Traditional Dual Growing Rods With 2 Different Apical Control Techniques in the Treatment of Early-Onset Scoliosis
Article information
Abstract
Objective
Based on traditional dual growing rods (TDGR), apical control techniques (ACTs) were introduced as adjuvant procedures to improve deformity correction at the apex segment in the treatment of early-onset scoliosis (EOS). We aimed to explore whether TDGR+ ACTs have different indications, attain more deformity correction, have negative effects on spinal growth, and have different complications.
Methods
Between 2004 and 2019, a retrospective study of EOS patients treated with TDGR with or without ACTs was conducted and divided into 3 groups: TDGR group; hybrid technique (HT) group: Vertebrectomy/hemivertebrectomy with short fusion and TDGR; ACPS group: apical convex control pedicle screws (ACPS) and TDGR. Demographic, radiographic parameters, clinical outcomes, complications, and revisions were analyzed and compared.
Results
Seventy-eight EOS patients were enrolled. The preoperative main curve was the largest in the HT group. ACPS group had the smallest residual curve (19° ± 8.9°) and apical vertebral translation (12.0 ± 9.0 mm) at the latest follow-up, followed by the HT group (30° ± 17.4°, 22.1 ± 13.4 mm) and TDGR group (30° ± 13.2°, 32.8 ± 17.1 mm). ACPS group had the largest T1–12 height and T1–S1 height after index surgery. Complications and revisions in the ACTs groups was lower than the TDGR group. Scoliosis Research Society-22 self-image questionnaire was superior in the ACPS group.
Conclusion
According to our intermediate results, TDGR+ACTs could improve correction ability of apex deformity. ACTs had little deleterious effects on spinal height during the lengthening procedures, with a lower complication rate than TDGR. TDGR+ACTs might be a supplemental option for suitable EOS patients.
INTRODUCTION
