|
 |
- Search
Abstract
Gas-containing (emphysematous) infections of the abdomen, pelvis, and extremities are well-known disease entities, which can potentially be life-threatening. They require aggressive medical and often surgical treatment. In the neurosurgical field, some cases of gas-containing brain abscess and subdural empyema have been reported. Sometimes they progress rapidly and even can cause fatal outcome. However, gas-containing spinal epidural abscess has been rarely reported and clinical course is unknown. We report on a case of rapidly progressive gas-containing lumbar spinal epidural abscess due to Enterococcus faecalis in a 72-year-old male patient with diabetes mellitus.
Emphysematous (gas-containing or gas-forming) infections of the body, especially in the abdomen and pelvis, are potentially life-threatening conditions that require prompt diagnostic work-up and aggressive medical and/or surgical treatment8). In the neurosurgical field, although rare, cases of gas-containing brain abscess, subdural empyema, discitis, and spinal intradural abscess have been reported, and sometimes rapid clinical deterioration and even death occurred1,3,4,15). Gas-containing spinal epidural abscess (SEA) is also very rare and only a few cases have been reported10,12,13,14). In one of the reported cases of gas-containing SEA, the patient developed septic shock and died within 3 days after the onset of symptoms13).
Enterococcus faecalis is an anaerobic Gram positive coccus and commensally inhabits the gastrointestinal tract19). While this normally does not cause disease in the intestine, it can be pathogenic when infecting sites outside of the gut19). In the neurosurgical field, although rare, it can cause brain abscess, subdural empyema, discitis, osteomyelitis, and SEA2,5,11,16,18,20). They are one of the pathogens of gas-containing infections in the extremities, such as non-clostridial gas gangrene and necrotizing fascitis6). However, gas-containing SEA due to E. faecalis was rarely reported. Here, we report on a case of rapidly progressive gas-containing lumbar SEA due to E. faecalis in a 72-year-old male patient with diabetes mellitus (DM).
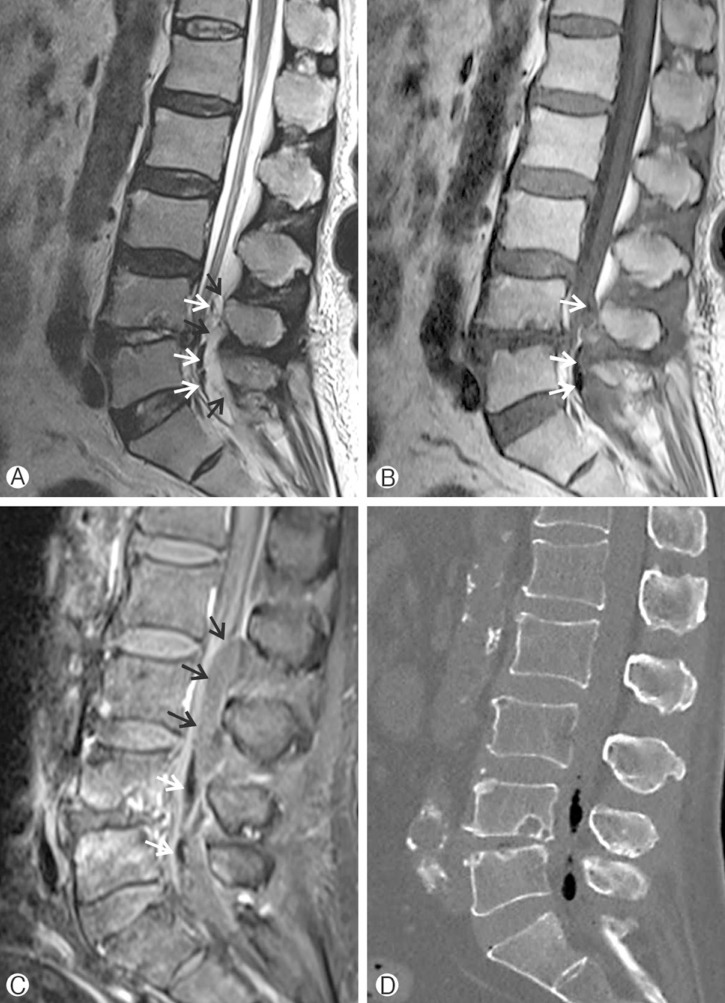
A 72-year-old man presented to the emergency department with a 3-day history of increasing low back pain (LBP). He was receiving medication for DM and hypertension for 2 years. He had no recent history of febrile illness and had not received any spinal procedure or intervention. On examination, he was afebrile, had no pain in the legs, and no neurological deficit. Magnetic resonance imaging (MRI) of the lumbar spine in the emergency department showed abnormal signal intensity in the L4-L5 intervertebral disc and in the L4 and L5 vertebral bodies. Gas was evident in the lumbar spinal canal. Thecal sac compression from a posterior epidural lesion was demonstrated from L4 to S1 level (Fig. 1A, B). Under the suspicion of lumbar SEA, he was admitted to the neurosurgical department. On admission, blood lab and blood culture were done. The laboratory findings showed a white blood cell (WBC) count of 10,890 cells/mm3 (normal: 4,000-10,000 cells/mm3), an erythrocyte sedimentation rate (ESR) of 129mm/h (normal: 0-9mm/h), and a C-reactive protein (CRP) level of 15.79mg/dL (normal: <0.5mg/dL). Hemoglobin A1c (HbA1c) was 8.1%(normal: 4.0-5.6%).
He was febrile from the night of the day of admission. LBP worsened and numbness in the legs developed. Gadolinium-enhanced MRI performed the next day revealed markedly increased extent of the epidural abscess from lower L2, increased amount of gas, and anteriorly displaced cauda equina (Fig. 1C). Gas was clearly demonstrated in non-enhanced computed tomography (CT) scan of the lumbar spine (Fig. 1D).
