Treatment of Odontoid Type II Fractures in Octogenarians: Balancing Two Different Treatment Strategies
Article information
Abstract
Objective
Demographic changes have led to a higher incidence of C-2 fractures, especially in elderly patients. For patients with type II fractures, treatment remains controversial, as discussed by Anderson and D’Alonzo, due to the rising morbidity and mortality rates for any treatment. The aim of this study was to compare conservative and surgical management in patients with type II C-2 fractures regarding outcomes, complications, and the mortality rate.
Methods
A retrospective analysis was performed of the medical records, X-rays, and/or computed tomography scans of patients ≥80 years of age with type II fractures who were admitted to our Department of Neurosurgery between January 1990 and December 2017. The success of treatment was evaluated 3 months after surgery.
Results
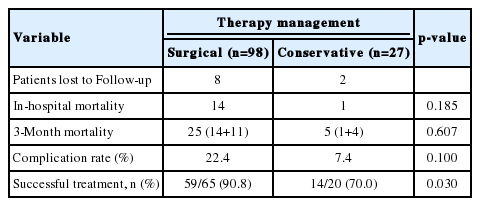
In total, 125 patients were included, of whom 98 were treated surgically and 27 were treated conservatively. Surgical treatment was successful in 90.8% of cases, while conservative treatment was successful in 70.0%. The in-hospital mortality was 14.29% and the 3-month mortality was 27.8% in the surgical group, compared to 3.7% and 20% in the conservatively treated group. The in-hospital complication rate was 22.4% in the surgically treated patients and 7.4% in the conservatively treated patients.
Conclusion
Surgical treatment of type II fractures seemed to be associated with higher success and complication rates than conservative treatment. Nevertheless, 3-month mortality was comparable in both groups. Therefore, we conclude that surgical treatment for type II fractures in elderly patients is superior to conservative management, although conservative treatment remains a valuable option in elderly patients with severe comorbidities.
INTRODUCTION
Odontoid fractures contribute to 9%–15% of all cervical spine injuries [1]. Type II fractures according to Anderson and D’Alonzo [2] are the most common type of C-2 fractures (up to 65%–74%). In the younger population (20–30 years of age), they account for 38%–46% of the fractures [3,4] and in the elderly population (70–80 years of age), even for 82%–95% [5-7].
The United Nations analyzed the demographic change in the population. In 2015, 1 in 8 people worldwide was aged >60 years. By 2030, this age cohort is projected to account for 1 in 6 people globally, and in 2050, 1 in every 5 people will be aged >60 years [8].
This will also lead to a rising incidence of cervical spine fractures, especially C-2 fractures [9].
As a matter of fact, comorbidities in elderly patients are common and, therefore, the peri- and postoperative risk for complications rises. Associated risk rates for the surgical treatment of odontoid fractures have been published before [10,11].
Up to date, general guidelines for the treatment of the type II fracture are still a subject of great controversy despite numerous studies on this topic. Operative treatment for type II fractures includes anterior stabilization with 1 or 2 odontoid screws, anterior transarticular screw fixation, or different approaches for posterior fusion. The conservative management of odontoid fractures requires an external immobilization with either a rigid cervical collar or a halo thoracic vest [12-14].
In the present study we conducted a retrospective single center analysis of a large cohort of elderly patients suffering from odontoid fractures classified type II according to Anderson and D’Alonzo to assess the superiority of one treatment method over the other.
MATERIALS AND METHODS
1. Including and Excluding Criteria
We included all consecutive patients with type II fractures classified according to the Anderson and D’Alonzo classification who were admitted to the Department of Neurosurgery, University Hospital Essen between January 1990 and December 2016. Medical records and computed tomography (CT)-scans of the cervical spine of 125 elderly patients, who were ≥80 years of age (mean age, 85.7±4.2 years; 30 males and 95 females), were retrospectively analyzed. Patients were excluded if: (1) age at the treatment was <80 years; (2) concomitant abnormalities of the C-1 and C-2 were found; (3) metastatic or rheumatoid disease may have caused the C2-fracture. Patients demographics are summarized in Table 1.
The study has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) and was approved by the Institutional Review Board (IRB) of Medical Faculty, University of Duisburg-Essen (registration number: 18-8049-BO). Individual informed consent from each patient was not required by the IRB due to the retrospective nature of this study.
2. Evaluation of the Fracture
Fractures were identified by thin multislices section CT-scan of the cervical spine (n=99) or, in the early 1990s, by anterior/posterior-fluoroscopy of the dens (n=26) and classified according to the Anderson and D’Alonzo classification [2].
