Box-Shape Cervical Expansive Laminoplasty: Clinical and Radiological Outcomes
Article information
Abstract
Objective
Box-shape cervical expansive laminoplasty is a procedure that utilizes a Miniplate® or Maxpacer® to achieve maximal canal expansion. This method is expected to show much larger canal expansion and good clinical outcome. So we investigated the clinical and radiological outcome of Box-shape cervical expansive laminoplasty.
Methods
Between June 2008 and July 2013, we performed cervical expansive laminoplasty in 87 and 48 patients using the Box-shape cervical expansive laminoplasty, respectively. We analyzed the clinical results of these operations using the Japanese Orthopedic Association (JOA) scoring system and by assessing the position of intralaminar screws with postoperative computed tomography (CT) at POD-6 months.
Results
A total of 48 patients with ossification of the posterior longitudinal ligament (OPLL) (36 pts), cervical spondylotic myelopathy (CSM) (12 pts) were enrolled. Overall JOA scores improved from 11.49 to 14.22 at POD-6 months (OPLL: 11.32 -->14.3; CSM: 12-->14). Postoperative CT scans were performed in 39 patients at 177 levels for a total of 354 screws. The malpositioning rate of intralaminar screws was 3.4% and hardware-related neurologic complications did not occur.
Conclusion
Box-shape cervical expansive laminoplasty creates maximal spinal canal expansion and leads to improved cervical myelopathy. The use of intralaminar screws to fix the remodeled lamina-facet does not represent a significant difficulty.
INTRODUCTION
Degenerative cervical spondylosis, herniated cervical discs, and ossification of the posterior longitudinal ligament (OPLL) can result in chronic compression of the spinal cord. Surgical treatment for this condition requires an anterior or posterior approach. Posterior approaches to decompression, such as laminectomy and laminoplasty, are typically indicated for cervical myelopathy3,6,7,10,16,19). Cervical laminoplasty has gradually become an established intervention for compression. Cervical expansive laminoplasty was originally carried out using spinous processes as spacers. Since development of classic open-door laminoplasty with the use of sutures, the procedure has been modified to reduce complications such as restenosis, axial symptoms, and segmental motor paralysis1,12,13,14,20).
Various modifications to expansive laminoplasty have been developed and clinical outcomes are typically satisfactory in patients with cervical spondylotic myelopathy (CSM). In fact, one of the most popular modifications is a bilateral hinge-type laminoplasty procedure called the double-door laminoplasty. Development of surgical implants for expansive laminoplasty has resulted in surgeons using various kinds of lamina spacers.
Previously, we introduced a new type of modified expansive double-door laminoplasty that utilizes a titanium miniplate system for an Box-shape cervical expansive laminoplasty14). This method showed much higher canal expansion rate than that of other cervical spacers such as hydroxyapatite (HA) (Apaceram®) and Centerpiece®8,9,14)(Fig. 1). So this new method was expected to show good clinical outcome but it was not studied up to date.
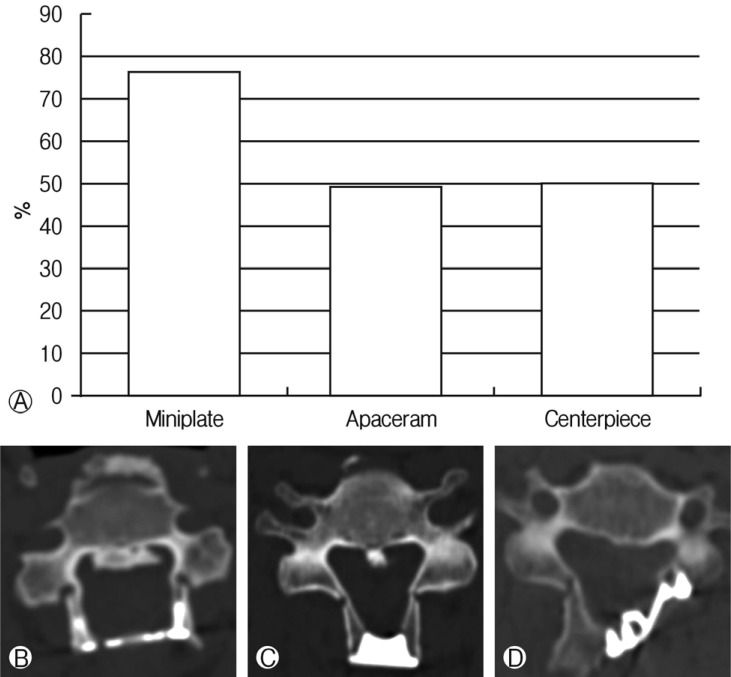
(A) Canal expansion rate for surgeries performed with Box-shape cervical expansive laminoplasty, Apacerum®, and Centerpeice®. CT axial image of the (B) Box-shape cervical expansive laminoplasty, (C) Apacerum®, and (D) Centerpeice®.
