Surgical and Clinical Outcomes Associated With the Use of Barbed Sutures and Self-Adhering Mesh System and Polymeric Glue for Wound Closure in Multilevel or Revision Spinal Surgery: A Matched Cohort Comparative Study With Conventional Wound Closure Procedure
Article information
Abstract
Objective
Multilevel or revisional posterior spinal surgery is prone to infection and delayed wound healing, related with the wound closure time and suture strength. Knotless barbed suture is an innovative self-locking, multianchor suture. This study aims to evaluate the safety and efficacy of the knotless barbed suture and self-adhering mesh with polymeric glue in multilevel or revisional posterior spinal surgery.
Methods
This is a single-center retrospective matched cohort study. Patients were divided into 2 groups based on the wound closure method: barbed suture group with novel wound closure, and conventional suture group with conventional wound closure, 1:1 matched by the level of surgery and sex, resulting in 120 subjects each. Total operation time and wound closure time were measured intraoperatively, and perioperative clinical outcome parameters including postoperative wound complication were investigated for the first 3 months postoperatively. The distribution of continuous variables was assessed for normality by Shapiro-Wilk test, then parametric or nonparametric tests were applied accordingly (paired t-test or Wilcoxon signed-rank test).
Results
Wound closure time was significantly shorter with the novel barbed suture than with conventional suture in all subgroups divided by the level of spinal surgery: 3–5, 6–9, ≥ 10 levels (p < 0.001). The 2 groups showed no significant differences in surgical complications (p = 1.000). Specially, total operation time and wound-closing time were significantly shorter in revisional subgroup.
Conclusion
Absorbable knotless barbed suture and self-adhering mesh with polymeric glue can shorten spinal wound closure time with noninferiority in complications for multilevel or revisional spinal surgery.
INTRODUCTION
The traditional surgical wound-closing method using knotted suture materials has several inherent limitations that are challenging to overcome. Commonly used absorbable suture materials along with nylon sutures or staplers may cause in infection, scarring, and limitations in everyday activitie [1].
In a multilevel spinal surgery, a long-wound closure time is also associated with surgical site infection. Additionally, postoperative wound complications such as wound dehiscence, surgical site infection, granuloma formation are a concern for revisional operations, the preformed scar tissue formation and adhesions cause difficulty in wound closure [2-4].
Studies on the parameters for determining the level of operation segment are being investigated due to the increase in long level of segments spinal surgery, including adult spinal deformity [5-7]. Additionally, there is a growing interest on the complications of long level of segment spinal surgery, and the research of which materials used for wound closure might significantly reduce the length of an operation [8-10].
Barbed suture, also known as self-retaining or knotless suture, is a unidirectional/bidirectional antibacterial monofilament and synthetic absorbable device prepared from polydioxanone. The surgical sutures are designed with small barbs or hooks along their length and barbs have innovative self-locking and multianchor properties that engage with the surrounding tissue, providing secure and stable closure without the need for traditional knots (Figs. 1, 2). Barbed sutures excel in tissue approximation, save time owing to knotless application, and are suitable for a wide range of surgical procedures. Furthermore, they have the major advantages of reducing the wound closure time and retaining better suture strength without requiring continuous tensile force (Figs. 3, 4). They differ from the traditional interrupted Vicryl sutures (Ethicon, Johnson & Johnson medical Ltd, Livingston, UK) in that they retain strength for a longer period of time during suture [11]. Therefore bared suture have been utilized in a various surgical procedures, including gastric bypass surgery, laparoscopic surgery, and arthroplasty [12]. However, only few studies have investigated the effectiveness of barbed sutures in spine surgeries [13-15].

Schematic diagram of the muscle-fascia suture of intermittent conventional nylon suture (A) and continuous barbed suture (B). Unlike conventional sutures, the continuous barbed suture has the advantage of maintaining tension owing to the self-locking and multianchor properties.
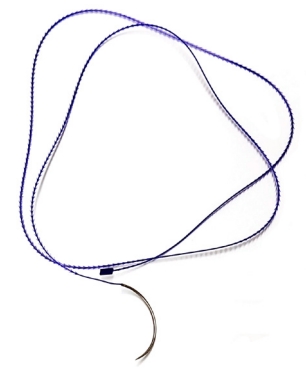
Knotless unidirectional barbed suture with a thickness of 1.0. The figure illustrates the densely arrayed unidirectional barbs with the distal end for anchoring.
