A 1-Year Cost Analysis of Spinal Surgical Procedures in Spain: Neurosurgeons Versus Orthopedic Surgeons
Article information
Abstract
Objective
To evaluate the direct costs of various spinal surgical procedures within 1 year of follow-up and to compare the profiles of neurosurgeons and orthopedic surgeons.
Methods
All spinal procedures performed within a 10-month period in patients covered by a private insurance company were included. Costs related to the spinal interventions were systematically registered in the company database. Associated costs during the 1-year follow-up were recorded.
Results
In total, 1,862 patients were included, with a total cost of €11,050,970, of whom 34.8% underwent noninstrumented lumbar decompression (€3,473), 27.1% dorsolumbar instrumented fusion (€6,619), 14.6% nucleoplasty (€1,323), 13.5% cervical surgery (€4,463), 3.4% kyphoplasty (€4,200), 2.9% scoliosis (€15,414), 1.2% oncologic surgery (€5,590), 0.5% traumatic compression (€7,844), and 4.7% (€1,343) other minor interventions (mainly rhizotomies). Approximately 42% of patients required reinterventions within the first year, with a global extra cost of €7,280,073; 11% were referred to the pain clinic, with a €114,663 cost; 55.5% were men; and the most common age range of patients who received an intervention was 65–75 years. Neurosurgeons performed 60% of all interventions. Noninstrumented lumbar operations were performed by neurosurgeons twice as often as instrumented operations, and they performed 76% of cervical operations. Orthopedic surgeons performed 2.5 times more instrumented than noninstrumented lumbar operations, and almost all scoliosis and rhizotomy procedures.
Conclusion
The direct costs of spinal surgery in Spain were generally lower than those reported in other European Union countries and the United States. Neurosurgeons and orthopedic surgeons had different spine surgical profiles and costs.
INTRODUCTION
Cost-effectiveness research in spine surgery has become a key topic in the last decade. Cost calculation methodology remains a common bias in many studies, in which costs are extrapolated or indirectly calculated. Differences in interventions between neurosurgeons and orthopedic surgeons have never been considered.
Spinal surgeries have been increasing in the past few decades, creating a burden on health care budgets, which have increased global costs by 175% from a decade ago in the United States (US) [1]. The annual cost of spine care in the US has been estimated at €94 billion [2,3].
Many cost-effectiveness studies in spine care have recently been published. One of their major limitations is the heterogeneous way in which costs are calculated or estimated. Moreover, most are performed in the US setting, where medical costs are completely different from those in European countries.
In this study, we present the direct costs of 1,862 different spinal surgical procedures systematically registered during a 1-year follow-up among the patients of a leading health care insurance company in Spain. Given these procedures can be performed by neurosurgeons or orthopedic surgeons, the differences between them are discussed.
MATERIALS AND METHODS
We studied the costs attributed to all the spinal surgical procedures performed on patients from a health care insurance company in Spain (Sanitas), within a 10-month period. Associated costs during a 1-year follow-up were also considered. Cost data were systematically registered in the company database.
Total direct costs of the various spinal surgical interventions performed include the preoperative consultation, imaging studies (X-ray, magnetic resonance imaging, computed tomography), hospital costs (surgical intervention, medications, blood transfusions, days of stay), medical fees, implants, physical medicine treatments, and ambulance transfers. One-year postsurgery follow-up costs were also considered, including the previous costs, but mainly the costs of surgical reinterventions and pain clinic treatments.
1. Data management
Using the databases of surgical intervention process and follow-up, we performed a statistical analysis. A descriptive analysis of the variables was performed, and a dynamic dashboard, cross tabulating data by sex, age, type of intervention or surgeon’s specialty, was designed. Costs are expressed as mean±standard error of the mean when needed. A p-value of less than 0.05 was considered statistically significant.
2. Ethical issues
The study data were collected, preserving in all cases the patients’ anonymity and adhering to the criteria of the national data protection agency. Institutional Review Board approval was not required because it was not a clinical study. All the patients had previously signed an informed consent document that allows the management of data registered in this study.
RESULTS
A total 1,862 patients who underwent various spinal surgical procedures were included. Over a year, it resulted in a 0.2% incidence of spinal surgery among the insured population. Lumbar spine surgery (both instrumented fusion and decompression via laminectomy or discectomy) represented more than 60%, followed by percutaneous nucleoplasties and cervical spine surgery (Fig. 1).
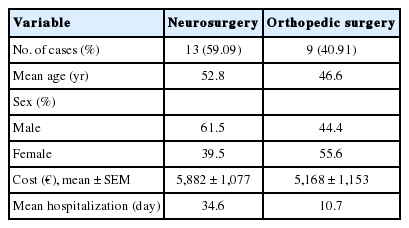
Overall, 55.5% of the patients were men and 44.5% women, with a mean age of 53.6 years, and a major incidence of intervention range of 65–75 years (15%). Neurosurgeons performed 60% of the interventions and 40% of the interventions were performed by orthopedic surgeons. The direct cost of all spinal interventions was €11,050,970.