Early-onset scoliosis (EOS) is one of the most challenging deformity in spine surgery, as patients with EOS still have great and important growth potential of the lung, thorax and spine [1]. Surgeons must consider the growth of these important structures when treating these children. Early long fusion for EOS patients who are far from bone mature should be avoided to prevent iatrogenic thoracic insufficiency syndrome [2]. Many growthfriendly techniques have been introduced to correct the deformity while allowing growth of the spine and thorax [3-8], and traditional dual growing rods (TDGR) are the most widely used procedures.
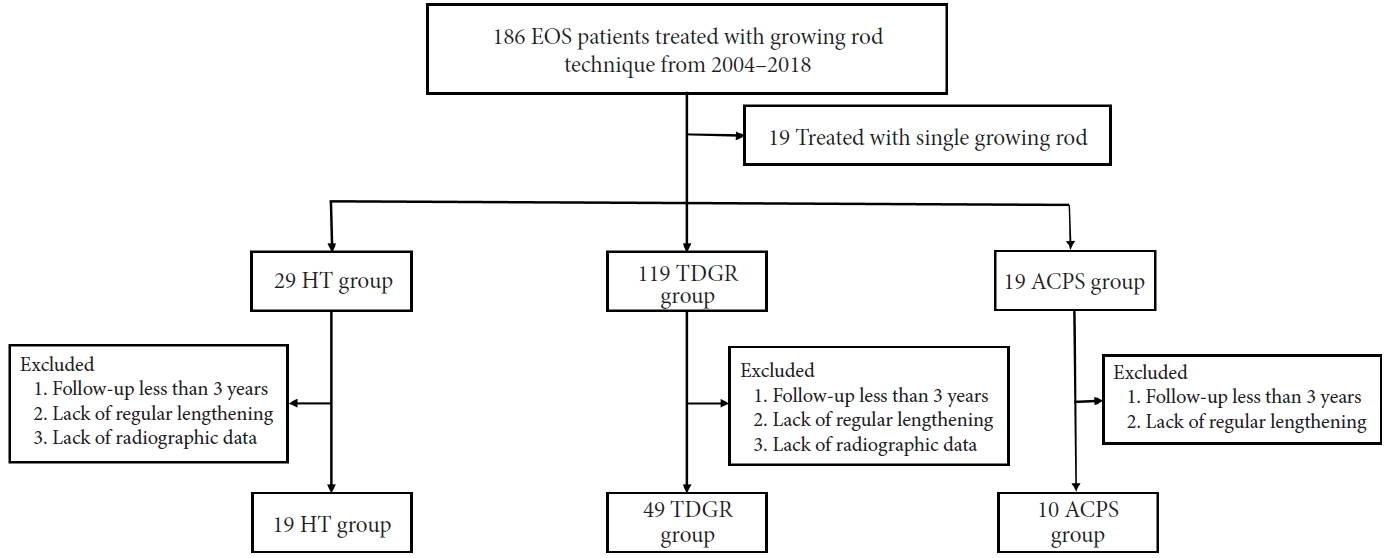
The clinical outcomes of TDGR have been well described [3,9-12]. However, there are still some challenges for TDGR, including repeated anesthesia and surgeries, large residual deformities, limited apex control, and a high risk of complications (Fig. 1) [5,9,13-16]. Large residual deformities and limited apex control due to the biomechanical limitations of TDGR may contribute to the 3-dimensional chest and spinal deformity, especially narrowing and rigidity of the convex hemithorax as the spine penetrates into the convex chest because of coronal translation, axial rotation and lordosis. To address this issue, surgeons reported several techniques to improve apical control of the curve when using growth-friendly techniques, including Luque-Trolley technique [17], Shilla technique [18,19] and TDGR combined with apical control techniques (ACTs). Wang et al. [20] and Johnston [14] building on the experience of TDGR, introduced 2 different ACTs, hybrid technique (HT, apical vertebrectomy/hemivertebrectomy and short fusion) and apical control pedicle screws (ACPS), aiming to improve correction of the apical deformity and decrease complications. As a relatively new technique, the results of TDGR+ACTs remain unclear. A prior study conducted a comparative study of HT and TDGR techniques on congenital EOS (CEOS) patients [21], and the preliminary results showed better deformity correction and fewer complications in the HT group. However, CEOS were different from EOS caused by other etiologies, some type of CEOS may progress quickly at a very young age, which is prone to result in a more severe and rigid deformity than other etiologies [22,23]. Besides, congenital scoliosis is often associated with abnormalities in other systems derived from mesoderm, among which spinal cord, cardiac and genitourinary tract abnormalities are commonly concomitant [24], which may also cause a potential impact on clinical outcomes.

