From the Spinopelvic Parameters to Global Alignment and Proportion Scores in Adult Spinal Deformity
Article information
Abstract
In the last 20 years, sagittal alignment and balance of the spine have become one of the most important issues in the field of spine surgery. Recent studies emphasize that sagittal balance and alignment are more important for health-related quality of life. The understanding of normal and abnormal sagittal alignment of the spine is necessary for the diagnosis and appropriate treatment of adult spinal deformity (ASD), and we will discuss the currently used classification of ASD, the parameters of sagittal alignment that are essential for the diagnosis of spinal deformity, compensatory actions to maintain sagittal balance, and the relationship between sagittal alignment and clinical symptoms. Furthermore, we will also discuss the recently introduced Global Alignment and Proportion scores. The Korean Spinal Deformity Society is publishing a series of review articles on spinal deformities to help spine surgeons better understand spinal deformities.
INTRODUCTION
In the last 20 years, sagittal alignment and balance of the spine have become one of the most important issues in the field of spine surgery [1]. Adult spinal deformity (ASD) is caused by a number of factors that lead to structural changes in spinal alignment, followed by changes in balance mechanisms to achieve the most economical upright posture [2]. The resulting disability and significant loss of quality of life require surgical treatment. However, if the intended sagittal alignment is insufficiently restored after surgery, patients often complain of persistent low back pain due to the so-called flatback syndrome. Recent studies emphasize that even in coronal plane deformities such as degenerative scoliosis, sagittal alignment are more important for health-related quality of life (HRQoL) [3-5]. The understanding of spinal sagittal alignment is necessary for the diagnosis and appropriate treatment of ASD.
We will discuss the currently used classification of ASD, the parameters of sagittal alignment, compensatory actions, and the relationship between sagittal alignment and clinical symptoms. Furthermore, we will also discuss the recently introduced Global Alignment and Proportion (GAP) scores and its clinical usage.
The Korean Spinal Deformity Society is publishing a series of review articles on spinal deformities to help spine surgeons better understand spinal deformities.
1. From the spinopelvic parameters to GAP scores in ASD
2. The selection of fusion level for adolescence idiopathic scoliosis
3. The proximal junctional kyphosis and failure after spinal fusion for ASD
4. The sacropelvic fixation for spinal deformity surgery
SCOLIOSIS RESEARCH SOCIETY-SCHWAB CLASSIFICATION
In 2007, Schwab et al. [6,7] proposed a Clinical Impact Classification of ASD by applying the concept of sagittal alignment of the Lenke classification of pediatric scoliosis to ASD. This classification used radiologic parameters related to HRQoL and initially described 5 types of scoliosis based on the location of the apex of the scoliosis curve: type I, thoracic only; type II, upper thoracic major; type III, lower thoracic major; type IV, thoracolumbar major curve; type V, lumbar major curve [7]. Schwab et al. [7,8] used 3 radiological parameters, lumbar lordosis (LL) and intervertebral subluxation as sagittal modifiers, and sagittal vertical axis (SVA) as the global balance modifier. Based on other studies, the Scoliosis Research Society (SRS) revised the SRS-Schwab ASD classification in 2012 for a practical approach to radiologic classification of ASD [9]. The classification utilizes spinal and pelvic parameters that have high interobserver and intraobserver reliability and are useful for classification [9]. Patients are categorized by primary coronal deformity and SVA, pelvic tilt (PT), and pelvic incidence (PI)-LL mismatch are used as modifiers to determine sagittal deformity (Fig. 1) [9].