Under the impression of lumbar SEA, he was brought to the operating room for an emergent operation. Just before starting to the operating room, he complained of residual urine sensation after voiding. He underwent multilevel laminectomy from L3 to S1 and evacuation of the abscess. Frank pus was identified in the epidural space. Cultures from the epidural abscess and the L4-L5 disc grew E. faecalis. Blood cultures performed on the day of admission also grew E. faecalis. The pathogen was sensitive to ampicillin and antibiotic treatment with intravenous ampicillin was begun. Intravenous ampicillin was administered for 6 weeks and discontinued without additional oral antibiotic treatment. On discharge, his pain and clinical condition improved greatly and the WBC count, ESR, and CRP levels were within normal limits.
Gas-containing infection can occur in many regions and organs in the body. Gas-containing infections of the abdomen, pelvis, and extremities are well-known6,8). Gas-formation infections can occur with both aerobic and anaerobic microorganisms15). Carbon dioxide and water are the end products of aerobic metabolism15). Hydrogen, nitrogen, hydrogen sulfide and methane are produced from the combination of aerobic metabolism and anaerobic fermentation15). Of these gases, carbon dioxide diffuses rapidly into the surrounding tissues and is quickly absorbed because of its water solubility15). Other gases, except carbon dioxide, accumulate in tissues because of their reduced solubility in water1,15). The most common predisposing factor for gas-containing infections is reported to be DM6). High blood glucose from poorly controlled DM and poor glycolysis at the tissue level in diabetic patients may contribute to increased glucose concentrations within the interstitial fluid1,8). Organisms then use the accumulated glucose to produce gases including carbon dioxide and hydrogen by means of anaerobic fermentation8). In the present case, HbA1c measured on the day of admission was 8.1%. HbA1c measures long-term glycemic control, reflecting a time-weighted mean over the previous 3 to 4 months17). A direct relationship exists between HbA1c and mean glycemia because erythrocytes are continuously glycated during their 120-day lifespan and the rate of glycohemoglobin formation is proportional to the ambient glucose concentration17). In the Diabetes Control and Complications Trial, a HbA1c of 6% corresponded to a mean plasma glucose level of 135mg/dL, and each 1% increase in HbA1c corresponded to an increase in mean plasma glucose level of approximately 35mg/dL17). Therefore, mean glucose level over recent 3 to 4 months of the patient was more than 200mg/dL in the present case. This suggested that the poorly controlled blood glucose of the patient rendered him susceptible to gas-containing infections and to increased gas production.
Gas-forming infections can cause potentially life-threatening conditions8). In infections of the abdomen and pelvis, the initial clinical manifestation may be insidious, but rapid progression to sepsis and even death can occur8). In cases of gas-containing brain abscess, subdural empyema, discitis, and spinal inradural abscess, rapid deterioration of the clinical status and death have been reported1,3,4,15). In a case of gas-containing SEA, fatal outcome due to rapid progression was reported13). Kökeş et al.13) reported that a 52-year-old man with DM developed septic shock and died on the third postoperative day despite emergent laminectomy and evacuation of abscess. Although the final outcome was favorable, the patient's initial symptom was only LBP, but pain worsened, and numbness in the legs and residual urine sensation after voiding developed in a short time in the present case.