3. Evaluation of the Physical Status of the Patient
The American Society of Anesthesiologist physical status classification (ASA-Score) was used [15] to evaluate the physical status of all patients and to determine the intraoperative risk.
4. Follow-up Examination of the Patients
Routine follow-up examination of the conservatively treated patients including CT-scan of the cervical spine, or anterior/posterior-fluoroscopy of the dens in the early 1990s, was performed after 4 and 12 weeks to assess bony consolidation.
Routine investigation of the surgically treated patients included a postoperative CT-scan of the cervical spine or a postoperative anterior/posterior-fluoroscopy of the dens assessing the alignment of the fracture and the osteosynthesis materials. Routine follow-up examination of the patients was performed 12 weeks after surgery.
5. Outcome Criteria
Successful conservative treatment was defined as bony consolidation of the fracture with restored alignment of the odontoid process after 12 weeks.
Surgical treatment was considered successful if: (1) the postoperative imaging showed good alignment of the fracture and the implants and (2) bony consolidation of the fracture was observed in the follow-up CT-scans, (3) the patient present pain-free and neurologically otherwise intact for the follow-up examination 12 weeks after surgery.
6. Statistical Analysis
All data were included into an electronic database “C2-fractures.” Analyzes of the data was performed using IBM SPSS Statistics ver. 23.0 (IBM Co., Armonk, NY, USA). Metric data were described by mean and standard deviation and nominal data by frequency and valid percent. Data was analyzed using the Fisher exact test for dichotomous variables. A p-value <0.05 was considered significant.
RESULTS
1. Patients
Urgent surgery was indicated in 98 of 125 patients (24 males and 74 females; mean age, 85.5±4.2 years) due to the radiological presentation of the C-2 fracture (lateral or posterior displacement of the fracture, dehiscence of the fracture greater than 5 mm), or because of associated neurological deficits. Therefore, 27 of 125 patients (6 males and 21 females; mean age, 86.5±4.3 years) were treated conservatively using external immobilization with a rigid collar in 26 patients or a halo thoracic vest in 1 patient (Table 1).
2. Patient’s ASA-Score
Patients treated with surgery showed a mean ASA-Score of 2.78±0.71 compared to a mean ASA-Score of 3.15±0.66 (Table 1). The ASA-Score did not differ significantly in both groups (p=0.016).
3. Treatment Regime of Type II Fracture
Of 125 patients, 58 were treated surgically by anterior odontoid screw fixation, another 7 underwent anterior transarticular screw fixation. Posterior fixation using C0–C3/4 stabilization with screws and rods was used in 11 cases. Seventeen cases were stabilized using C1/2 fixation with wire and a polymethylmetacrylate interpolant and 5 patients were treated using Ransford-Loops. The later was mainly used during the 1990s and in the early 2000s. These days, anterior odontoid screw fixation, anterior transarticular screw fixation, and posterior screw fixation (C1–C2 or C0–C3/4, if required) are employed according to the individual situation.