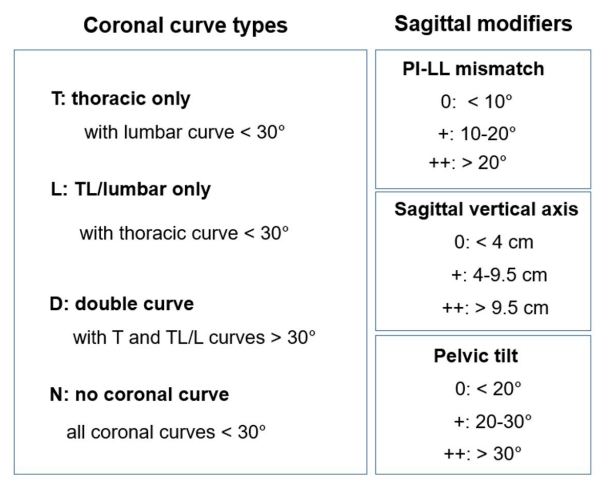
SRS-Schwab adult spinal deformity classification. A coronal curve pattern is categorized and each of 3 sagittal modifiers (PI-LL, SVA, and PT) is classified as ‘nonpathological (0),’ ‘moderate deformity (+),’ or ‘marked deformity (++).’ SRS, Scoliosis Research Society; PI, pelvic incidence; LL, lumbar lordosis; SVA, sagittal vertical axis; PT, pelvic tilt.
These sagittal modifiers are not only related to pain and disability, but are also objective measures of spinopelvic deformity on the sagittal plane and can be used to guide surgical planning.
SPINOPELVIC PARAMETERS
The pelvis and hip joints serve as a balance regulator that controls the movement of the spine [10,11]. The hip joints axis serves as a reference point for accessing the sagittal balance of the spine [12,13].
The parameters that indicate the shape and position of the sagittal curvature of the spine are called spinal parameters and the parameters that determine the shape and position of the pelvis are called pelvic parameters [14,15]. While there are numerous spinal and pelvic parameters proposed by various authors [14], this paper will discuss the spinopelvic parameters listed as sagittal modifiers in the SRS-Schwab ASD classification, as well as other parameters that may be useful.
1. Normal Spinal Sagittal Profile
According to anatomical segmentation, the spine can be divided into cervical lordosis, thoracic kyphosis (TK), LL, and sacral kyphosis.
The TK is usually placed in the range of 20°–40° [17,18] and is defined as hyper kyphosis if it exceeds 50⁰ [18]. The LL has a wider range, broadly considered with 20°–80° and narrowly 40°–60° as the normal range [11,18-20]. The LL is usually 20° larger than the TK. The TK is closely correlated with the LL, and the larger the TK, the larger the LL. As age increases, the LL gradually decreases and the TK gradually increases [19]. The average cervical lordosis is reported to be about 40° [11].
The segmental angles of the lumbar spine show that the L5 is approximately 20°, the L4 12°, the L3 9°, and the L2 5°. So, the lordotic angles of each segment account for approximately 40%, 30%, 20%, and 10% of the total LL, respectively [21]. Two-thirds of LL is formed in the L4 to S1, making these 2 segments the most significant in LL [21]. Therefore, when attempting to restore LL, emphasis should be placed on correction in these 2 segments.
2. Pelvic Parameters (Table 1) (Fig. 2)
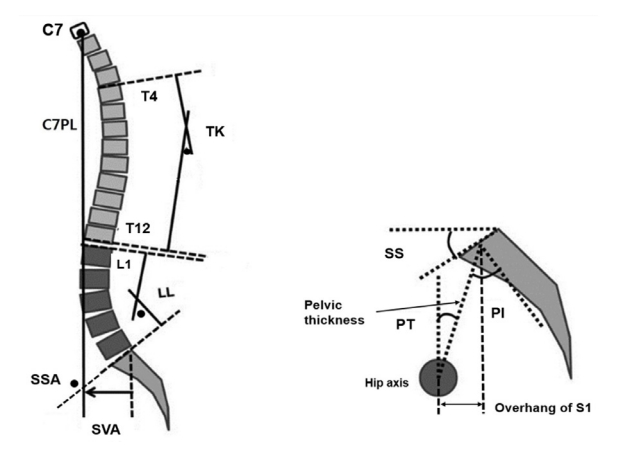
Spinopelvic parameters. C7PL, C7 plumb line; TK, thoracic kyphosis; LL, lumbar lordosis; SSA, spinosacral angle; SVA, sagittal vertical axis; SS, sacral slope; PT, pelvic tilt; PI, pelvic incidence.
