Factors Associated With Longer Postoperative Outpatient Follow-up Duration in Patients With Single Lumbar Disc Herniation: A Noncomplicated Patient Cohort Study
Article information
Abstract
Objective
Many reports have described the outcomes of surgical treatment of lumbar disc herniation (LDH). However, few reports have investigated the treatment period after lumbar disc surgery. If no complications occur, how long should an ordinary patient be treated? Which factors are associated with the outpatient follow-up period (OFP)? To answer these questions, we reviewed the medical records of patients who underwent lumbar disc surgery, calculated their average OFP, and sought to identify factors associated with the OFP.
Methods
Patients who underwent surgical treatment of single-level LDH from July 2005 to December 2011 were enrolled in this study. Patients who had no pain or required no further treatment did not receive follow-up. Patients’ medical records were reviewed retrospectively. Cases of recurrent LDH, postoperative infections, instrumentation, cauda equina syndrome, postoperative hematoma, trauma-associated herniation, and spondylolisthesis were excluded. We reviewed the postoperative hospitalization period (PHP) and the OFP. Sex, age, operation year, surgical approach, the operating surgeon, disc level, and insurance type were investigated as associated factors.
Results
In total, 611 patients underwent surgical treatment for single-level LDH by 4 surgeons. Their average age was 44.3 ± 15.1 years. There were 377 male and 234 female patients. The average PHP was 4.4 ± 3.2 days, the average OFP was 112.3 ± 198.6 days, and the 95% confidence interval for the OFP among the enrolled patients was between 96.5 and 128.1 days.
Conclusion
Although this is a single-institute report, most LDH patients showed an OFP of less than 4 months after surgical treatment. In this study, sex, age, and insurance type seemed to be related with the OFP.
INTRODUCTION
Lumbar disc herniation (LDH) is a common disease, and extensive information about LDH is available online. Patients affected by LDH can learn about many related topics, such as the symptoms of LDH, its prognosis, and rehabilitation after surgery. Nonetheless, the widespread information available about LDH is still not sufficient to answer all questions that a patient might have.
One such question is how long a patient will be treated conservatively, and another is how long postoperative treatment will last. Without answers to these questions, patients with LDH may have difficulties making preoperative or postoperative plans. However, if we can give patients information about the length of treatment, they can estimate how long they will have to be absent from work and make plans about travel or important ceremonies, such as weddings.
The authors of the present study assumed that doctors can straightforwardly discuss operative plans with patients and that patients can make their own plans accordingly. Therefore, we investigated the outpatient follow-up period (OFP) of patients who underwent surgery for single-level LDH without complications. Using the results of this study, the length of postoperative treatment can be estimated, which could be valuable to medical service providers and their patients.
MATERIALS AND METHODS
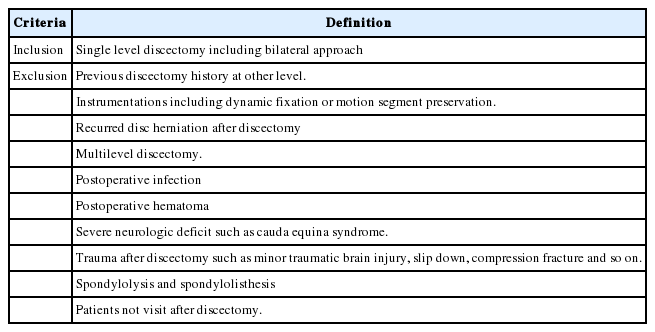
This study was a single-institutional retrospective study conducted in Gangwon Province, Korea. The patients lived in an urban-rural complex city. The medical records of patients who underwent surgical treatment for LDH from 2005 to 2011 were reviewed, and those with single-level LDH were enrolled. Patients with a normal postoperative course were included, and patients with complications were excluded. The inclusion and exclusion criteria are shown in Table 1. Patients who had no pain or required no further treatment did not receive follow-up.
After analyzing patients’ medical records, the preoperative symptom duration, postoperative hospitalization period (PHP), and OFP were measured. Repeated visits within 6 months after discharged were included in the OFP, while visits after 6 months were not.
Associations between the OFP and demographic, clinical, radiological, and socioeconomic factors were evaluated. The demographic factors included sex, age, and the operating surgeon. The clinical factors included the preoperative conservative treatment period, the presence of motor weakness, and the surgical approach (e.g., midline microdiscectomy, paramedian microdiscectomy for foraminal LDH, and percutaneous endoscopic lumbar discectomy). The radiological factors included the disc location (level), disc degeneration (Pfirrmann grade [1]), and severity of root compression [2]. Insurance type was used as a proxy for socioeconomic factors, instead of direct measures of occupation, educational level, and income.
