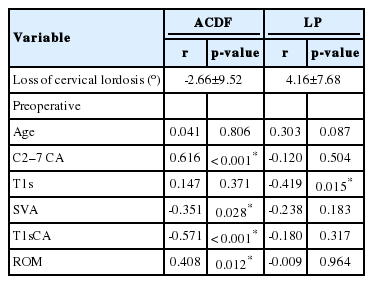
3) Correlation analysis for loss of cervical lordosis
We evaluated a correlation analysis for continuous variables to analyze factors affecting loss of cervical lordosis (PRE-CA minus F/U-CA). In the ACDF group, loss of cervical lordosis was related to PRE-CA, PRE-SVA, PRE-T1sCA, and PRE-ROM, and was unrelated to age and T1s. In the LP group, T1s has a significant correlation with loss of cervical lordosis (r=-0.419, p=0.015), but all other factors were not significant (Table 4).
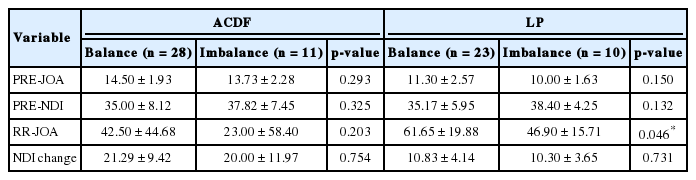
3. Clinical Outcomes
In the ACDF group, the PRE-JOA and PRE-NDI were 14.28±2.04 and 35.79±7.94, respectively, and were improved to 15.72±2.15 and 15.03±9.91 after surgery, respectively. No statistical significance was found in the Spearman correlation analysis between clinical improvement and preoperative radiologic parameters and postoperative parameter changes. We assessed the effect of cervical balance on clinical outcome, and no difference was found in RR JOA and NDI change between the 2 groups (Table 5).
In the LP group, PRE-JOA and PRE-NDI were 10.91±2.38 and 36.15±5.63, respectively, and were improved to 14.73±2.07 and 25.21±5.06 after surgery, respectively. Spearman correlation showed that RR JOA was significantly correlated with PRE-CA (r=0.362, p=0.038), F/U-CA (r=0.473, p=0.005), and F/U-T1sCA (r=-0.509, p=0.002). The cervical balance showed a significant difference in the clinical outcome in the LP group. RR JOA in the balance group (61.65%±19.88%) was significantly higher than that in the imbalance group (46.90%±15.71%) (p=0.046). NDI change did not show a significant difference (balance group, 10.83±4.14; imbalance group, 10.30±3.65) (Table 5).
DISCUSSION
ACDF and LP are the most common surgical methods for degenerative cervical spondylosis. The effect of LP is due to indirect decompression by posterior migration of the spinal cord from the anterior compression lesions [25,26]. In this respect, several studies found poor outcome in patients with preoperative kyphotic alignment [27-29]. Furthermore, postoperative kyphotic changes are also associated with poor outcome [4,30,31]. This postoperative kyphotic changes have also been reported in patients without preoperative kyphotic alignment [4], and recent studies focused on their association with T1s [2,5,7,8,32]. In patients with high T1s, the posterior neck muscular-ligament complex injury is associated with postoperative kyphotic changes, leading less posterior migration of the spinal cord [6].
The ACDF directly removes the anterior compression lesion and increases the height of the neural foramen, which also results in the indirect decompression [33]. However, graft failures, such as subsidence and pseudarthrosis have been reported frequently [12,34,35], which may diminish the effectiveness of indirect decompression and resulted in the recurrence of symptoms [35]. Our recent study reported that subsidence was associated with PRE T1s [36]. In addition, preoperative cervical alignment has also been reported to be associated with the clinical outcome of ACDF [37-39]. Kwon et al. [13] recently evaluated the relationship of preoperative radiologic parameters to postoperative SVA, which was known to be associated with clinical outcome [2,32]. With regard to the recognition of the importance of preoperative parameters in ACDF, we analyzed the effects of preoperative parameters on radiological and clinical outcomes in ACDF compared with LP.