To determine the sagittal alignment, it is important to understand and measure the parameters for pelvic orientation (version) and pelvic shape (morphology) [14]. The versions of the pelvis can be divided into anteversion, neutral, and retroversion with respect to the hip axis and can be determined by using positional parameters [11,14,22]. The shape of the pelvis is determined by anatomical parameters (shape parameter, morphological parameter) that do not change significantly over the lifetime depending on the position of the pelvis [10,14]. The most commonly used pelvic parameters are those described by Duval-Beaupère et al. [22] in the 1980s.
1) Positional parameters of pelvis
The positional parameters are an indicator of the degree of rotation of the pelvis around the hip axis. Sacral slope (SS) is used as a positional parameter for the horizontal plane and PT is used for the vertical plane. In addition, overhang was described as an indicator of the degree of pelvic displacement with respect to the hip axis. The reference point for these parameters is the center of endplate of S1. Other pelvic parameters have been described by different authors, who described sacropelvic angle and sacropelvic translation, which are based on the hip axis and the posterior superior margin of sacrum [23]. These are slight variations of the parameters described by Legaye et al. [10] and Duval-Beaupère et al. [22]. Of these, the sacropelvic angle corresponds to PT and the sacropelvic translation corresponds to overhang [22].
(1) Pelvic tilt
PT refers to the spatial orientation of the pelvis, which denotes to how it is positioned anteriorly and posteriorly with respect to the transverse axis through the hip joints. PT is a dynamic pelvic parameter that changes with pelvic rotation and is normally not significantly affected by PI, so changes in PT are the important indicator of pelvic compensation in pathological conditions [15,24].
In the standing position, the average PT is tilted posteriorly by 13°±6° [15,24]. As the PT increases due to pelvic compensation, the sacrum gradually becomes more horizontal and stands close to vertical. In this position, the acetabulum covers only the posterior aspect of the femoral head and further hip extension is limited. Mac-Thiong et al. stated that under normal circumstance, the upper limit of PT should ideally be no more than 50% of PI, and similarly, the ideal SS should be no less than 50% of PI. Theoretically, maximum PT can occur until the endplate of sacrum is horizontal (SS=0°) and further pelvic rotation is limited by hip extension reserve [25-27]. Theoretically, the maximum value of PT is equal to PI (Fig. 3). In summary, pelvic posterior rotation, as a phenomenon of pelvic compensation, is limited by the value of PI, and when PI is small, the capability of pelvic posterior rotation to compensate for sagittal imbalance is small [26,27].

Schematic representation of pelvic retroversion which increase PT and decrease SS by bringing back the sacrum closer to the axis of the femoral heads. This mechanism compensates for the anterior shift in the center of gravity. SS, sacral slope; PT, pelvic tilt.
It is generally accepted that the ideal pelvic position is a PT < 20°, which is the goal of surgical treatment [28]. The normal range of PT is broadly -5° to 30°. However, the normal range of PT varies depending on the individual's PI. Unlike PI, PT increases with age as a compensatory response to a decrease in LL and an increase in TK [15].
However, it is worth reconsidering whether PT simply refers to compensation for hip extension. PT practically refers to the pelvic posterior rotation angle, which combines the posterior rotation of the pelvis at the hip joint with the posterior rotation of the hip joint at knee flexion. Therefore, hip extension is the true pelvic compensation at the hip joint, and PT is the apparent pelvic compensation with compensatory knee flexion combined.
(2) Sacral slope
The SS is the important factor in determining the size and shape of lumbar curvature, and the shape and size of the lower lumbar vertebrae are directly affected by the size of the SS. By determining the shape and size of the lumbar spine, the SS determines the shape of the sagittal curvature of the entire spine [15,18].
The relationship between SS and LL was first described by Stagnara et al. [29]. The greater the SS, the deeper the lumbar curvature (“dynamic back”) and conversely, the smaller the SS, the flatter the lumbar curvature (“static back”). The size of the lower lumbar curve is equal to the SS, indicating that the lower curve is important in determining the overall LL. Roussouly et al. [30] described 4 types of LL in normal adults according to SS. SS is rarely affected by growth after the onset of walking. It has also been reported that PT increases with age but SS remains relatively unchanged [11].