A descriptive statistical analysis was conducted of the PHP and OFP. To compare men and women, t-test and chi-square test were used. One-way analysis of variance and the Pearson correlation coefficient were used to analyze the effects of other variables.
The study protocol was approved by the Institutional Review Board (IRB) of Hallym University Chuncheon Sacred Heart Hospital (approval number: 2014-61). Informed consent was waived by the IRB.
RESULTS
Of the 1,750 patients who underwent spinal surgery from 2005 to 2011, 611 were enrolled in this study. The average age at the time of surgery was 44.3±15.1 years old. There were 377 men and 234 women. The average PHP was 4.4±3.2 days, the average OFP was 112.3±198.6 days, and the 95% confidence interval of the OFP of enrolled patients was between 96.5 and 128.1 days.
1. Demographic Factors and Socioeconomic Factors
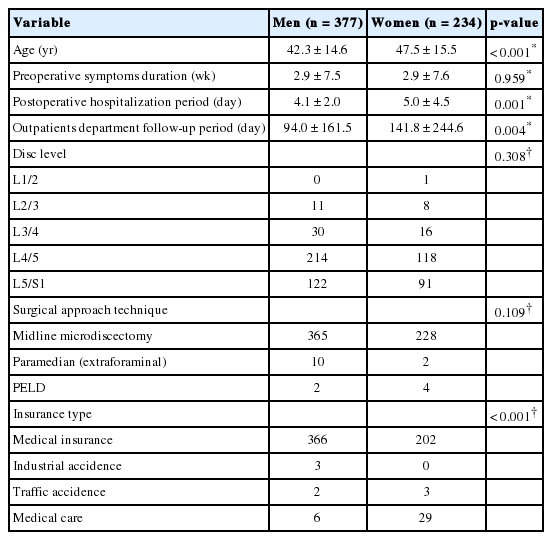
There were 377 men and 234 women, and many findings differed significantly between men and women (Table 2). Men were younger than women (p<0.001), and showed a shorter PHP (p=0.001) and OFP (p=0.004) than women. The average OFP and the corresponding 95% confidence interval for each age group (defined by decade) and sex are shown in Table 3. Preoperative symptom duration, surgical disc level, and surgical technique did not affect the OPF in either sex.

Average outpatients department follow-up period (day) and 95% confidence interval of each decade and sex
Age showed significant relationship with the OFP. In both sexes, older patients showed a longer OFP than younger patients (Table 3).
The PHP and OFP varied according to insurance type (Table 4). Only 3 patients had experienced an industrial accident, while 5 had experienced a traffic accident. The PHP of traffic accident patients was longer than that of other patients (p<0.001). The OFP of patients who had experienced an industrial accident was longer than that of other patients. The OFP of patients covered under the national health insurance program was shorter than that of patients who had experienced an industrial or traffic accident and those covered under Medical Aid.
2. Clinical Factors and Radiological Factors
The surgical level, surgical approach, severity of root compression on magnetic resonance imaging, presence of motor weakness, and severity of motor weakness were reviewed. The PHP and OFP showed no significant relationships with any of those factors (Table 5).

Results of analysis of variance according to the surgical level, surgical technique, root compression, and motor weakness
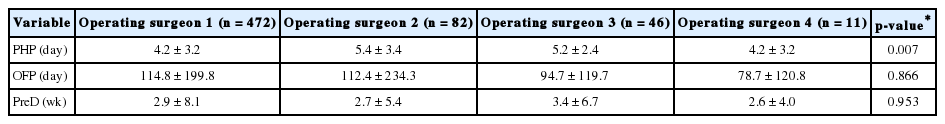
The operating surgeon influenced the PHP. There were 4 operating surgeons, whose patients showed significantly different PHPs (p=0.007). However, the operating surgeons did not influence the OFP or preoperative duration after symptom onset (Table 6).
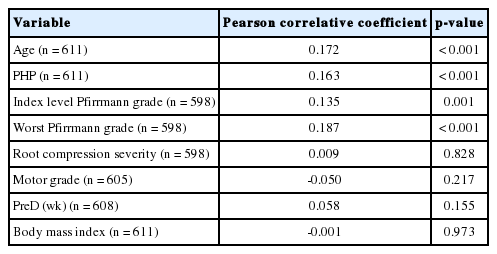
Age, the PHP, and the disc degeneration grade showed significant correlations with the OFP (Table 7).