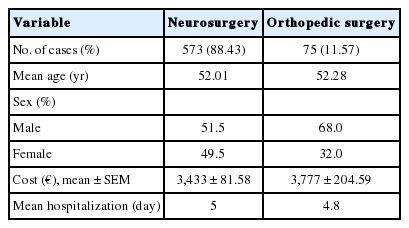
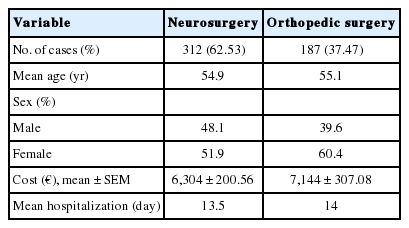
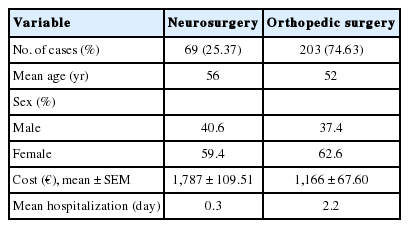
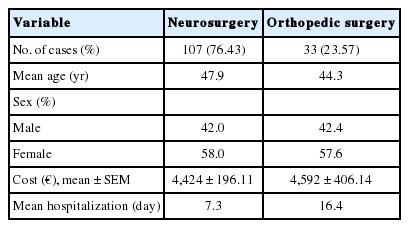
Surgical interventions were grouped as follows: noninstrumented lumbar surgery (laminectomy, discectomy, and foraminotomy, always one level), instrumented dorsolumbar surgery (all variations, mean levels affected 1.7), nucleoplasty, cervical surgery, kyphoplasty, scoliosis, oncological surgery, and posttraumatic surgery with spinal cord compression. The main data (direct cost, days of hospitalization, age, and sex distribution) for every specific procedure are shown in Tables 1-8.
The “other” group included minor procedures such as rhizotomies and biopsies, and these are not included in a Table. They had an average cost of €1,343 and were all performed mostly by orthopedic surgeons (91%) in an ambulatory setting.
Within the first year of follow-up, 42% of the patients experienced any kind of reintervention, with an overall extra cost of €7,280,073; 205 patients were treated in a pain clinic, with a cost of €114,663. Surgical reintervention frequency and median costs were distributed as follows: noninstrumented lumbar surgery (40.57%; €4,876), instrumented dorsolumbar surgery (26.52%; €8,099), nucleoplasty (13.96%; €3,132), cervical surgery (7.52%; €5,664), kyphoplasty (3.47%; €8,139), scoliosis (1.98%; €18,995), oncology (0.74%; €5,475), trauma (0.49%; €19,130), and “other” procedures (4.7%; €4,911).
DISCUSSION
Costs are an increasingly important aspect of health care. In spine surgery, cost-effectiveness research has become a key topic in the last decade. However, cost calculation methodology remains a common bias in many studies, in which costs are extrapolated or indirectly calculated [1]. Moreover, there are substantial differences in cost inclusion criteria and type of surgery definitions among the published studies.
This study investigated, for the first time, the exact direct cost of various spine interventions in a broad population in Spain. As far as we know, no previous studies have analyzed the differences between neurosurgeon and orthopedic surgeon profiles.
Indirect costs, such as those related to lost productivity or social care, were not considered. Other so-called “intangible costs” related to the decreased value of life enjoyment because of illness, were also not estimated due to the difficulty in quantifying them [4].
Noninstrumented lumbar decompression surgery was the most common intervention, and comprised more than one-third of all procedures. Costs were lower, but in a similar range, as those described by others in the European setting (prices adjusted to 2014 euros according to inflation rates): €3,473 our study in Spain, €4,218 in France [5], €3,767 in Finland [6], and €5,292 in the Netherlands [7]. Similar results have been published in Canada (€4,724) [8] and (€3,146) [9]. On the other hand, published costs in the US (€13,342) [10] or Switzerland (€10,978) [11] are much higher.
Most of these surgeries were performed by neurosurgeons (88.4%), but with similar data to that of orthopedic surgeons. Interestingly, the days of hospitalization can appear excessive for this procedure, but it is a consequence of the long stays of a few patients who suffered postoperative complications. Some 58% of patients had a stay of less than 2 days.
Instrumented dorsolumbar surgery was the second-most common intervention (27%). Compared with other European Union countries, the cost in Spain is clearly the cheapest. In our study, the cost was €6,619, whereas it would be €11,679 in Denmark [12], €15,065 in the United Kingdom and €10,985 in Italy [11]. In Canada, the cost would be €12,312 [9], with €22,014 in Switzerland [13] and €19,281 in the US; however, this study includes some follow-up costs [14] (all prices adjusted to 2014 euros, according to inflation rates).
The cost differences can be related to at least two factors: (1) the country’s socioeconomic level, and (2) the coexistence or not of a public and private health system. In this way, the prices in other European Union countries and Canada are in the range of Spain, but in others, such as Switzerland and the US, costs are 2 or 3 times higher. In most of the European Union countries (i.e., France, Holland, Denmark, United Kingdom, Italy, or Spain), and also in Canada, there are powerful and prestigious public health systems. In others such as Switzerland the public and private systems coexist and both have a well-recognized reputation too, but probably the higher socioeconomic level of this country is the main reason for its costs.