2) Anatomical parameters of pelvis
Anatomical parameters are indicators of the shape of the pelvis, which changes to some degree during growth, but does not change throughout life after the complete of growth, and does not change with the position of the pelvis. However, this anatomical parameter directly influences the positional parameters to determine the size and shape of the lumbar curvature, making it the fundamental factor in determining the overall shape of the spine. Anatomical parameters include PI and pelvic thickness [10,14].
(1) Pelvic incidence
In 1992, Duval-Beaupère et al. [22] and Legaye et al. [10] described the ‘pelvic incidence’. This is similar to a vector for the load transmitted through the sacral endplate. PI represents the most important sagittal morphologic feature of the pelvis [8].
In effect, PI is equal to the sum of the SS and the PT (PI=SS+PT). PI does not change with pelvic rotation around the hip joint. If the pelvis rotates posteriorly, PT increases and the SS decreases by the same amount. If the pelvis rotates anteriorly, PT decreases and SS increases.
PI is stabilized in adulthood and does not change with age, nor does it change with pelvic position [19]. PI is a reliable measure of SS and LL [15,31]. Recently, however, there have been reports that PI increases as a process of aging, even in adulthood [5]. There is a significant chain of correlations between various pelvic and spinal parameters, of which PI plays the most pivotal role. Among these correlations, the correlations between PI and SS and between SS and LL is the highest [18]. If PI is high, SS is large and if SS is large, LL and TK is large, which affects other spinopelvic parameters. Therefore, Legaye et al. [10] stated that PI is the important factor that determines the shape of the spinal sagittal plane. However, the same PI does not always result in the same shape of the sagittal curvature because both the SS and the PT can be different [19]. So, in the other’s opinions, PI-LL mismatch is acceptable in patients with high PI.
PT determines the position and orientation of the pelvis when standing. The larger the PI, the larger SS or the lager PT, or both increases [32]. A pelvis with a small PI will have a short anteroposterior length and a long vertical pelvis, resembling the pelvis of a primate. In this case, the femoral head is located directly inferior to the sacral endplate [17]. On the other hand, a pelvis with a large PI has a horizontal pelvis with a large anteroposterior diameter, a large SS, and the femoral head is located anterior to sacral endplate (Fig. 4) [17].
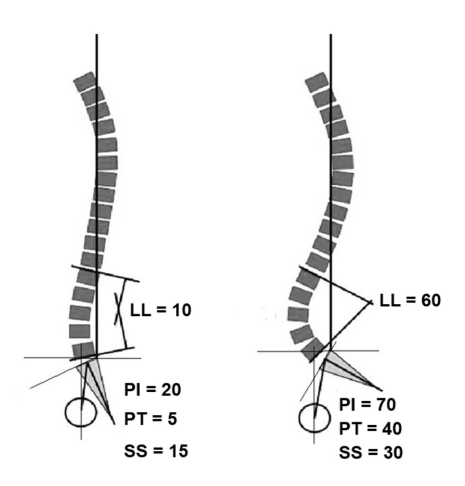
The correlation of spinopelvic parameters such as PI, PT, SS, and LL. PI, pelvic incidence; LL, lumbar lordosis; SS, sacral slope; PT, pelvic tilt.
A large PI allows for a large PT, but is limited by the extension range of the hip joint. On the other hand, a small PI allows for a small amount of posterior pelvic rotation, because of the large hip extension range, PT can occur theoretically until SS reaches zero degrees (PT=PI) [15].
The PI also determines the relative position of the sacral endplate to the femoral head, which in turn determines the position of the spine in relation to the pelvis. Barrey et al. [33] have shown that PI determines the ability to create pelvic retroversion and the patients with a larger PI have a larger range of control to PT and more room for compensatory adaptation. Those with a small PI usually have a small SS, so even a slight increase in PT can cause the SS to be close to 0, which has the advantage of moving the sagittal axis posteriorly, so it is thought that the pelvic compensatory ability is large [12]. This means that SS can reach 0 degrees relatively easily with a small PI compared to a large PI. This is thought to be due to the limited range of hip extension.