A case of traditional dual growing rods (TDGR) to treat early-onset scoliosis. (A) A 3-year-old girl with severe congenital deformities caused by multiple segmentation failures in the thoracic spine. (B) TDGR was applied to correct the deformity while allowing for the growth of the spine and thorax. (C, D) However, the residual spine and chest deformities were large, and a “Windswept” thorax causing by apical coronal translation, axial rotation and along lordosis still existed during lengthening procedures at 6 years. High-grade osteotomy such as a 3-column osteotomy with increased complications in a stiff spine may be mandatory to correct residual spine and chest deformities.
We therefore compared HT, ACPS and TDGR in EOS patients, and asked whether apical control technique (1) have different indication, (2) attain more deformity correction, (3) have negative effects on spinal growth, and (4) have different complications?
MATERIALS AND METHODS
1. Participants and Demographics
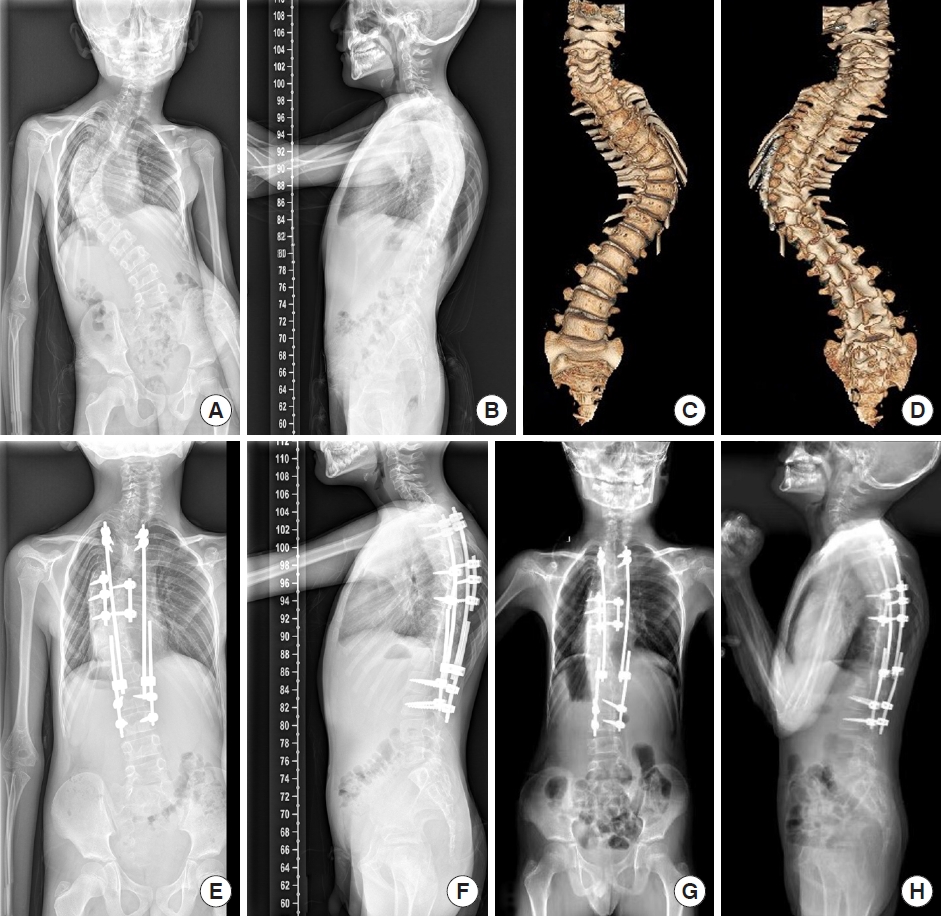
Following Institutional Review Board approval of Peking Union Medical College Hospital (K2138), a single-center, retrospective study was conducted. Patients diagnosed with EOS and underwent growing rod technique between March 2004 and December 2019 were considered potentially eligible for recruitment in this study. A total of 186 EOS patients treated with growing rod technique, 10.22% (19 of 186) of patients treated with single growing god were excluded. Based on the surgical method used, the patients were divided in the TDGR (n= 119), HT (n= 29), and ACPS (n= 19) group. A flowchart showed the recruitment process of the current study (Fig. 2).
A flowchart showed the recruitment process of the current study. EOS, early-onset scoliosis; HT, hybrid technique; TDGR, traditional dual growing rods; ACPS, apical control pedicle screws.
In the TDGR group, 21.01% (25 of 119) patients short of 3-year follow-up was excluded, 12.61% (15 of 119) patients without regular follow-up were excluded, and 25.21% (30 of 119) patients lack of preoperative and/or postoperative radiographic data were excluded, leaving 41.18% (49 of 119) for analysis.