Twenty-seven patients were treated conservatively by external immobilization (rigid collar: n=26; halo thoracic vest due to an accompanying instable C1/C2-fracture: n=1).
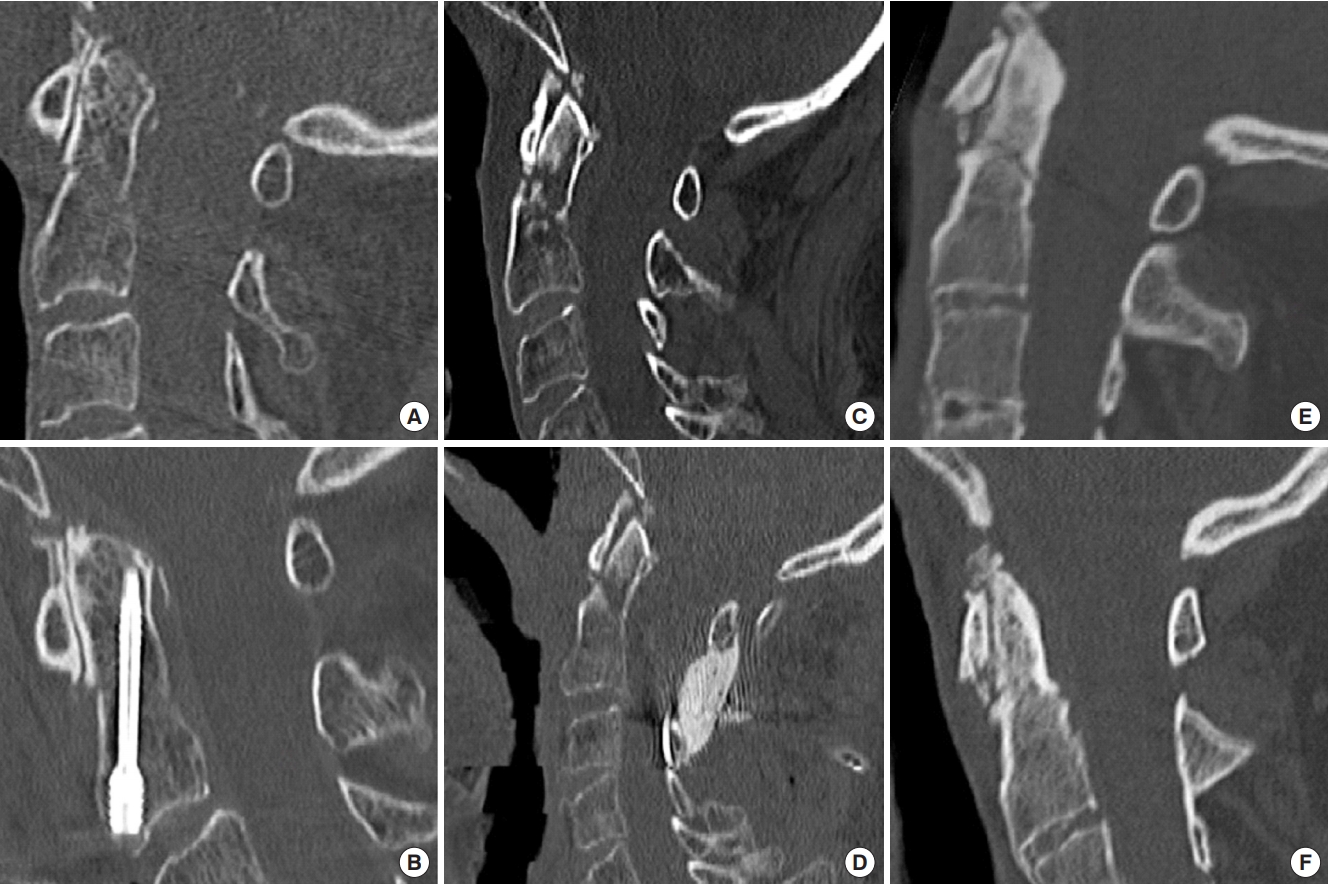
Cases illustrating the different treatment modalities can be seen in Fig. 1.
4. Follow-up Examination of the Patients
The routine examination was possible in 20 patients treated conservatively. Two patients were lost to follow-up and 5 patients died before the last follow-up examination.
A routine investigation of the surgically treated patients included a postoperative CT-scan of the cervical spine (n=72) or a postoperative anterior/posterior-fluoroscopy of the dens (n=26) assessing the alignment of the fracture and the osteosynthesis materials. Eight patients treated surgically were lost to follow-up and 25 patients died before the last examination. Therefore, 65 patients attended to the follow-up examination 12 weeks after surgery. Of those, 26 patients were completely pain-free and neurologically unremarkable at the follow-up examination. Due to this, additional CT-scans were discarded. In 39 cases an additional CT-scan of the cervical spine was performed at the follow-up examination due to persisting complaints to rule out fracture displacement or loosening of the osteosynthesis materials (Table 2).
5. Outcome
A successful treatment, after excluding the patients who were lost to follow-up (n=8) and those who died before the follow-up examination (n=25), was observed in 90.8% (n=59/65) of the surgically treated patients 12 weeks after surgery. In 6 patients, a screw loosening was detected before/at the follow-up examination due to persisting nuchalgia (Table 2).
A successful treatment was seen in 70.0% (n=14/20) of the conservatively treated patients after 12 weeks. Consequently, surgery was offered to them. Of these, 4 patients showed a successful consolidation of their fracture 3 months after surgery. Two patients refused to undergo surgery and remained with a stable pseudarthrosis. However, the difference between both treatment modalities was not statistically significant (p=0.03), presumably due to the low number of conservatively treated patients (Table 2, Fig. 1).
6. Complication Rate
Major intraoperative complications were observed in four of 98 patients (n=4/98 [4.1%]). Misplacement of a screw, detected in the postoperative CT-scan one day after surgery, occurred in 2 cases, leakage of cerebrospinal fluid in one case and skin incision due to the Mayfield-clamp in 1 case.
Postoperative complications were recorded in 21 patients (n=21/98 [21.4%]). Major complications were seen in 8 patients (n=8/98 [8.2%]) including: myocardial infarction (n=3), cardiac arrest with need for mechanical reanimation (n=2), bradycardia with the need of a temporary pacemaker (n=1), sepsis (n=1), and postoperative swelling of the larynx followed by percutaneous tracheotomy (n=1).