DISCUSSION
LDH is common spinal disease that frequently affects young and middle-aged patients [3]. Therefore, it is important to provide patients with appropriate information about the disease, including treatment options, prognosis, the side effects of treatment, and especially the length of treatment, which includes the OFP. We conducted this study to obtain basic information about how the treatment of LDH is related to the OFP, which can be used to counsel patients with LDH.
In this study, the average OFP was 112.3 days. According to the literature on LDH surgery, most of the symptoms usually improve, but some patients have back pain or leg sensory abnormalities, and some must undergo reoperation due to recurrence. Whereas previous studies have examined dozens of patients, the present study included approximately 600. The purpose of this study was to measure the OFP, and we therefore did not investigate the clinical course of these patients. However, the outcomes of surgery were not significantly different from those reported in the existing literature [4-7]. The results of the present study are only applicable if LDH therapy is not defined as an asymptomatic postoperative period. Many patients present with residual symptoms after LDH surgery, but do not require medication. In the authors’ opinion, this study presents valuable information that can be used as an empirical guideline for the approximate length of treatment after the surgical treatment of LDH. Although no new theory or paradigm was articulated in this study, our findings may nonetheless be useful for treating patients.
The male patients in this study were younger than the female patients and showed a shorter PHP and OFP. This age discrepancy was most likely due to sex-related lifestyle differences. In addition, it has been reported that women who underwent LDH surgery had worse underlying symptoms than men [8]. Several previous studies have reported differences between men and women in the results of LDH surgery [9-11]. Sex differences in outcomes have also been observed in the elderly [12]. It is likely that male patients usually have more muscle, which could affect the results. Rahme et al. [9] reported that female sex and lack of exercise were poor prognostic factors for LDH surgery. In general, female patients exercise less than male patients. In some studies, rehabilitation has been found to improve the results of surgery [13]. Therefore, a relative lack of muscle mass and infrequent exercise could help explain the difference in outcomes between men and women. Although the OFP was not associated with clinical outcome, it is noteworthy that women had longer OFPs.
We compared the OFP according to insurance type. Although the results showed statistical significance, we do not think they are conclusive due to the insufficient number of patients. Nonetheless, it remains possible that insurance type, as a proxy for socioeconomic status, could affect the OFP in patients in South Korea. For instance, a previous study reported a difference in the length of hospital stay after gastrectomy for gastric cancer according to medical insurance status in the Republic of Korea [14]. No reports have investigated the relationship between OFP and insurance status. In this study, since medical insurance status reflected patients’ socioeconomic status, it is likely that the preoperative and postoperative period and OFP were related to medical insurance status.
The findings of this study reflect patients’ natural postoperative course after LDH surgery. This study included 5 cases of traffic accidents, 3 cases of industrial accidents, and 35 cases of patients who received Medical Aid, but these numbers are much smaller than the number of patients who were covered through the national health insurance system (568 patients). The average OFP of the patients covered through the national health insurance system was 98 days, and we think that this result is meaningful.
Medical environments and systems differ from country to country. In some countries, the appointment success rate, referral rate, and wait time of LDH patients vary depending on the type of medical insurance they have [15]. Due to differences in hospital accessibility and the appointment success rate, the OFP is likewise expected to show variation according to the health care system.
In this respect, the findings presented in this study regarding the OFP after LDH surgery may not be absolutely accurate in terms of reflecting purely medical considerations, rather than issues of access to care. However, South Korea was ranked 23rd of 195 countries in a study of health care access that presented a quality index based on the degree to which countries were amenable to personal health care [16]. Although this disease is unique, our findings on the OFP after LDH surgery are significant given the relatively high appointment success rate and medical accessibility of the Republic of Korea.
As discussed above, we defined the length of treatment as similar to the OFP. Therefore, we reviewed the literature to identify articles on this topic, and found no previous studies that investigated the OFP after LDH surgery. We suggest that it could be useful to conduct studies of the OFP after various treatments, because doing so would help medical service providers advise patients about the duration of treatment.
LDH occurs more frequently in younger patients, who are economically active [17]. Therefore, providing such patients with information about the length of treatment would help them make decisions about when to undergo an operation and how long to plan on being absent from work. Furthermore, it would be helpful to research the exact timing of return to work and to analyze possible effects of the type of occupation on return to work.
CONCLUSION
Although this was a single-institution report, most LDH patients showed an OFP of less than 4 months after surgical treatment. In this study, sex, age, and insurance type were found to be related to the OFP. More studies should be conducted of the OFP and the length of time needed before return to work in order to provide patients with appropriate guidance before undergoing surgery for LDH.
Notes
The authors have nothing to disclose.