In the HT group, 13.79% (4 of 29) patients short of 3-years follow-up was excluded, 17.24% (5 of 29) patients without regular follow-up was excluded, and 3.45% (1 of 29) patients lack of preoperative and/or postoperative radiographic data was excluded, leaving 65.52% (19 of 29) for analysis.
In the ACPS group, 26.32% (5 of 19) patients short of 3-years follow-up was excluded, 21.05% (4 of 19) patients without regular follow-up were excluded, leaving 52.63% (10 of 19) for analysis.
2. Treatment Algorithm and Reference
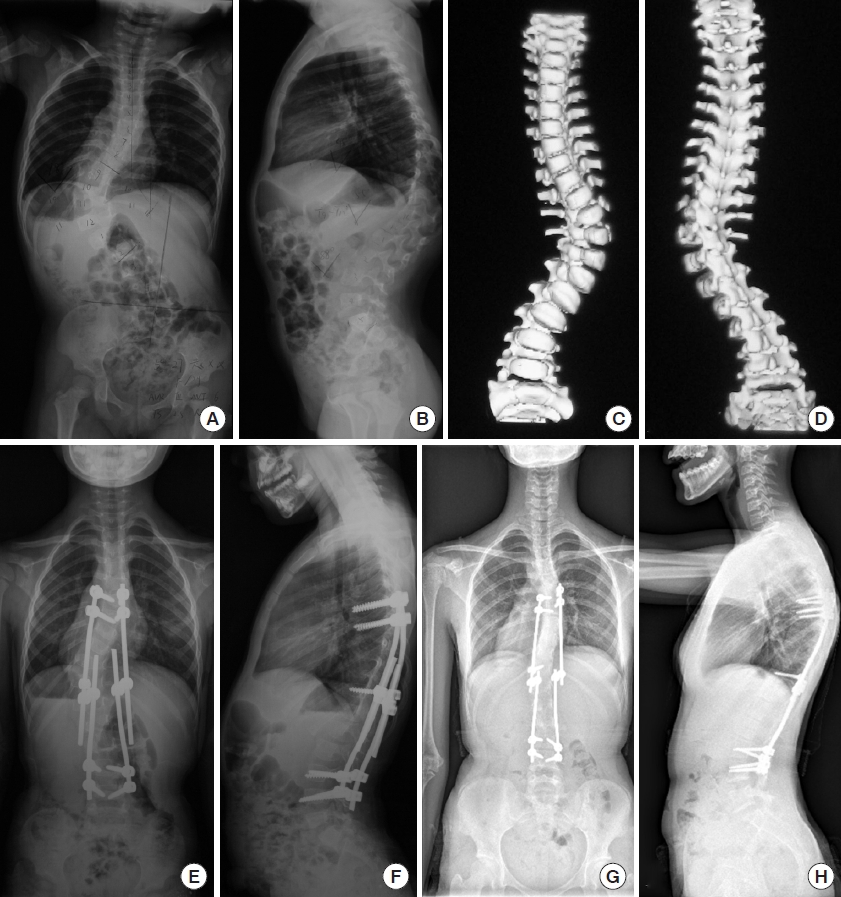
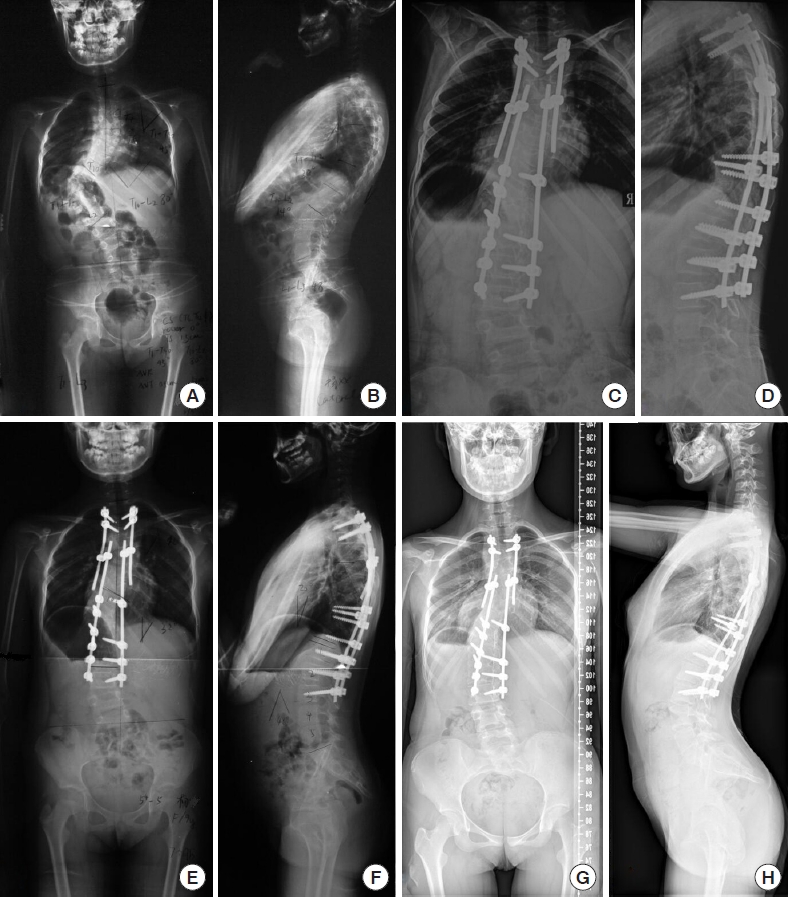
Both TDGR and TDGR+ACTs were used to treat EOS patients in our institution. In principle and practice, most TDGR was indicated for: (1) failure of treatment with bracing or casting, (2) curve more than 60°, (3) ages younger than 10 years old, (4) diagnose with all etiology [25]. ACTs were introduced in recent years, as relatively novel technologies, no clear indication has been proposed or confirmed. We used HT [20] as ACT in patients with rigid and severe curves (most were congenital formation or segmentation failures at apex segment) (Fig. 3) while using ACPS described by Johnston [14,15] in relatively flexible curves (mostly had flexible discs at apex segments, such as idiopathic, syndromic or neuromuscular scoliosis) (Fig. 4). The convex supine bending film was also used to evaluate the curve flexibility in all patients and as a reference for choosing the ACTs.
A case of hybrid technique (HT) to treat early-onset scoliosis. (A–D) A 7-year-old boy with severe congenital early-onset scoliosis due to multiple formation and segmentation failures. HT was applied. T9 vertebral column resection and short fusion were performed. Growing rods were implanted with a 6-rod technique from T2–L3. (E, F) The correction of the main curve was good after index surgery and was well maintained. (G, H) Significant growth of the spine and thorax was observed after 3 lengthening procedures. T1–T12 height: 12.1 cm to 14.2 cm to 17.7 cm; T1–S1 height: 21.3 cm to 26.6 cm to 33.1 cm (pre- to post- to follow-up).