Enterococcus is fast emerging as a major pathogen causing serious and life threatening bacteremia and endocarditis18). It is also increasingly being implicated in spine infections18). In 2004, Tarr et al.18) reviewed 12 cases of enterococcal vertebral osteomyelitis and they noted 9 cases were reported since 1995, which may reflect the emergence of the enterococcus as a clinically important pathogen in the recent decades. In a recently published large series of SEA, the incidence of enterococcal infection was about 2.6%(2 out of 77 cases) and 4% (3 out of 82 cases)2). This emergence may be the result of the increased clinical application of broad-spectrum antimicrobial therapy without significant activity against enterococci, such as cephalosporins, quinolones, and macrolides18). Exposure to such antibiotics has been identified as a risk factor for colonization and infection by enterococci18).
E. faecalis is a major (80-90%) pathogen of human enterococcal infection19). Although rare, it can cause brain abscess and subdural empyema5,11). Also it can cause discitis, vertebral osteomyelitis, and SEA2,16,18,20). We could not find any exclusive case report or case series of SEA due to E. faecalis in MEDLINE search. Therefore, characteristic radiologic findings such as formation of gas, and clinical course are unknown. In cases of brain abscess and subdural empyema, no fatal case has been reported. In a case of brain abscess following ischemic stroke, multiple punctuate lesion of low signal intensity was found in MRI5). However, the causative organisms were Escherichia coli and E. faecalis, so it was uncertain which organism was responsible for gas formation5). In a case of osteomyelitis with paravertebral abscess due to E. faecalis, the presence of gas in the retroperitoneum adjacent to the infected vertebra was found in CT scan, the condition of the patient deteriorated quickly, and subsequently died20). In the previously reported cases of gas-containing SEA, the pathogens were Staphylococcus aureus, E. coli, a mixed Streptococcus, Peptostreptococcus, and Bacteroides, and Aeromonas hydrophila12,13,14). However, in our opinion, E. faecalis can cause gas-containing SEA. E. faecalis ferments some sugars with gas production9). Although E. faecalis typically ferments glucose without gas formation, but some strains produce sufficient gas from glucose7). In the above mentioned case of osteomyelitis due to E. faecalis, gas was found in CT scan20). E. faecalis is one of the pathogens of gas-containing infections in the extremities, such as gas gangrene and necrotizing fascitis6). Clostridium is a major cause of gas gangrene in the extremities, however, in non-clostridial gas gangrene, E. faecalis is one of the pathogens6). E. faecalis was reported to be the most common organism in necrotizing fascitis, in which the presence of gas in tissues is an important radiological finding6). In the present case, only E. faecalis grew from the disc aspirates and epidural abscess. Gas within the spinal canal might be produced from anaerobic fermentation by E. faecalis. E. faecalis might have spread hematogeneously to the lumbar spine; this is plausible, given its recovery from the blood culture.
Gas-containing SEA can rapidly progress and result in clinical deterioration, especially in patients with DM. Therefore, close monitoring of the patient, prompt diagnostic work-up, initiation of appropriate use of antibiotics, and surgical treatment should be done to obtain a favorable outcome.
References
1. Adamides AA, Goldschlager T, Tulloch SJ, McMahon JH. Pneumocephalus from gas-forming Escherichia coli subdural empyema. Br J Neurosurg 2007 21:299-300. PMID: 17612923.