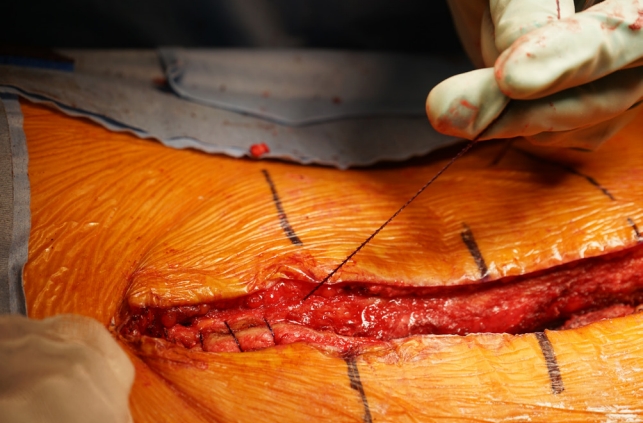
Fascia layer closure using a unidirectional barbed suture. Dense and uniformly arrayed unidirectional barbs have a locking property to the surrounding tissue. Due to its configuration, barbed sutures can tightly hold the approximated tissue without the need for continuous application of tensile force.

Subcutaneous layer closure using a bidirectional barbed suture. Two surgeons begin the suture from the center of the wound and proceed to the opposite directions. Note that the tension applied on the suture in opposite directions approximates the wound in between.
A self-adhering mesh system is a user-friendly wound closure method involving mesh materials with adhesive backing. It offers easy application, secure closure, breathability, flexibility, and reduced scarring. The mesh directly adheres to the skin or wound edges, providing mechanical support and tension to promote proper healing [16-18]. Polymeric glue, also known as a tissue adhesive or surgical glue, is a noninvasive alternative to traditional sutures or staples for wound closure. It is applied topically and forms a strong bond, eliminating the need for invasive closure methods. Polymeric glue has a rapid application and biocompatibility, provides flexibility, and is associated with minimal scarring [18-20].
Therefore, we evaluated the safety and effectiveness of a self-adhering mesh system, polymeric glue, and knotless barbed sutures for wound closure in multilevel and revisional posterior spinal surgery to broaden the evidence and knowledge regarding their clinical use.
MATERIALS AND METHODS
The single-center, retrospective, matched cohort study was approved by the appropriate Institutional Review Board of Seoul National University Bundang Hospital (WC-2019-15), and the informed consent was waived. From the electronic medical system, we identified patients (1) who underwent multilevel, defined as at least 3 levels, or revisional posterior spinal surgery between August 2013 and March 2021; (2) who were followed up for at least 3 months; and (3) whose data regarding wound closure time and total operation time were available. We excluded patients who underwent cervical spinal surgery and included those who underwent thoracolumbar surgery. Patients who underwent for fascia and subcutaneous tissue approximation using knotless barbed sutures and skin closure using a self-adhering mesh and polymeric glue were selected as the experimental group (Fig. 5). Furthermore, within the same patient pool, the control group was selected using a 1 to 1 matching for sex and number of segments operated (with 1 level of difference tolerated) who underwent conventional wound closure using Vicryl interrupted sutures and skin staplers.
Wound closure in all patients was performed by 2 fellowship-trained spine surgeons with at least 1–2 years of experience at a single academic institution. For patients who underwent surgery in different years, other fellow surgeons performed wound closure. Each surgeon received sufficient training before using the barbed suture, and the risk of microperforation was prevented by double gloving during the suturing.
Baseline demographic data including age, sex, body mass index, height, smoking status, and diabetes were collected. The wound closure time and total operation time were measured intraoperatively and recorded. Main operation time was defined as the value obtained by subtracting the wound closure time from the total operation time. Pre- and postoperative 3-month back pain assessments using the visual analogue scale, hospitalization days, and postoperative wound complications were also retrieved retrospectively from electronic records. Postoperative wound complications were defined as wound dehiscence or surgical site infection within 3 months of the surgery. We also checked the outpatient medical records for skin complications such as contact dermatitis.
Patients were subdivided into 3 groups (3–5, 6–9, and ≥ 10 levels) to evaluate the difference in wound closure time and total operation time between the groups stratified by surgical level. Furthermore, patients who underwent revisional thoracolumbar surgery in the experimental and control groups were included in the subgroup analysis.
The distribution of continuous variables was assessed for normality using the Shapiro-Wilk test, and then parametric or nonparametric tests were performed using the paired t-test or Wilcoxon signed-rank test, respectively. Parameters did not satisfy the normality requirement were presented as median (interquartile range) and were analyzed using the Wilcoxon signed-rank test for between-group differences. Significance level was set at 0.05, and statistical analyses were performed using IBM SPSS Statistics ver. 29.0 (IBM Co., Armonk, NY, USA).