Minor complications (n=13/98 [13.3%]) included: pneumonia (n=8), pleural effusion (n=3) with the need for drainage (n=2), postoperative hematoma (n=1), and poor wound healing (n=1).
Thus, the overall complication rate (intraoperative and postoperative complications) was 22.4% (n=22/98; 3 patients suffered from intraoperative and postoperative complications).
In the conservative managed patient cohort, 2 patients suffered from pneumonia during the hospital stay, bringing the total complication rate to 7.4% (n=2/27).
There was no significant difference using Fisher exact test between the complication rates (p=0.100) (Table 2).
7. Mortality
The in-hospital mortality was as high as 14.3% (n=14/98) among the surgically treated patients, and 3.7% (n=1/27) among the conservatively treated. Circumstances leading to death of the patients included heart failure, pneumonia or unfavorable postoperative clinical status of the patient falling under the declared will of the patient regarding a limitation of therapy (Table 2).
Three-month mortality rose to 27.8% (n=25/90) for the surgically treated patients and reached 20.0% (n=5/25) for the conservatively treated patients. Cardiopulmonary distresses remained the leading cause of death within 90 days. There was no significant difference between both groups using Fisher exact test (in-hospital mortality rate: p=0.185; 3-month mortality rate: p=0.607) (Table 2).
DISCUSSION
C2-fractures due to falls are the most common injuries of the cervial spine in the elderly. The demographic change with an aging population will increase the incidence of those fractures [16]. While a general consensus on the treatment of type I- and type III-fractures according to the Anderson and D’Alonzo classification has been established, this consensus lacks in the approach of odontoid fractures [13,17].
Type I fractures can be treated safely conservatively using a rigid collar for immobilization of the cervical spine over a 6–8 weeks period of time. Type III fractures may be treated conservatively, too, employing a halo thoracic vest or a rigid collar over the same period [13,17]. A recently published study showed that treatment with either a halo thoracic vest or the rigid collar is associated with similar rates of healing, opening the discussion whether the higher rate of morbidity using a halo thoracic vest may be outweighed by the equal success rate especially in elderly patients [14].
Treatment of type II fractures has been a subject of intense research over the past decades, nevertheless is still a matter of great controversy. The different treatment options, especially the different surgical approaches, should be individually tailored based on the age, fracture pattern, presence of associated injuries and comorbidities of the patient [18,19]. Bearing in mind, that the aging population remains their activity of daily living for much longer than it used to have 30 years ago, this new agility has to be taken into account when counseling the patient. Likewise, a cumulation of comorbidities is to be respected in the choice of treatment.
Factors predisposing to failure of conservative management of type II fractures include age [5,12,20], posterior displacement of the fracture [21], fracture distraction [22], lateral displacement on the posterior radiograph [22], displacement greater than 4 mm [5,12,21] and a delay in treatment [22]. Nevertheless, conservative treatment by external immobilization may be referable in elderly multimorbid patients with increased anesthetic risk [23,24].
In our single center analysis, conservative treatment warranted bony consolidation of the fractures in 70.0% (n=14/20) of the octogenarians, whereas a surgical management led to fracture healing in up to 90.8% (n=59/65). Nevertheless, the complication rate (7.4%; n=2/27) vs. 22.4% (n=22/98) as well as the in-hospital mortality rate (3.7% [n=1/27] vs. 14.3% [n=14/98]) were markedly lower for conservatively managed patients during their in-hospital stay. However, the complication rate (p=0.100) and the in-hospital mortality rate (p=0.185) did not differ significant (Table 2). This result might be biased due to the small number of cases analyzed. This effect was maintained at the 3-month follow-up (mortality rate in the nonsurgical vs. surgical group: 20.0% [n=5/25] vs. 27.8% [n=25/90]). Again, there was no significant difference between both groups (p=0.607) (Table 2).
Schoenfeld et al. [11] found an increase of the mortality rate after surgery for patients over 85 years of age. The 3-month mortality rate was 21%, (6% mortality for patients aged 65 to 74 years [group I], 18% mortality for patients aged 75 to 84 years [group II], and 34% mortality for patients aged 85 years or older [group III]). After 1 year, the mortality in their study raised naturally over all subgroups with 21% for group I, 29% in group II, and 45% in group III, respectively. The data are in concordance to our findings.
We assume that the higher in-hospital mortality rate in the surgically treated group (14.29% vs. 3.7%) is driven by the burden of the operation and the accumulated risk of complications.