2. Adogwa O, Karikari IO, Carr KR, Krucoff M, Ajay D, Fatemi P, et al. Spontaneous spinal epidural abscess in patients 50 years of age and older: a 15-year institutional perspective and review of the literature: clinical article. J Neurosurg Spine 2014 20:344-349. PMID: 24359002.


3. Aghaei Lasboo A, Walker MT, Hijaz TA. An unusual appearance of discitis due to gas-forming Escherichia coli with associated pneumocephalus. Spine (Phila Pa 1976) 2010 35:E257-E259. PMID: 20228705.


4. Cho KT, Park BJ. Gas-forming brain abscess caused by Klebsiella pneumoniae. J Korean Neurosurg Soc 2008 44:382-384. PMID: 19137083.



5. Davenport RJ, Gibson R, Mumford CJ, Will RG. Brain abscess complicating ischemic stroke. Stroke 1995 26:1501-1503. PMID: 7631361.
6. Fazeli MS, Keramati MR. Necrotizing fascitis: an epidemiologic study of 102 cases. Indian J Surg 2007 69:136-139. PMID: 23132965.


7. Gillespie SH, Hawkey PM. Principles and Practice of Clinical Bacteriology. ed 2. West Sussex: John Wiley & Sons; 2006. p.59-60.
8. Grayson DE, Abbott RM, Levy AD, Sherman PM. Emphysematous infections of the abdomen and pelvis: a pictorial review. Radiographics 2002 22:543-561. PMID: 12006686.


9. Gupte S. The Short Textbook of Medical Microbiology for Dental Students. New Delhi: Jaypee Brothers Medical Publishers; 2012. p.136-137.
10. Hur JW, Lee JB, Kim JH, Kim SH, Cho TH, Suh JK, et al. Unusual fatal infections after anterior cervical spine surgeries. Korean J Spine 2012 9:304-308. PMID: 25983839.



11. Jones BL, Wilcox MH. Subdural empyema due to Enterococcus faecalis. Scand J Infect Dis 1997 29:627-628. PMID: 9571746.


12. Kirzner H, Oh YK, Lee SH. Intraspinal air: a CT finding of epidural abscess. Am J Roentgenol 1988 151:1217-1218. PMID: 3263775.

13. Kökeş F, Iplikçioğlu AC, Camurdanoğlu M, Bayar MA, Gökçek C. Epidural spinal abscess containing gas: MRI demonstration. Neuroradiology 1993 35:497-498. PMID: 8232872.


14. Lee JS, Choi SM, Kim KW. Triparesis caused by gas-containing extensive epidural abscess secondary to Aeromonas hydrophila infection of a thoracic vertebroplasty: a case report. Spine J 2013 13:e9-e14.

15. Nadkarni T, Shah A, Kansal R, Goel A. An intradural-extramedullary gas-forming spinal abscess in a patient with diabetes mellitus. J Clin Neurosci 2010 17:263-265. PMID: 20036548.


16. Pascaretti C, Legrand E, Laporte J, Fromont P, Masson C, Brégeon C, et al. Bacterial endocarditis revealed by infectious discitis. Rev Rhum Engl Ed 1996 63:119-123. PMID: 8689282.

17. Saudek CD, Derr RL, Kalyani RR. Assessing glycemia in diabetes using self-monitoring blood glucose and hemoglobin A1c. JAMA 2006 295:1688-1697. PMID: 16609091.


18. Tarr PE, Sakoulas G, Ganesan A, Smith MA, Lucey DR. Hematogenous enterococcal vertebral osteomyelitis: report of 2 cases and review of the literature. J Infect 2004 48:354-362. PMID: 15066338.


19. Yuen GJ, Ausubel FM. Enterococcus infection biology: lessons from invertebrate host models. J Microbiol 2014 52:200-210. PMID: 24585051.



20. Zamora A, Florez J, Vidal F, Richart C. More on enterococcal osteoarticular infections: vertebral osteomyelitis. Br J Rheumatol 1997 36:1132-1133. PMID: 9374938.


Fig. 1
Magnetic resonance imaging of the lumbar spine. (A) Sagittal T2-weighted image and (B) sagittal T1-wighted image show abnormal signal intensity in the L4-L5 intervertebral disc and in the L4 and L5 vertebral bodies, air (white arrows) within the spinal canal at L5 level, and posterior epidural mass (black arrows) from L4 to S1 level. (C) Gadolinium-enhanced magnetic resonance image on the following day shows markedly increased extent of epidural abscess (black arrows) from lower L2 to S1 level and anteriorly displaced cauda equina. Increased amount of gas (white arrows) is also evident. (D) Non-enhanced computed tomography scan shows gas within the spinal canal.