3. Sagittal Alignment Parameters (Table 1; Figs. 5, 6)

Parameters of the sagittal balance of the spine and pelvis. The spinal balance is defined as the horizontal offset between the midsacral point and C7 plumb line (C7PL); spinopelvic balance, between hip axis and C7PL; and sacropelvic balance, between hip axis and midsacral point. SVA, sagittal vertical axis; HA, hip axis.
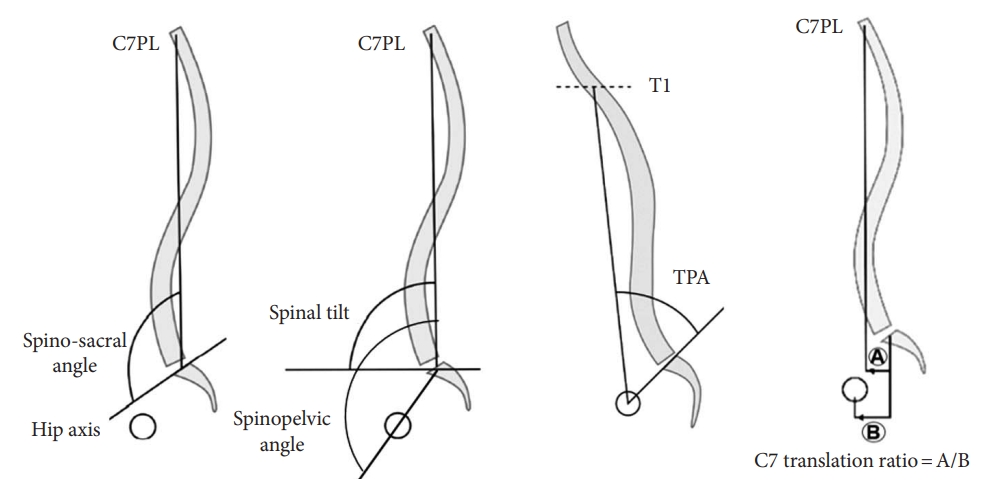
Measurement of global spinal balance. Spinosacral angle, spinal tilt, spinopelvic angle, T1 pelvic angle (TPA), and C7 translation ratio. C7PL, C7 plumb line.
Standing balance is achieved by the corrective or compensatory mechanisms of the pelvis in response to the various alterations that occur in the spinal column. The body’s gravitational lines regulate the body’s balance within a cone with a narrow point at the foot as the apex. When the body’s gravitational lines are within this cone, the body is in a balanced and economical posture, and when the body’s gravitational lines are outside of the cone, the body is out of balance. This is an uneconomical posture that requires a lot of compensation and energy. Dubousset named this the ‘cone of economy’ [34].
The balance of the spine with respect to the pelvis is called spinal balance and is determined by the relationship between the C7 plumb line (C7PL). This corresponds to the SRS definition of sagittal balance. The balance of the pelvis with respect to the hip axis is called sacropelvic balance which is determined by the relationship between the midsacral point and the hip joint axis. The balance of the whole spine and pelvis with respect to the hip axis is called spinopelvic balance, and is determined by the relationship between the C7 PL and the hip axis, which is a sagittal balance that considers the shape of the spine and pelvic compensation together [8,18,25,35].
The methods of evaluating sagittal alignment are measuring the distance from a reference point (distance parameters), measuring the angle centered on a reference point (angular parameters), and measuring the ratio between the distances (distance parameters).
The distance parameter of sagittal alignment is typically represented by SVA and angular parameters include T1 pelvic angle (TPA) and spinal tilt (ST). Sacropelvic balance is determined by PT or pelvic overhang (Fig. 2).
(1) Sagittal vertical axis
This distance is used as the important and representative parameters of spinal sagittal balance, and it is now standardized to use the SVA to determine spinal sagittal alignment and overall patient outcome [3,36]. The SVA ranges normally within 5 cm. If the SVA exceeds±5 cm, it is considered a sagittal imbalance [37-39].
