The Characteristics and Incidence of Posterior Apophyseal Ring Fracture in Patients in Their Early Twenties With Herniated Lumbar Disc
Article information
Abstract
Objective
Posterior apophyseal ring fracture (PARF) is a common disorder that may be accompanied by herniated lumbar disc (HLD) in patients in their early twenties. However, there are very few reports on PARF in this clinical context. The objective of this study was to identify the incidence and characteristics of PARF with HLD in this age group.
Methods
We surveyed patients who visited Armed Forces Busan Hospital between May 2017 and October 2017 and included those aged between 19 and 25 years who had HLD accompanied by PARF. We retrospectively collected their demographic characteristics, clinical manifestations, and radiological findings on computed tomography (CT) scans. We categorized the PARF lesions according to Takata’s classification.
Results
Of 140 HLD patients, 43 (30.7%) had PARF lesions with HLD. We found that the presence of a PARF lesion was significantly related to a severe pain score on the visual analogue scale for lower back pain and/or lower leg radiating pain (p=0.001). The most common level and location of PARF were L5/S1 (n=25, 56.8%) and the superior endplate of the S1 vertebra, respectively. Type 1, according to Takata’s classification, was the most common type of PARF in the patients (n=34, 77.2%).
Conclusion
We recommend that spinal surgeons perform CT scans to check for PARF lesions in all young patients in their 20s who present with severe radiating and lower back pain.
INTRODUCTION
Lumbar posterior apophyseal ring fracture (PARF) is generally an uncommon disorder reported in adolescents and young adults having low back pain and neural symptoms. This disease was specifically diagnosed in young athletes and confirmed by separation of bony particle at the posterior edge of the cephalad or caudal vertebral endplate where apophyseal ring and adjoining vertebral body had been completely fused. This fusion becomes complete between the ages of 18 and 25 years [1-3]. Many neurosurgeons have not been familiar with this disease and not everything about this disorder has been proved clearly. Therefore, there are only few articles about the incidence of this disorder some of which reported the incidence in all patients having herniation of the lumbar disc [4-6] while others appeared frequently in children and adolescents [7,8]. There are, however, no reports on its incidence in the age group of 18 to 25 years, when apophyseal rings and the adjoining vertebral bodies are not completely fused. Therefore, we studied the clinical and radiological features of PARF with herniated lumbar disc (HLD) in this age group.
MATERIALS AND METHODS
We examined the patients who visited Armed Forces Busan Hospital between May 2017 and October 2017 and shortlisted those aged between 19 and 25 years having HLD accompanied with PARF. All patients were soldiers, and they had similar level of physical labor intensity. We excluded the patients with other spinal diseases, such as spondylolysis, spondylolisthesis, idiopathic adolescent scoliosis, and spinal stenosis. The Institutional Review Board of Armed forces medical research institutes approved this retrospective study protocol (AFMC-17105-IRB-098).
1. Demographic Characteristics and Histories
We retrospectively surveyed the patients for age, history of trauma, and any athletic activities in the past.
2. Clinical Manifestations at Admission
At admission, we assessed the severity of subjective discomforts about lower back pain or radiating pain using the visual analysis scale (VAS) and checked those having weakness of lower extremity, hypoesthesia, and increased deep tendon reflexes. We performed straight leg raise (SLR) test on all patients with lower back pain or radiating pain.
3. Radiological Analysis
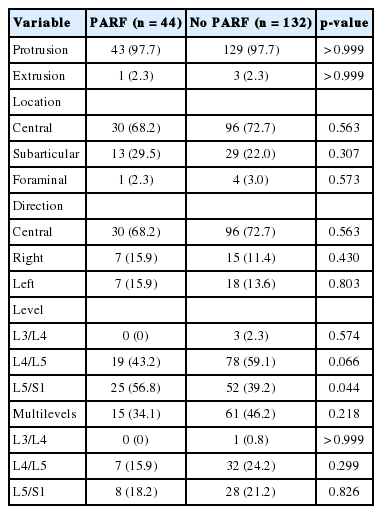
We reviewed the computed tomography (CT) scans (with continuous slices, no gap and 5-mm slice thickness) of all HLD patients. We classified the degree and location of HLD according to lumbar disc nomenclature: version 2.0 of North American Spinal Society and used Takata et al. [3] classification to subdivide findings in patients with PARF. In this classification, there are three types in computed tomographic morphology. The type 1 is simple separation of posterior vertebral endplate not containing the vertebral body, type 2 corresponds to an avulsion fracture of the posterior rim of vertebral body including the cartilage endplate of annulus fibrosus, and type 3 defined a small posterior vertebral body fracture larger than vertebral rim. One neurosurgeon and one radiologist crosschecked these findings, which were included in this article (Fig. 1).