A case of ACPS to treat early-onset scoliosis. (A–D) A 3-year-old girl with idiopathic scoliosis with severe rotation and mild kyphosis. ACPS was used at the apex, and growing rods were implanted with a 4-rod technique from T6–L4. (E, F) Good correction was obtained immediately after the index surgery. (G, H) The residual spine and chest deformities were mild, and significant growth of the spine and thorax was observed after 8 lengthening procedures in 8 years. The T1–T12 height: 15.1 cm to 17.5 cm to 21.2 cm; T1–S1 height: 23.0 cm to 28.0 cm to 34.4 cm (pre- to post- to follow-up).
3. Measurement of Study Outcomes
Data for all patients were reported at the preoperative, postoperative, and latest follow-up visits within the study period. To answer our question, data included demographic information, radiographic parameters (corrective parameters of scoliosis, spinal growth parameters) [26], complications and revision procedures was measured. All radiographs were evaluated blindly by 2 well-trained attending spine surgery surgeons. A Scoliosis Research Society (SRS)-22 questionnaire was used as an outcome measure at the latest follow-up in patients who were old enough to complete the questionnaire.
4. Statistical Analyses
Analyses were performed using IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA). Continuous variables were presented as mean ± standard deviation. All continuous variables were tested for normal distribution, using t-test for data that conformed to normal distribution and nonparametric test for data that did not conform to normal distribution (Kruskal-Wallis test for comparison among 3 groups and Mann-Whitney U-test for comparison between the 2 groups). For categorical variables, the chi-square test and Fisher exact test were used. Comparisons at different time points were analyzed. A p-value of < 0.05 was considered as statistically significant.
RESULTS
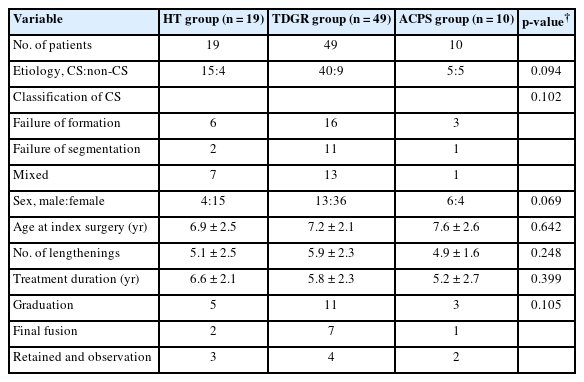
Seventy-eight patients were finally enrolled, including 49 patients in the TDGR group, 19 patients in the HT group and 10 patients in the ACPS group. The etiology of congenital scoliosis was 15 of 19 in the HT group (6 with formation failure, 2 with segmentation failure, 7 with mixed type), 40 of 49 in the TDGR group (16 with formation failure, 11 with segmentation failure, 13 with mixed type) and 5 of 10 in the ACPS group (3 with formation failure, 1 with segmentation failure, 1 with mixed type). The curve flexibility in convex bending film was 52.4%± 10.7% in the ACPS group, 30.7% ± 14.4% in the TDGR group, and 21.3%± 7.6% in the HT group. There were no differences in the mean age, number of lengthening or lengthening treatment duration (Table 1). Nineteen patients graduated from lengthening procedures, 10 of them received final fusion surgery and 9 just retained growing rods under regular follow-up.