The concept of preoperative cervical sagittal balance is evaluated by various factors. In existing literature, cervical sagittal imbalance was defined as T1s >40°, SVA>40 mm, and T1s-CA>20° [21]. In our study, no T1s>40° in both groups, and SVA>40 mm was also too small to obtain statistical significance (ACDF SVA>40 mm, 4 patients; LP SVA>40 mm, 2 patients). We compared the postoperative alignment differences based on each operation based on T1sCA>20°, and ACDF showed a significant improvement in alignment of the imbalance group and no significant change in the balance group (Fig. 3). In the LP balance group, alignment deterioration was prominent, whereas in the imbalance group, it was not significant (Fig. 4). However, these results do not mean that LP in the balance group results in worse outcomes. The loss of cervical lordosis (ΔCA) of the balance group is much larger than the imbalance group, but F/U CA of balance group still maintains a higher value than the F/U CA of the imbalance group (F/U CA: balance, 11.59°±10.67°; imbalance, 2.38°±12.79°; p=0.040). This result is similarly present in T1sCA (F/U T1sCA: balance, 13.70°±7.75°; imbalance, 25.01°±8.33°; p=0.001). Similarly, in the ACDF, the improvement of cervical sagittal alignment parameters in the imbalance group was significantly higher than that in the balance group, but the F/U values of these parameters were still higher in the balance group (F/U CA: balance, 17.74°±8.96°; imbalance, 8.05°±7.09°; p=0.015). This result shows that the cervical sagittal balance, which is a comprehensive result of preoperative factors, has different effects on the radiological results of 2 different surgical procedures.
What is interesting at POST is that T1s was significantly decreased in the imbalance LP group, and this change was slightly recovered in the F/U period (Fig. 4B). The imbalance group has high T1s and low CA. When LP was performed in these patients, additional decrease in CA occurred. We speculated that the additional decline of CA caused gaze disturbance. The patient attempted to recover gaze by changing the T1s (as a proxy of thoracolumbar curvature) to compensate the disturbance. Surely, to explain these changes, a large-scale study of whole spine images would be needed. We note, however, that our study suggests that the change in T1s is also an important parameter in the study of LP, and that T1sCA is a better representative of LP alignment than T1s alone.
Because our study is not based on the similar disease entities, we did not compare the clinical outcomes between the 2 surgical procedures. We analyzed the effect of preoperative sagittal balance and postoperative radiologic change on the clinical outcome for each surgical procedure. In the clinical results of the LP group, the RR JOA in the balance group was higher than that in the imbalance groups, despite a significant decline of CA occurring in the balance group. Based on the Spearman correlation analysis, RR JOA was correlated with PRE-CA, F/U-CA, F/U-T1sCA, but not with SVA and T1S. All delta values of CA, T1s, SVA, and T1sCA were also not correlated with RR JOA. In addition, our study demonstrated that F/U-T1sCA can better reflect the RR JOA than F/U CA. We assumed that the reason of F/U-T1sCA being more correlated with RR JOA than F/U-CA is because T1s also affected by the surgical procedure. In the case of ACDF, balance did not affect postoperative clinical outcomes.
This study has several limitations. First, this study is a retrospective small sized, non/-controlled study. Second, we did not limit the inclusion criteria to the same disease entity in comparing the two surgical procedures. Third, we did not include the various methods of ACDF and LP.
CONCLUSION
We found a significant difference in the postoperative alignment of ACDF and LP based on the preoperative cervical sagittal balance. Particularly, the imbalance ACDF group showed postoperative alignment improvement, but the balance LP group showed alignment deterioration. The postoperative clinical results of the LP group were more affected by F/U alignment than the change of alignment. Because T1s in LP is also a variable element based on surgery, we suggest that T1sCA is a more appropriate alignment evaluation factor.
Notes
The authors have nothing to disclose.