Classification of posterior apophyseal ring fracture [22]. (A) Type 1, an arcuate simple avulsion of the posterior cortex of the endplate without osseous defect. (B) Type 2, an avulsion fracture of the central cortical and cancellous rim of posterior vertebra. (C) Type 3, a more lateral localized fracture involving a larger amount of the vertebral body, resulting that osseous defect anterior to the fragment is larger than the fragment. Arrow indicates the lesions of posterior apophyseal fracture.
4. Statistical Analyses
To ascertain factors associated with PARF, we used the chisquare test in all patients with HLD. The independent samples ttest and Mann-Whitney U-test were used to compare the average values amongst the patients with and without PARF. All statistical analyses were performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). All p-values <0.05 were considered statistically significant.
RESULTS
Of the patients visiting Armed Forces Busan Hospital, 140 were diagnosed with HLD, of which 43 patients had the associated PARF lesion (30.7%). Moreover, 176 HLD lesions were included in our study, of these, 44 lesions were accompanied PARF. Only male patients were included in our study, and the median age of each group showed similar results (with PARF: median age, 21 years; interquartile range [IQR], 20–22 years vs. without PARF: median age, 21 years; IQR, 20–21 years).
The characteristics of patients with PARF versus those without PARF are presented in Table 1. Amongst the clinical manifestations in each group, there was only one significant result in the severity of whole discomforts using VAS: median VAS 6 (4–7) in patients having PARF versus median VAS 4 (3–5) in patients without PARF. However, we did not find any significant statistical differences in other clinical symptoms. There were also no statistically meaningful results in neurological examination such as hypoesthesia, motor weakness of lower extremities, SLR test, and cauda equina syndrome. There were also no differences in past history of receiving trauma that patients have remembered such as fall down, traffic accidents, and blunt injury (20.9% vs. 15.5%, p=0.470) and the experience of athletes in young ages (7.0% vs. 9.3%, p=0.755).
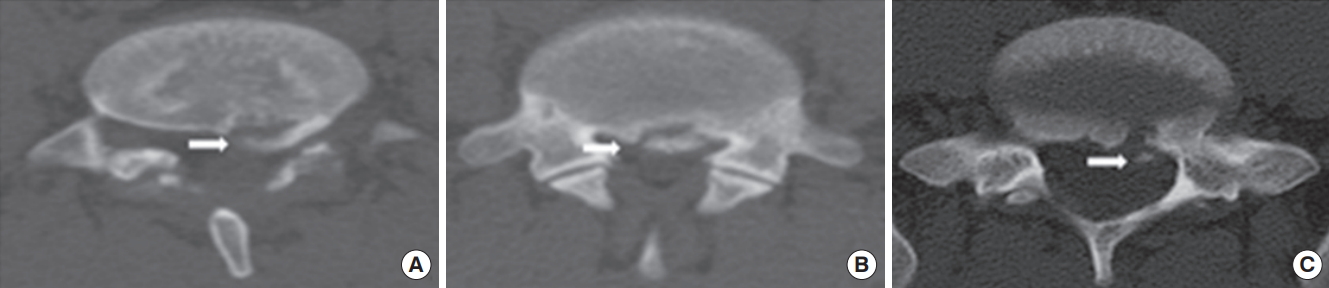
Table 2 shows differences in the radiological findings between each group. The ratio of protrusion to extrusion remained the same in each group. The locations and directions of ruptured particle in the spinal canal did not reveal significant differences in each group. In the group having HLD without PARF, the most common level was L4/L5 (78 patients, 59.1%) followed by L5/S1 (52 patients, 39.2%). In the patients with PARF, the lesion was accompanied with HLD at the same spinal level. The most common level with PARF was L5/S1 (n=25, 56.8%) followed by L4/L5 (n=19, 43.2%). The incidence of PARF in multilevel discs in each group did not show a meaningful result.