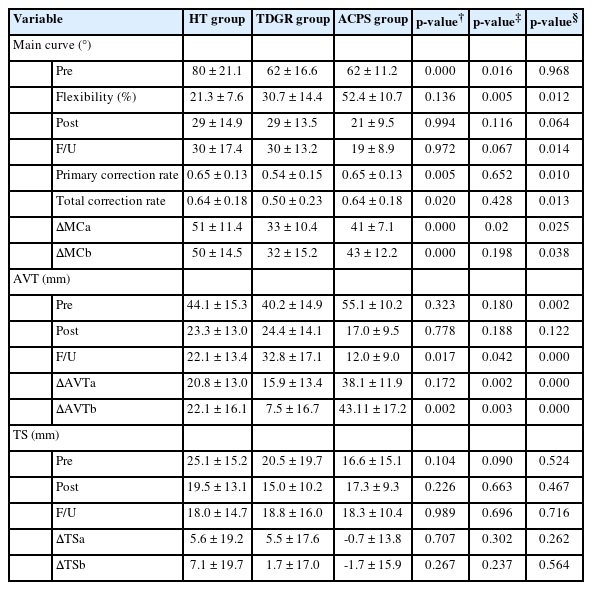
1. Correction of the Deformity
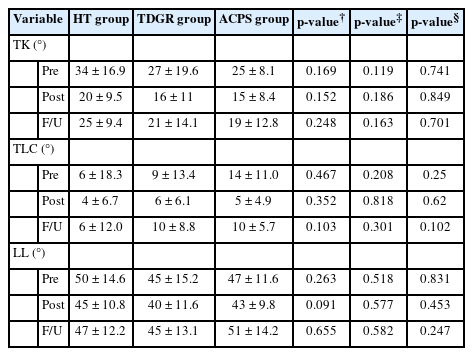
The preoperative main curve was the largest in the HT group among 3 groups, while the preoperative apical vertebral translation (AVT) was larger in the ACPS group. Patients in the ACPS group had the smallest residual curve (19°± 8.9°) and AVT (12.0 ± 9.0 mm) at the latest follow-up, followed by the HT group (30° ± 17.4°, 22.1 ± 13.4 mm) and TDGR group (30° ± 13.2°, 32.8± 17.1 mm). The correction rate of the main curve at the latest follow-up was comparable between the HT (64%) and ACPS (64%) groups and was higher than that of the TDGR group (50%) (Table 2). No differences were found in sagittal parameters among the 3 groups after index surgery and during follow-up (Table 3).
2. Gain of Spinal Height
Patients in the ACPS group had the largest T1–12 height and T1–S1 height before and after index surgery, while the parameters in the other 2 groups were comparable at any observation time. No significant differences were found in the annual growth of T1–12 height and T1–S1 height during the lengthening procedures in the 3 groups. Preoperative space available for lung (SAL)27 was smallest in the HT group. However, no differences were found in SAL among the 3 groups at either the postindex surgery or latest follow-up time points (Table 4).
3. Complications and Patient-Reported Clinical Outcomes
Sixteen complications occurred in 10 patients in the HT group (12 mechanical-related complications, 2 wound problems, 1 dural tear, and 1 neurological deficit; Fig. 5), 71 complications occurred in 32 patients in the TDGR group (65 mechanical-related complications, 5 wound problems, and 1 dural tear), and 5 complications occurred in 4 patients in the ACPS group (4 mechanical-related complications and 1 wound problems). The mean number of total complications, mechanical-related complications and unanticipated revision surgeries was comparable between the HT group and the ACPS group and was lower than that of the TDGR group. Thirty-eight patients could complete the SRS-22 questionnaire at the latest follow-up, and SRS-22 self-image score was superior in ACPS group among the 3 group at the latest follow-up, while the other 2 group were comparable (Table 5).
Patients with a complication of neurological deficits. (A, B) A 9-year-old girl with severe and rigid congenital early-onset scoliosis without preoperative neurological deficits. She underwent HT surgery. The motor-evoked potential loss (more than 80%) was shown when we performed T11 hemivertebrectomy. We chose to complete the osteotomy quickly to control bleeding, raised mean arterial pressure and used methylprednisolone. After that, the signal partially recovered from the lowest point. The patient showed transient motor function deficits of the left lower limbs, and recovered to preoperative status at 6 months. The correction of the main curve was good after index surgery (C, D) and was well maintained (E–H).
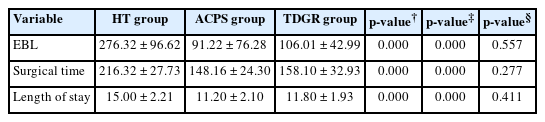
4. Outcomes of Surgical Variables
The mean surgical time of index surgery was 216.32± 27.73 minutes in the HT group, 148.16± 24.30 minutes in the TDGR group and 158.10± 32.93 minutes in the ACPS group. The estimated blood loss was 276.32± 96.62 mL in the HT group, 91.22± 76.28 mL in the TDGR group and 106.01 ± 42.99 mL in the ACPS group. The length of stay was 15.00± 2.21 days in the HT group, 11.20± 2.10 days in the TDGR group and 11.80± 1.93 days in the ACPS group. One positive intraoperative neurological monitoring event occurred in the HT group (Table 6).