RESULTS
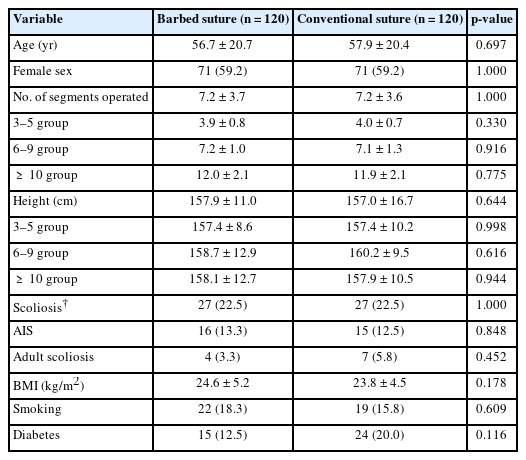
We included 120 patients each in the experimental (barbed suture) and control (conventional suture) groups (Table 1). There were no significant differences between groups regarding sex, age, height, body mass index, number of scoliosis, and diabetes mellitus.
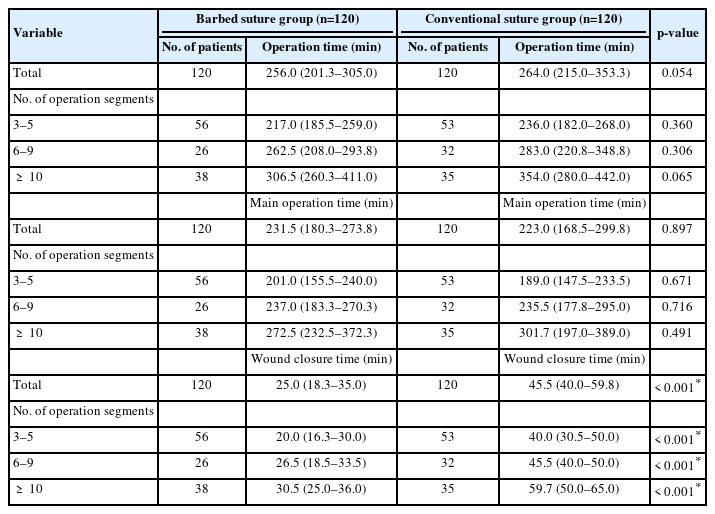
Each group was divided into 3 subgroups according to the number of operated spinal levels: 3–5, 6–9, and ≥ 10 (Table 2). The difference in total operation time, main operation time, and wound closure time for each corresponding subgroup was analyzed. All corresponding subgroups showed significantly less wound-closing time in the barbed suture group than in the conventional suture group (3–5 levels of segments; 20.0 (16.3–30.0) minutes vs. 40.0 (30.3–50.0) minutes, p<0.001; 6–9 level of segments; 26.5 (18.5–33.5) minutes vs. 45.5 (38.0–50.0) minutes, p<0.001; ≥ 10 levels of segments; 30.5 (25.0–36.0) minutes vs. 59.7 (50.0–65.0) minutes, p<0.001).
Furthermore, the total operation time, main operation time, and wound closure time for the revisional operation was analyzed (Table 3). Among the patients, 46 patients in the barbed suture group and 23 in the conventional suture group underwent revisional surgery. Including operation time, the wound-closing time showed statistically significant differences with more time consumption for the conventional suture subgroups. Moreover, the barbed suture group had a significantly shorter time reduction in operation time and wound closure time. The ratio of wound closure time to operation time in the revision surgery group was approximately 16% in the conventional suture group and 9% in the barbed suture group.
The perioperative clinical outcome parameters were also measured and compared (Table 4). Both groups showed no significant differences in postoperative back pain scores, hospitalization days, and postoperative wound complications. In the barbed suture group, 3 of 4 patients had wound dehiscence (48, 58, and 64 days after surgery), and one had surgical site infection. In the conventional suture group, 2 of 3 patients had wound dehiscence (30 and 37 days after surgery), and 1 patient developed a surgical site infection. We also found that 1 of 120 patients (1.7%) treated with the 2-octyl cyanoacrylate and polymeric glue acquired contact dermatitis during the follow-up period.