Table 3 exhibits the detail about superior or inferior endplate of each vertebra where PARF occurred and the result that the morphologies of PARF were divided by Takada’s classification. The locations of PARF were L4 inferior endplate in 4 patients, L5 superior endplate in 13, L5 inferior endplate in 6, and S1 superior endplate in 21. There was no patient who had multiple PARF lesion. According to Takata’s criteria, type 1 was the most common condition in PARF (n=34, 77.2%). In this type, the superior endplate of S1 was the most common site of occurrences (n=17, 50%). The second common type was type 2 (n=6, 13.6%), which mostly occurred at the superior endplate of L5 vertebra.
DISCUSSION
The epiphyseal ring ossifies between the age of 4 to 6 years and fuses completely before the age of 18 to 25 years [9] approximately. It is strongly attached to the annulus fibrosus by Sharpey’s fibers. The posterior longitudinal ligament wrapping the posterior part of vertebral body firmly holds onto annulus fibrosus. Consequently, the apophyseal ring is weakly joined to vertebral body; hence, PARF occurs. There are several hypotheses about the occurrence of PARF. Some authors have reported that sports trauma and injury such as weight lifting and falling caused the separation of apophyseal ring as they have frequently noted this condition in young athletes and patients with history of physical trauma [2,8,10-12]. Others revealed that repetitive extension is the mechanism of PARF. The large stress under this situation may damage and weaken the apophyseal ring in young ages and finally cause PARF, when it goes over the point that apophyseal ring physiologically endured [13,14]. The others reported that the pathogenesis of this disease is the degeneration of the intervertebral disc and cartilage [15,16]. We suggest the pathogenesis of this disease to be microtrauma and degeneration. In our reports, most patients with PARF had not been athletes and recalled the episode of recent trauma. Moreover, we did not find the radiological lesion associated with trauma. We noticed that all patients with PARF had HLD at the same level of vertebra.
Some authors have reported the incidence of PARF, but the results of these reports varied according to the patients’ age. In all ages, the incidence of PARF accompanied with HLD was 5.35%–8.2% [4-6]. Some revealed that the prevalence of PARF in children and adolescents was 5.8%–28% [7,8]. Scarfo et al. [16] reported that 11% of patients with HLD were diagnosed with PARF. In our reports, PARF lesion was diagnosed in 43 patients with HLD, who were in their young twenties (30.7%). The difference in incidence was caused by the fact that PARF cannot be easily detected on plain radiograph and magnetic resonance imaging (MRI) [17,18]. Moreover, the other reason of this difference was that many spine surgeons were unfamiliar with this lesion and confused it with ossification of posterior longitudinal ligament, calcified intervertebral disc, and degenerative osteophytes. The report of Martínez-Lage et al. [8] and our reports noticed that the incidence in patients with unfused apophyseal ring was higher than that in adults. Our reports showed the highest incidence of PARF in these articles about the incidence of PARF; so, the incidence of this disease is expected to increase until 25 years old when apophyseal ring is completely fused.
The most common symptoms of PARF are lower back pain with or without radiating pain due to nerve root irritation [5,7,15,17,19]. Other symptoms are paravertebral muscle spasm and tenderness, the decreased motor power in lower extremity or/and sensory defect, and loss of deep tendon reflexes according to the affected nerve. However, cauda equina syndrome is a rare symptom in the patients with PARF [5,15]. In our study, the most common manifestations of PARF were lower back pain and radiating pain. Neurological defects such as weakness of lower extremity, sensory defects, and caudal equina syndrome were rare. The positive ratio of SLR test in PARF patients was similar to that in the patients with HLD alone. In contrast, the patients with PARF had more severe pain than those with HLD alone. The report of Chang et al. [7] showed the same result regarding the symptoms of patients having PARF being more painful. We supposed that separated osseous particles in PARF caused the severe pain in these patients.
CT was the best modality to diagnose and recognize the size, shape, and location of fracture (Fig. 2). Almost all the authors diagnosed PARF and its associated characteristics using a CT scan [20]. Additionally, CT scan was the best way to distinguish calcified HLDs and particles of fracture. However, MRI is a less precise method of diagnosing PARF because it is difficult to differentiate the bony fragment from the disc or ligament that also presented with low signal intensity (Fig. 3). In terms of sensitivity, CT scan was a better method than MRI because MRI only identifies 22% of lesions [17].