In this study, we analyzed clinical and radiological outcomes of Box-shape cervical expansive laminoplasty.
MATERIALS AND METHODS
1. Study Population
Between June 2008 and July 2013, a total of 87 patients with OPLL and CSM underwent laminoplasty at our institute with Box-shape cervical expansive laminoplasty (60 pts), Apaceram® (1 pt), centerpiece® (20 pts). All patients presented myelopathy in a physical exam and cord compression was observed by MRI.
A total of 48 patients (OPLL(36 ts), CSM(12 pts)) that underwent Box-shape cervical expansive laminoplasty with Miniplate® or Maxpacer® were enrolled to this study. Male patients were more common than females (M:F=35:13) and the average age was 62.83 (max 81, min 30) (Table 1).
2. Surgical Techniques
A French-door (double-door) laminoplasty was used in all cases discussed. Horizontal amputation of the spinous processes was performed and bilateral lamina exposure was carried out. Midline laminotomy was subsequently achieved with a drill and lateral outer cortical bone drilling was performed to facilitate elevation. When performing lateral outer cortical bone drilling, the surgeon must find the lamina-facet junction, which is a landmark for drilling. It is important to drill medially to the facet joint to have adequate spinal canal area. Because a narrow drilling space can induce lamina fracture during elevation, adequate space is important to avoid fracture. After drilling, the ligament flavum was split centrally and each lamina and ligamentum flavum was opened bilaterally until the lamina stood straight. After proper positioning of the lamina, miniplates were applied to the space between both lamina. Intra-laminar drilling was performed for miniplate screw fixation. A miniplate is typically fixed with an 8-mm screw14).
3. Assessment of Clinical and Radiological Outcome
Clinical outcomes of patients who received Box-shape cervical expansive laminoplasty were assessed at postoperative day (POD)-6 months using the JOA scoring system, performed by a single observer in all 48 patients. Clinical outcomes were compared to patients with OPLL (36 pts), CSM(12 pts) before and after surgery.
Postoperative CT scans were performed in 39 patients at 177 levels for a total of 354 screws to investigate the position of intralaminar screws.
RESULTS
1. Clinical Outcomes
For patients given the Box-shape cervical expansive laminoplasty, the total average JOA score improved from 11.49 to 14.22 by POD-6 months. In the 36 patients with OPLL, scores improved from 11.32 to 14.3. In the 12 patients with CSM, scores improved from 12 to 14 (Table 2). Most patients' JOA scores improved and there were none with JOA scores that decreased (Fig. 2). Only one patient suffered from temporary C5 palsy at 5 to 7 days POD.
2. Radiological Outcomes
Of the 48 patients that received the Box-shape cervical expansive laminoplasty, postoperative CT scans were performed in 39 patients at 177 levels for a total of 354 screws. The total malposition rate of intralaminar screws was only 3.4% (12 out of 354). The rates of medial invasion (Fig. 3), lateral invasion (Fig. 4), center to medial invasion, center to lateral invasion, and pulling out were 4%, 2%, 0%, 4%, and 1%, respectively (Table 3). But, hardware-related neurological complications did not occur in any of the cases.