DISCUSSION
Our study demonstrated the efficacy and safety of knotless barbed sutures for revision or long-level posterior spine surgery. We found that compared to using conventional sutures, using barbed sutures significantly decreased wound closure time, which is associated with decreased total operation time, and showed comparable perioperative clinical outcomes. In posterior spinal surgery, wound closure is conventionally performed separately using interrupted suture techniques separately for each layer. Although this is a familiar method, it has inherent disadvantages regarding wound closure strength and time. Skin wound from revision surgeries have scar tissue that requiring stronger tension than the normal skin which is why wound suture in revisional surgeries require more time for close. Moreover, wound closure time might increase proportionately with the increasing number of operated segments using the interrupted suture technique. Wound dehiscence and surgical site infection are major concerns as they usually involve reoperation, implant failure, or prolonged hospital stays with devastating results sometimes. Multilevel or revisional posterior spinal surgeries are especially concerning as it requires more wound closure time than short-level or virgin spinal surgeries; furthermore, they are associated with higher postoperative wound complication rates [2,3,21].
In contrast to interrupted sutures, barbed sutures can firmly hold the tissue in place without continuous tension being applied [22]. These advantages relieve stress and reduce the time required to close the wound at every step of suturing. Furthermore, owing their favorable biomechanical properties, they have been used for tendon repair and veterinary medicine [23-26]. Several studies have demonstrated the safety and efficacy of this novel wound closure material, but evidence in thoracolumbar spinal surgery is scarce [27-32].
Wound closure time for all surgical level subgroups was measured and compared (Table 2). It was shown that all segmental subgroups of barbed suture had significantly shorter wound closure time than the conventional suture group. Furthermore, there were no significant differences in the main operation time between the subgroups. The similar main operation time in relation to shorter total operation time which demonstrates the advantages of barbed sutures in terms of the closing time, especially when more spinal levels are involved, in which the operation time was significantly shorter in the barbed suture group than in the conventional suture group although no significant difference in the main operation time was observed between the groups. Clearly, the group employing barbed suture materials for wound closure significantly shortened the wound closure time compared to the group using conventional sutures, and they also reduced the overall operation time.
Despite the shorter wound closure time, there were no differences in the measured perioperative outcomes between the 2 groups (Table 4). Both groups had no significant difference in postoperative back pain scores after 3 months and hospitalization days. Notably, the barbed suture group was comparable in terms of postoperative wound complications within 3 months, reflecting the suture material’s clinical safety and strength. Interestingly, we found that wound problems occurred later in the barbed suture than in the conventional group. The reason is that the tensile strength of the barbed suture is maintained at a high level; therefore, wound issues will emerge in the latter. There are not enough wound problem cases between groups; more data is needed for generalization. The number of patients with contact dermatitis in the barbed suture with self-adhering mesh and polymeric glue was minimal, according to review of medical records. From this, it can be assumed that the self-adhering mesh and polymeric glue is biocompatible with the study participants’ postoperative wound. Additionally, wound complexity may potentially impact wound closure time. However, the number of scoliosis patients was the same in both groups, and there was no significant difference (27 patients in each group). Although precise measurements did not take, it can be inferred that there was no significant difference in wound complexity between the 2 groups in our research.
Our study had several limitations. First, the total operation time was multifactorial and also affected by the time required for wound dissection and main procedures, such as screw insertion, osteotomies, or interbody fusion. However, we found no significant difference between the 2 groups when comparing the main operation time for each group. Consequently, it was confirmed how the difference in wound closure time between the 2 groups had a significant effect on efficiently reducing the surgical time by using a barbed suture. Second, this is a single-center retrospective study. However, it also had the advantage of providing valuable information because of matched analysis of the experimental and control groups, both of which included more than 100 patients.
We expect that our study will extend our knowledge regarding the safety and efficacy of this novel suture material for posterior spinal multilevel surgery.
CONCLUSION
Compared to using the conventional interrupted Vicryl suture, using the knotless barbed suture decreased the time and effort to close surgical wounds in posterior spinal surgeries with comparable safety and clinical outcomes. Our study results support the use of barbed sutures, especially in multilevel and revisional spinal surgeries.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This work was supported by an Investigator-Initiated Study Grant (No. WC-2019-15) from Johnson and Johnson Medical.
Author Contribution
Conceptualization: SJH; Data Curation: JM, SJH, JKL, SA; Formal Analysis: JM, SJH, JKL; Investigation: JM, SJH, JKL, SA; Project Administration: JM, SJH, JKL, SA, KJK; Writing – Original Draft: JM, JKL, SA; Writing – Review & Editing: JM, SJH, JKL, SA, KJK.