Computed tomographic axial image (A) and sagittal reconstruction image (B) represent a small fracture fragment located at superior endplate of sacrum. Arrow indicates the lesions of posterior apophyseal fracture.
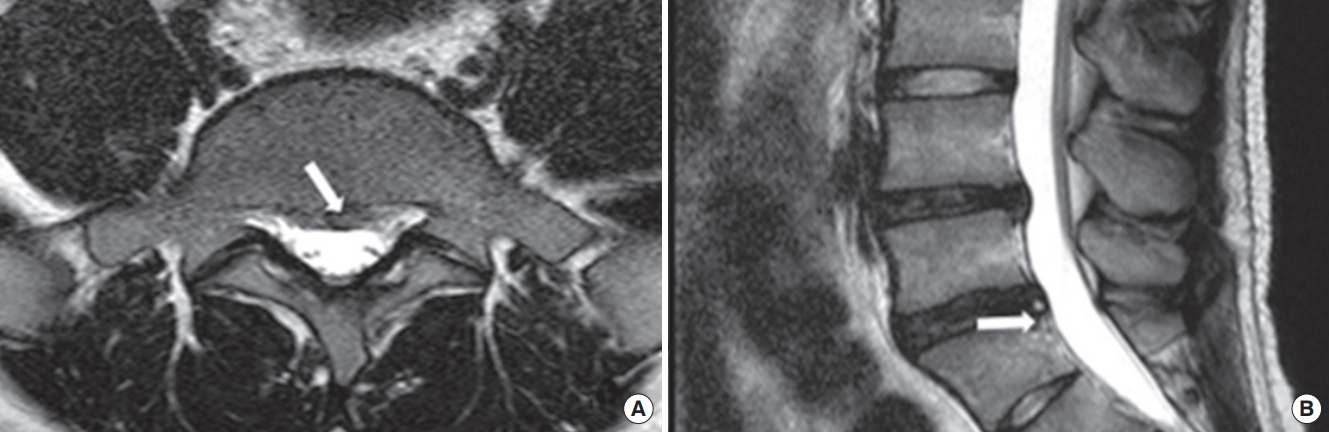
Theses magnetic resonance images showed the lesions of posterior apophyseal fracture. We could not exactly distinguish between the lesions of posterior apophyseal ring fracture and ruptured disc particles on these images. Arrow indicates the lesions of posterior apophyseal fracture.
The most common site and level of PARF are controversial. Some authors reported that L4/L5 level was the most common level of PARF with HLD in adolescents and L5/S1 in young adults [3,21-23]. Other researchers presented that PARF occurred at L5/S1 level mostly in all people [5,15,22]. All reports about the site of PARF showed that the S1 superior endplate was the most commonly affected site [15,24]. Our study also revealed that L5/S1 level and S1 superior endplate were the most commonly affected sites. According to some reports including ours, the posterior part of superior vertebral endplate is a more frequently affected site than the lower endplate because the superior endplate of vertebral body was the most stressful site from functional point of view [8].
The widely used classification of PARF is Takada’s classification [3]. This method divides PARF into 3 types according to the morphology of fracture. The type 1 is simple and thin avulsion fracture of posterior vertebral endplate that does not contain the vertebral body. It has been reported that children under 13 years of age are mostly affected by this type. The type 2 is a large and thicker avulsion fracture of the posterior rim including the cartilage endplate of annulus fibrosus and is found in children over 13 years and in adolescents. Type 3 defines a small posterior vertebral body fracture larger than the vertebral rim. These fractures are found more frequently in the young adults older than 18 years. We enrolled the patients with PARF aged between 19 and 25 years, so we predicted that type 3 was the most common type in our study, according to this report. However, the most common type in our report was type 2. For the Takata’s classification is based on small groups including 29 patients and 31 fractures, so it is assumed that this difference about most common type in these age would have occurred. Other classifications are also based on small groups or retrospective review. So we suggested that the spinal surgeons should develop the systemic and faithful classification using prospective studies in large groups.
CONCLUSION
Our study shows that the adults in early twenties have the highest incidence of PARF. The adults having PARF in their early twenties present with severe lower back pain and radiating pain than those with HLD alone. CT scan is the best way to identify this condition. Thus, we recommend that the spinal surgeons should perform a CT scan for all patients, in their young twenties, with severe radiating pain and/or lower back pain and multiple HLD lesions in patients’ MRI.
Notes
The authors have nothing to disclose.