DISCUSSION
Cervical laminoplasty is widely used to treat cervical myelopathy with OPLL or spondylosis. There have been many reports regarding satisfactory surgical outcomes using this procedure1,6,7,10,12,16,19). Double-door laminoplasty was originally devised by Kurokawa in Japan. This method achieves expansion of the spinal canal and preservation of the posterior structures for stability11,13,14,18,19,20).
The relationship between degree of spinal canal expansion and clinical outcomes was not known and current techniques for canal expansion are not sufficient5,9). However, maintaining spinal canal expansion is critical. So we developed the Box-shape cervical expansive laminoplasty for use with the Miniplate® or Maxpacer®. The Box-shape cervical expansive laminoplasty allowed for maximal expansion of the spinal canal, and neurologic deterioration caused by restenosis or hinge reclosure did not occur14).
Cervical laminoplasty using plating systems has been previously performed. Edmund Frank et al. reported a technique using titanium miniplates that permitted adequate decompression of the cervical spinal cord and bilateral cervical nerve roots. They showed successful reconstruction of an enlarged rigid spinal canal. Deutsch and Harel et al. showed successful laminoplasty using a Ti-Mesh LP miniplate system without complications in five patients. Park and Andrew E et al. reported performing laminoplasty using a novel titanium system that provided secure laminar fixation, thus minimizing the risk of canal restenosis, better preserving motion and decreasing axial neck pain2,4,17).
In this study, we investigated clinical outcomes associated with our procedure. We show that those who received Boxshape cervical expansive laminoplasty had an average JOA score increase from 11.49 to 14.22 at POD-6 months. None of the patients displayed decreased JOA scores and none developed neurologic deficits. One patient, however, suffered from C5 palsy at PODs 5 to 7, but they completely recovered by POD-6 months. Although excessive opening of the spinal canal results in risk of nerve root kinking and epidural scar tissue21,22), the major finding of this study is that maximal expansion of the spinal canal leads to improvements in JOA scores of patients with severe OPLL or CSM with narrowed canals. This result demonstrates the clinical efficacy of Box-shape cervical expansive laminoplasty.
The defining characteristic of this operation is the use of intralaminar screws to create maximal standing at each lamina. However, the double-door laminoplasty to create maximal lamina standing is a difficult technique and insertion of intralaminar screws at the proper position can be tedious. Proper positioning of the intralaminar screw is important for holding the remodeled lamina-miniplate.
To determine whether screws were inserted in the proper intralaminar position, we reviewed postoperative CT scans of the surgical methods at POD-6 months. Of the 39 patients, scanned at 177 levels in 354 screws, the malpositioning rate of intralaminar screws was only 3.4%. No hardware-related complications occurred in patients after POD-6 months and there were only 4 screws that invaded the medial wall. However, this does not present a problem because the ligament flavum is a good protector of medially invaded screws. To avoid improper screw insertion, it is essential to have an anatomical understanding of the spinous process and medial lamina wall. Additionally, even though the miniplate screw is selftapping, it does not necessarily mean that the screw will penetrate to the proper insertion point. Creating a screw pathway with a small power drill can make correct insertion of the intralaminar screw easier.
One limitation to this study is that the follow-up period was only 6 months, and posterior neck pain (VAS score) and range of cervical motion were not analyzed. And comparative study should be performed to assess clinical benefits by comparing other cervical laminoplasty methods.
CONCLUSION
The Box-shape cervical expansive laminoplasty provided maximal canal expansion and demonstrated excellent clinical benefits. This method is easy to perform, provides a rigid construct, and intralaminal screws are placed in the proper position without inducing neurologic deficits.
Notes
We certify that this manuscript is a unique submission and that is not being considered for publication by another source or in another medium. The authors have no conflicts of interest to declare. However, the author is the inventor of both the Miniplate® and Maxpacer®, which are the first, plate-type commercial devices for Box-shape cervical expansive laminoplasty.