Just as the C7PL is the most commonly used reference line to measure sagittal balance, but it does not reflect the alignment of the cervical spine [40,41]. It also does not reflect the role of the pelvis and lower extremities in sagittal alignment [41,42]. Therefore, a global sagittal alignment using SVA alone fails to evaluate the compensatory actions of the pelvis and lower extremities [42]. The PT, which is a parameter of compensation in the pelvis and knee joints, should be considered together [43,44]. In addition, SVA is a parameter based on the posterior superior aspect of the sacrum rather than the hip axis, which is considered the important reference point for spinal balance, but SVA < 50 mm is recognized as one of the most important criteria for sagittal balance, which is equivalent to having the C7PL located posterior to the hip axis, and this threshold is consistent with a good HRQoL score [5,11].
In radiologic measurements, angular parameters and ratios are preferred over distance parameters because they are less sensitive to changes in radiologic magnification [45]. Mac-Thiong et al. [25] proposed 3 parameters to measure global spinal alignment: the angular parameters such as ST and spinosacral angle (SSA) and the ratio parameter (C7 translation ratio). These are parameters about the position of the C7 vertebra in relation to the pelvis or sacrum.
(2) Spinal tilt
ST is greater than 90°, which means that the center of the C7 located behind the center of the sacral endplate and less than 90 degrees means that center of the C7 is in front of the center of the sacral endplate [46].
(3) Spinosacral angle
Roussouly and Pinheiro-Franco [18] showed that SSA is a quantitative measure of global kyphosis of the whole spine. In a well-balanced spine, SSA is proportional to SS and decreases with loss of LL. This relationship can be used as a guide to determine the need for kyphosis correction. There is a strong correlation between SSA and SS and LL [18,45]. In normal individuals, SSA is predicted to average 135°±8° (110°–150°), ST is predicted to be 85°–100°, and ST is close to 90° [18].
ST can be considered a functional positioning parameter that indicates the global orientation of the spine with respect to the horizon, while SSA is considered a morphologic parameter that indicates the overall kyphosis of the spine. ST and SSA can be expressed as SSA = ST+SS [45]. When sagittal imbalance occurs, ST can be maintained relatively stable by decreasing SS [18]. In particular, normal SSA values can be used to determine the degree of overall kyphosis and the outcome of surgical treatment [47]. On the other hand, ST is preferred over SSA because it is maintained in a narrow range (85°–100°) and is more closely related to the vertical line in normal adults [15].
(4) C7 translation ratio
This parameter is also an indicator using distance ratio, which can solve the problem of measurement error of distance parameter. It averages -0.9±1 [48]. The distance anterior to the center of the sacral endplate is positive value [49]. If the hip joint axis is located anterior to the center of the sacral endplate and the C7PL is located posterior to the center of the sacral endplate, the C7 translation ratio has negative value, and if the C7PL is in front of the hip joint axis and the center of the sacral endplate, it has a value greater than 1. It decreases in the case of compensatory balance and becomes greater than 1 in the case of decompensation [50].
(5) Spinopelvic angle
Roussouly and Nnadi [51] described spinopelvic angle for postural angle, which decreases with spinal kyphosis.
(6) T1 pelvic angle
SVA and PT can be altered by posterior pelvic rotation, knee flexion, or the use of bracing during standing [8,37]. According to Lafage et al. [8], when measuring SVA alone, an increase in PT can mask spinal deformity, so PT must be considered in conjunction with SVA to identify patients with spinal deformity in the absence of abnormal SVA.
Protopsaltis et al. [52] introduced a new parameter called TPA which is not affected by compensation of patient’s knee. In an individual, SVA and PT are interrelated and influence each other. This interaction is further modified by compensatory mechanisms to maintain sagittal balance, such as knee flexion and pelvic posterior rotation. However, since TPA is a parameter that considers ST and PT simultaneously, it is less affected by compensation [52]. TPA was closely correlated with SVA, PI-LL, and PT, and HRQoL gradually worsened as TPA increased, and it was highly correlated with the Oswestry Disability Index (ODI) [52]. A TPA of 20° or more leads to an ODI of 40 or more, which is the criterion for severe disability, and it is recommended to aim for a TPA of 14° or less [52]. Ryan et al. [53] recommended that the surgical target for TPA be 10o to account for postoperative correction loss. TPA is the sum of T1 tilt and PT, so as the deformity increases, the TPA value also increases [53].