Although most of the instrumented surgeries were performed by neurosurgeons, but it should not confuse us. In this study, over 60% of all procedures were performed by neurosurgeons; however, the noninstrumented surgery they performed was double that of the instrumented. On the other hand, orthopedic surgeons performed 2.5 times more instrumented surgery than noninstrumented. The cost of an orthopedic surgeon for this surgery is approximately 12% higher than for a neurosurgeon. It can be argued that the billing process could affect the choice of surgical procedures in the private setting, but it would be highly unethical and we cannot consider it as a possibility.
Nucleoplasty involves several minimally invasive percutaneous intradiscal treatment methods, such as radiofrequency thermocoagulation, targeted disc decompression, plasma-laser, annulo-nucleoplasty, and others [15]. In Spain they are performed mainly by traumatologists, most often in an ambulatory setting. Its high incidence is surprising; even more so when these techniques, which have a variable success rate, are not yet fixed in the algorithms of axial pain treatment.
Cervical surgery in our study was mainly performed by neurosurgeons, with costs similar to orthopedic surgeons. In this area, there are very few quality studies for cost comparison [16].
On the other hand, kyphoplasties, and even more so scoliosis, are typically performed by orthopedic surgeons. In all these cases, the days of hospitalization were significantly higher in the trauma group. This difference can partially be explained by the fact that traumatology is usually the first specialty that requires consultation by others, such as internal medicine, and many of these patients have comorbidities that prolong their in-hospital stay.
The high incidence of secondary interventions was the most surprising result of this study. Although there are similar reported reintervention rates, it should not exceed 10% [17]. As a consequence, the insurance company is now revising the surgical criteria of the various surgeons and is following their results. However, part of the “reinterventions” can include those of patients submitted to minor interventions such as rhizotomies or failed nucleoplasties; it should be noted that the latter incidence was especially high in our study. On the other hand, the absence of an insurance policy regarding the authorization of secondary interventions could affect the high reoperation rate during the first-year follow-up.
More difficult to explain is the significant increase in the cost of these surgical interventions compared with the first: noninstrumented lumbar surgery is +28.8% more expensive, instrumented dorsolumbar surgery +18.3%, nucleoplasty +57.8%, cervical surgery +21.2%, kyphoplasty +48.4%, and scoliosis +18.9%.
Within the first-year postintervention, only 11% of patients were referred to a pain clinic, at a cost of €559/patient. This cost is very low, probably because they were referred very late, and the cost includes only the first treatments performed in the pain clinic. The management of patients with failed back surgery is currently well defined and has attained a long-term success rate of 65%, with a final reintervention rate of 16%; far from the 42% found in our study [18].
The major limitation of our study is the consideration only of the direct costs generated from the payer’s perspective. On the other hand, this limitation could also be interpreted as its strongest point, given that many of the cost-effectiveness studies speculate about the direct cost calculations through estimations or extrapolations (and even more so with the indirect costs). The patients’ clinical and social data inclusion would have allowed us to know the patients’ outcome and to calculate the indirect costs generated, but this approach would require a much more complex design. Despite this limitation, the high reintervention rate tells us something about our patients’ outcome. Surgical indications must be constantly revised, and patients should be referred to the pain clinic before considering a second intervention.
Spinal surgeons, including neurosurgeons and orthopedic surgeons, should make decisions on what type of surgery to be executed based on many reasons. Their training background (neurosurgey or orthopedics) should play only a small role in the process of decision making. Our study might oversimplify the process of decision making, but the most relevant conclusion of this study is that the training background of the surgeon (neurologist or orthopedist) is the only significant conditioning factor in the process of decision making. As far as we know, there are no studies investigating this factor in other countries.
The population in European countries and in the US is gradually aging. By 2030, the expected percentage of people over 65 in the US is expected to be 20%, and higher in Europe [3]. With this perspective, the prevalence of degenerative spinal disorders needing treatment will also increase. Decompressive surgeries, fusion surgeries and kyphoplasties will necessarily improve in coming years [3,19]. An accurate knowledge of spine treatment costs, outcomes and alternative treatment strategies is mandatory for all the clinicians and health care managers involved.
CONCLUSION
The direct costs during a 1-year follow-up of various spinal interventions in the Spanish population have been recorded for the first time. Costs are generally cheaper than those recorded in other European countries and, more significantly, than in the US.
Neurosurgeons and orthopedic surgeons have different activity profiles in our country. Neurosurgeons perform noninstrumented lumbar surgery twice as often as instrumented surgery, and they perform 3 of 4 cervical surgeries. However, orthopedic surgeons perform more instrumented surgeries, they are responsible of most kyphoplasties and they perform almost all scoliosis surgeries and minor interventions such as rhizotomies.
The high incidence of reintervention must be analyzed, and the role of nonsurgical treatments (rehabilitation, pain clinic) improved, especially in the failed back surgery setting.
Notes
The authors have nothing to disclose.