DISCUSSION
TDGR is the most widely used distraction-based growth-friendly technique for EOS [28]. Due to biomechanical limitations of simple distraction through end-vertebral anchors, it may only partially control the 3-dimensional spinal and chest deformity [29]. Therefore, ACTs were introduced to improve the control of the apical deformity when TDGR was applied. Different ACTs were applied in different EOS patients, and evaluation of apical deformity flexibility should be the key consideration when choosing ACT. Johnston used convex control pedicle screws to improve deformity correction by direct apex derotation and translation while allowing for concave growth [14,15]. They enrolled patients for the ACPS technique included: Large curves and short T1–12 segments (range, 8.5–14.4 cm) in patients 5 years of age or less, with significant axial plane deformity. However, direct apex derotation and translation with ACPS could only be used in relatively flexible curves, as this technique could hardly work in patients with angular and rigid deformity, such as CEOS with multiple formation and segmentation failures. ACPS might be best indicated for patients whose apical deformity is flexible with relatively normal discs, without multiple formation or segmentation failures. The ACPS group is treated with a more flexible curve in our institution, with an average flexibility of 52.4%. Therefore, we propose the indication for the ACPS technique: (1) failure of treatment with bracing or casting, (2) ages younger than 10 years old, (3) degree of curvature of more than 60° with large AVT and AVR at the apical segment, (4) flexible disc at the apical segment. However, based on the current results, we are unable to quantify AVT and AVR. Furthermore, as previously reported, the TDGR results for CEOS were not as good as those caused by other etiologies [12,30]. HT technique was first reported by Wang et al. [2]0 in 2014, and by apical vertebrectomy/hemivertebrectomy and short fusion, the apical rigid, severe deformity at apex segment could be better addressed. The indication was also based on the TDGR technique, and the ideal candidate for the HT technique was: severe and rigid EOS at the apical segment with a long sweeping curve, which has pronounced asymmetric growth potential around the apex. In this study, we also followed and standardized the indication as follows: (1) failure of treatment with bracing or casting, (2) ages younger than 10 years old, (3) severe and rigid deformity at the apical segment with a long sweeping curve. As the high-grade osteotomy needed advanced technique and increased surgical difficulty, we only used the HT technique to treat severe and rigid EOS patients (most of them were CEOS). We have developed a preliminary workflow of ACT choice for the treatment of EOS (Fig. 6), and further study by setting flexibility thresholds may help to develop indications for different ACTs.
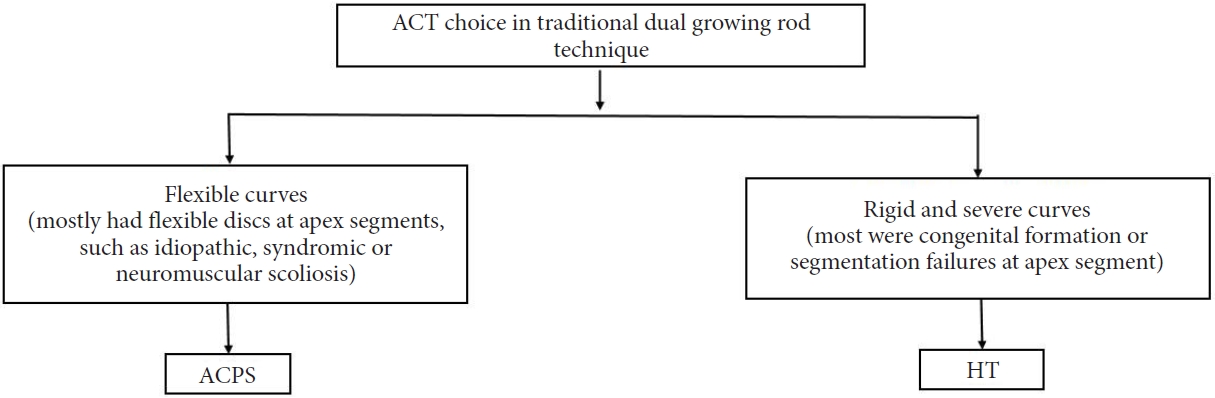
A workflow of apical control techniques (ACTs) selection in our institution. HT, hybrid technique; ACPS, apical control pedicle screws.