According to Roussouly and Pinheiro-Franco [15,18], there are 3 things to access to quickly diagnose sagittal imbalance; (1) Pelvic angles: PI, PT, and SS, (2) type of LL, (3) positioning of C7PL (SSA, ST).
Barrey et al. [54] stated that the following steps are necessary to analyze the spinal sagittal balance: (1) measurement of PI, (2) analysis of sagittal alignment by measuring SSA and C7PL/SFD ratio, (3) determination of compensatory mechanisms: LL, TK, presence of discopathy, and spondylolisthesis, (4) measurement of PT and knee flexion.
COMPENSATORY MOVEMENT
In the degenerative kyphotic changes in the spine, the sagittal alignment is maintained by hip extension, posterior rotation of pelvis, and creating lordosis in the adjacent segment of spine [55]. Also, by flexing the knee joints, which relieves tension in the anterior hip joint, making it easier for the hips to extend [56]. However, if the hips are not able to extend, the compensatory failure occurs. This can occur especially if there is a kyphotic deformity of the lower lumbar spine and the hip extensors are weakened at the same time, and Lee et al. [57] described this phenomenon as ‘sagittal spinopelvic decompensation over the hip joint,’ which is contraindicated for surgical treatment of the lumbar spine. Not all compensatory mechanisms are observed in a single patient, but compensatory mechanisms will be present to varying degrees, depending on the flexibility of the spine, muscle condition, and degree of imbalance [54].
Legaye et al. [10] stated that pelvic posterior rotation is a sign of spinopelvic imbalance, but it does not always occur with spinopelvic imbalance.
The most basic concept of the compensatory mechanism is that it occurs by extending the neighboring segments of the kyphotic region [12]. This can lead to hyperextension and posterior displacement of the neighboring segments, which can lead to adjacent segment disease. Focal hyperextension is effective in moving the above spine posteriorly, but it overloads the posterior structures of the segment, increasing the risk of spondylolisthesis, degenerative change of the facet joints, over-compression of the spinous processes (Baastrup's disease), and sometimes spondylolysis [12,55,58].
A typical finding of sagittal imbalance in the elderly is a gradual anterior shift of the line of gravity due to increased TK and decreased LL. Once sagittal imbalance is out of range, compensation is required and several mechanisms are triggered to correct the imbalance [12]. First, the posterior muscles of the spine will contract to try to keep the trunk upright, and over time, this can lead to muscle fatigue and pain. This process can also result in excessive pressure on the facet joints, which can also cause pain. Secondly, there is the posterior rotation of the pelvis around the femoral head. However, As the aging progresses, the hip joint undergoes degenerative changes and loses its range of motion. This eventually limits the ability to strengthen the PT [12]. Also, even with normal hip range of motion, the pelvis cannot rotate posteriorly to infinity, and this posterior pelvic rotation is limited by a 10° hip extension allowance [23]. Third, in more severe cases, it is compensated for by flexion of the knee joint, which is controlled by the quadriceps muscle.
The ability of the spine to compensate for these deformities is determined by the patient’s intrinsic pelvic morphology, defined by PI. Based on the equation SS+PT=PI, posterior rotation of the pelvis will decrease SS. The significance of this equation is that the ability to change PT or SS to compensate for a vertebral sagittal imbalance is determined by the size of the PI. A large PI has a greater ability to compensate for kyphotic deformity by increasing the posterior rotation of the pelvis and decreasing SS, whereas a small PI has less range to increase PT to restore sagittal alignment [32,33,54].
However, this is limited by the remaining hip extension range after pelvic posterior rotation has occurred. This is why, after maximal pelvic posterior rotation has occurred, the spinopelvic complex uses the next level of compensation, knee flexion [37]. Therefore, in order to understand the global compensatory mechanism, it is important to understand the role of the knee joint as well as the hip joint.