Complication rates in our study are in line with other studies showing similar rates of complication and mortality [25-27]. Smith et al. [27] analyzed the complication rate and the mortality rate in conservatively and surgically treated patients (mean age: 85.5±3.5 years) suffering from type II fractures. They observed a complication rate in the surgically treated group of 62% compared to complication rate of 35% in the nonsurgical group. Despite this, mortality rate did not vary significantly between the groups (nonsurgical: 12.5% vs. surgical: 15%). Molinari et al. [25] showed comparable results with respect to complication rate (surgical: 24% vs. nonsurgical: 6%) and mortality rate (surgical: 20% vs. nonsurgical: 12.5%) for type II fractures. However, treating physicians are well aware of the problems coming along with patients of advanced age, and management policies have been adjusted. Not surprisingly, several contemporary studies have demonstrated a significant decrease in the mortality rate in geriatric patients treated surgically compared to those treated nonsurgical [28-30].
Chapman et al. [29] demonstrated that surgical treatment of type II odontoid fractures in an elderly population did not negatively impact survival, even after adjusting for age, sex, and comorbidities. They suggested a significant 30-day survival advantage and a trend towards improved long-term survival for operatively treated over nonoperatively treated patients.
After adjusting the analyzes for age, sex, comorbidity and year of injury, Robinson et al. [31] could show a lower 1-year mortality of surgically treated patients compared to nonsurgical treated patients. Nevertheless, the positive effect of surgical treatment lost its effect on survival in patients aging >85 years of age.
Vaccaro et al. [28] published a prospective study demonstrating the severity of these fractures in geriatric patients showing a significantly lower nonunion rate in the surgical group compared to the nonsurgical group (5% vs. 21% in the nonsurgical group; p=0.0033). This was confirmed by others too [32-34]. Interestingly, complication rate did not differ significantly comparing both groups even in experienced hands. There was a trend in the mortality at 1 year towards a higher rate in the nonsurgical group compared with the surgical group (26% vs. 14%, respectively; p=0.059) [28].
A possible selection bias of patient’s eligible/noneligible for surgery might change the results in complication rate and mortality rate, independently from the study design (retrospective/prospective). Presumably, healthy patients or patients with an acceptable risk for an operation are more often referred to surgery than to conservative treatment. Therefore, nonsurgical treatment is mainly used for multimorbid patients with a significantly raised anesthetic risk. Our data support this hypothesis. The surgically treated patients showed a mean ASA-Score of 2.78±0.71 compared to a mean ASA-Score of 3.15±0.66 for the nonsurgically treated patients. Although, there was no significant difference (p=0.016), there might be a tendency towards sicker patients treated conservatively.
Conservative management employing a halo thoracic vest or a semirigid collar is not as “noninvasive” as one could assume. Patients are as well restricted in their activity of daily living as compromised in their normal food intake and the excursion of the chest. The latter may result in an insufficient respiratory function [35] and increased risk of pneumonia or respiratory distress [36]. Furthermore, dysphagia caused by external immobilization may lead to aspiration [37,38], dehydration and malnutrition [39,40].
Early rehabilitation may diminish the risk of pneumonia and, possibly, lead to a higher level of restored function, and greater quality of life. It is speculative, whether this effect may be spoiled, if an early mobilization and restoration of activity of daily living are not possible due to external immobilization devices.
Limiting factors regarding this study have to be acknowledged. The retrospective character of this study leads to associated inherent biases. Furthermore, data were collected from documented electronic records, operative reports, radiological data, and reports of the patients. The treatment regime was solely defined by the attending neurosurgeon. Thus, a standardized operating procedure for the fracture treatment was missing. Additionally, the number of conservative treated patient is relatively low diminishing the conclusiveness of statistical analysis. The follow-up, a 90-day-period, was relatively short, therefore, data on longterm survival and functional status are lacking.
CONCLUSION
According to our data, surgical treatment of type II fractures shows a higher rate of bony consolidation compared to patients treated conservatively. Nevertheless, surgery may imply a higher complication rate for the patients. Mortality rate nears for both groups to a nonsignificant difference according to our data. This implies that any treatment regime should be individually tailored to the patient. We suggest that—whenever the anesthetic risk is acceptable—surgery should be offered as the treatment of choice. Yet, conservative management remains a valuable option especially in octogenarians with striking comorbidities.
Notes
The authors have nothing to disclose.
Acknowledgements
An IFOREs grant (D/107-40960) to Oliver Gembruch from the University Duisburg-Essen supported the research (https://www.uni-due.de/med/forschung/forschungsfoerderung/ifores-programm). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.