Attaining a better deformity correction was a major surgical goal for EOS treatment. Alanay et al. [31] and Demirkiran et al. [32] reported the effectiveness of posterior convex growth arrest with pedicle screws and concave distraction with traditional growing rods or magnetically controlled growing rods for the treatment of patients with long sweeping congenital curves. The correction of the main curve at the latest follow-up was about 41.3% (60.5° to 35.5°), and spine growth was achieved during concave distraction. Three column osteotomies may be needed for patients with severe and rigid EOS to gain mobility for correction. Wang et al. [20] introduced HT of apical vertebrectomy/hemivertebrectomy and TDGR for more severe, non-flexible deformity. In Wang’s cohort of 7 patients treated with HT, the mean curve improved from 81.4° to 41° [20]. Their preliminary results were supported by Bas et al. [33] and Sun et al. [34]. Our study found that HT had the best curve magnitude correction in patients with the most severe and rigid preoperative main curve. The correction rate of the main curve was comparable in the HT group and ACPS group immediately after index surgery and at the latest follow-up. Patients in the ACPS group had the smallest residual curve and AVT at the latest follow-up.
Another major concern is whether ACT, especially the HT technique, which needs apical vertebrectomy/hemivertebrectomy and fusion, has negative effects on spine growth. Thompson found that apical segmental fusion within growing rods could exert a negative influence on spine growth [11]. Wang et al. [20] and Sun et al. [34] reported that the growth of T1–S1 height in their cohort of patients treated with HT was similar to that reported of patients treated with TGR only. In the current study, the gain of T1–12 and T1–S1 height after index surgery was greater in the ACPS and HT groups, while T1–12 and T1–S1 height gain was greater during the lengthening procedures in the TDGR group. Although there were no significant differences, the mean annual growth of T1–12 and T1–S1 height was lower in patients in the HT and ACT groups than in those in the TDGR group. Both HT and ACPS may have slightly negative effects on spine growth during lengthening procedures, but these negative effects could be countered by more spine height gain during index surgeries in both groups. No significant differences were found in the T1–12 and T1–S1 heights among the 3 groups at the latest follow-up.
TGR is inherently prone to complications due to biomechanical limitations. The complication rate of TGR could be more than 50%. Mechanical failures are the most common complications [3,9,12,13,30]. Helenius et al. [13] found that severe EOS was associated with larger residual deformity and more complications than moderate EOS when treated with TGR. Patients with a severe and rigid apical curve may have large residual deformities when treated with TDGR [35]. The enormous asymmetric growth potential around the residual deformities may contribute to an increased risk of complications of the TGR for patients with CEOS [36,37]. HT was introduced to address these issues. During the index surgery of HT, apical vertebrectomy/hemivertebrectomy and short segmental fusion could powerfully improve the correction of the major curve while eliminating the asymmetric growth potential around the apex. Furthermore, additional pedicle screws used in patients treated with HT and ACPS could provide more fixation points to improve the stability of TDGR. Wang et al. found that the correction of the main curve was 50.7%, and no complications occurred [20]. In the study of Sun et al. [34], the correction of the main curve after the index surgery was 57.2%, and 2 of 13 patients developed 2 complications. In the current study, patients in the HT and ACPS groups had fewer complications, mechanical failures, and anticipated revision surgeries. TDGR+ACTs may help to decrease the risk of complications, especially mechanical failures.
There were several limitations in this study. First, this was a retrospective study and suffered from treatment selection bias; Second, the etiology of EOS was not unified in this study; Third, ACT was relatively more aggressive and not widely used, so the patient samples in the ACT groups were relatively small, and most patients in both groups were still skeletally immature and still in the treatment period. Larger studies of such patients who graduate from lengthening procedures will be critical in fully understanding the strengths, weaknesses, and indications of the procedures. However, understanding the intermediate follow-up period offers valuable information on the advantages of TDGR+ACTs for surgeons and patients who may be candidates for these techniques.
CONCLUSION
In summary, ACTs, including HT and ACPS, could improve the correction of TDGR while decreasing the risk of complications and unanticipated revision surgeries. HT and ACPS did not have deleterious effects on the gain of T1–T12 and T1–S1 height during the lengthening procedures. TDGR+ACTs may be a supplemental option for patients with EOS, especially those with a large apical deformity. HT is indicated for severe and rigid curve, while ACPS is indicated for flexible curve. Long-term follow-up is mandatory to evaluate the final results of ACTs.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This work was supported by the National Natural Science Foundation of China (81171673, 81972037 and 81902178), Beijing Natural Science Foundation (No. L192015).
Author Contribution
Conceptualization: SW, JZ; Formal Analysis: SW, YZ, YD; Investigation: YZ, SW; Methodology: SW, GL; Project Administration: JZ, JS; Writing – Original Draft: SW, YZ; Writing – Review & Editing: NW, YY, JZ.