RELATIONSHIP OF SPINOPELVIC PARAMETERS TO CLINICAL SYMPTOMS
Glassman et al. [36] found that anterior shift of the SVA was the most reliable radiographic predictor of HRQoL in the review of 352 patients. The degree of disability correlated closely with the degree of kyphosis, especially in the lumbar spine compared to other parts of the spine. Therefore, in the surgical treatment of ASD, we strive to achieve a postoperative SVA < 50 mm, as this is the way to achieve a physiologic standing position and level gaze. The SVA of < 50 mm means that the C7 PL is eventually positioned posterior to the hip axis and this threshold corresponds to a favorable HRQoL score [28].
Schwab et al. [28] showed that HRQoL is strongly correlated with this increase in PT and the ideal PT goal for surgery should be to achieve 20° or less. In ASD, if the increased PT is not recognized before the correcting surgery, the sagittal imbalance due to insufficient correction is likely to remain and lead to persistent symptoms [7]. Therefore, the appropriate surgical goal is to return the PT to the normal range of 20° or less [28].
However, Lafage et al. [8] analyzed spinopelvic parameters in 125 ASD patients to determine which parameters correlated est with HRQoL using ODI, SRS questionnaire, and 12-item Short Form health survey. TPA, which has been underutilized, had the highest correlation followed by SVA, and PT, which had the third highest correlation [53]. TPA was strongly correlated with ODI (r = 0.52, p < 0.0001) [53]. In addition, it was found that as PT increases, HRQoL worsens, but the worst ODI is when SVA is large and PT is small, which may indicate compensatory failure [9].
Several studies have suggested thresholds for spinopelvic parameters that can cause pain and disability. It has been reported that PT> 22°, PI-LL> 11°, and SVA> 46 mm are associated with an ODI score of 40, which is a criterion for severe disability [7,9,28]. Recent studies have suggested several other criteria such as Hamamatsu formula [59].
GOALS FOR SURGICAL TREATMENT
Schwab et al. [28] suggest that to successfully restore harmonious spinopelvic alignment, 3 key parameters should be achieved: SVA < 50 mm, PT < 20°, and PI-LL <±9°. Using SSA as a reference, it is important that it do not exceed about 135° and PT is about 20° [53].
THE GLOBAL ALIGNMENT AND PROPORTION SCORE
The GAP score was first introduced by Schwab et al. in a published study. They recognized the need for a comprehensive and practical method to assess spinal alignment and balance in patients undergoing spinal deformity surgery, and developed the GAP score as a result [59-61].
The GAP score was based on the concept of global spinal alignment, which takes into account the interrelationships between different regions of the spine and the pelvis. The authors identified several key radiographic parameters including PT, PI, LL, TK, and SVA [61]. The authors then combined these parameters into a single composite score, which they called the GAP score [60]. The score ranges from 0 to 100, with higher scores indicating better spinal alignment. The authors validated the usefulness of the GAP score in a cohort of 69 patients who underwent spinal deformity surgery, and found that higher GAP scores were associated with better outcomes in terms of pain, disability, and HRQoL [59].
Since its introduction, the GAP score has become widely used in clinical practice to guide surgical decision making and postoperative management in patients with spinal deformity. Practical use of the GAP score in spinal deformity surgery involves several steps. First, preoperative radiographs are obtained, and the various parameters used to calculate the GAP score are measured. Once these measurements have been obtained, the GAP score can be calculated using a formula that takes into account each of the individual parameters. The resulting score can then be used to guide surgical decision making, including the selection of surgical techniques and the extent of surgical correction. Postoperatively, the GAP score can be used to monitor patient outcomes and assess the effectiveness of surgical correction. For example, if a patient has a low GAP score preoperatively and a high score postoperatively, this indicates that the surgical correction was successful in improving spinal alignment [59-61]. Although the usefulness of GAP score, several papers have argued that further prospective studies and revalidation of the GAP score are necessary, especially the validation between the GAP score and mechanical complication [63].
CONCLUSION
It is necessary to have a basic understanding of the ASD and the spinopelvic parameters. In addition, there are various compensatory actions that occur to maintain sagittal balance, which must be evaluated to determine correct sagittal alignment.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: YC; Formal Analysis: DJ, SJH; Investigation: NRY; Methodology: SJH, JHP; Project Administration: YC; Writing – Original Draft: NRY; Writing – Review & Editing: YC.

