Screw Insertional Torque Measurement in Spine Surgery: Correlation With Bone Mineral Density and Hounsfield Unit
Article information
Abstract
Objective
Achieving successful fusion during spine surgery is dependent on rigid pedicle screw fixation. To assess fixation strength, the insertional torque can be measured during intraoperative screw fixation. This study aimed to explore the technical feasibility of measuring the insertional torque of a pedicle screw, while investigating its relationship with bone density.
Methods
Thoraco-lumbar screw fixation fusion surgery was performed on 53 patients (mean age, 65.5 ± 9.8 years). The insertional torque of 284 screws was measured at the point passing through the pedicle using a calibrated torque wrench, with a specially designed connector to the spine screw system. The Hounsfield units (HU) value was determined by assessing the trabecular portion of the index vertebral body on sagittal computed tomography images. We analyzed the relationship between the measured insertional torque and the following bone strength parameters: bone mineral density (BMD) and HU of the vertebral body.
Results
The mean insertion torque was 105.55 ± 58.08 N∙cm and T-score value (BMD) was -1.14 ± 1.49. Mean HU value was 136.37 ± 57.59. Screw insertion torque was positively correlated with BMD and HU in whole patients. However, in cases of osteopenia, all variables showed very weak correlations with insertional torque. In patients with osteoporosis, there was no statistically significant correlation between BMD and torque strength; HU showed a significant correlation.
Conclusion
The insertional torque of screw fixation significantly correlated with bone density (BMD and HU). HU measurements showed greater clinical significance than did BMD values in patients with osteoporosis.
INTRODUCTION
Spinal fusion surgery is a common technique for the treatment of various spinal disorders. Although the procedure is associated with strong and reliable anchoring of pedicle screws, screw loosening can result in fusion failure, loss of correction, and need for revision surgery. These complications are particularly problematic in patients with poor bone quality [1,2].
Biomechanical studies have shown that the pullout strength of a pedicle screw is affected by various factors, including bone mineral density (BMD), osteoporosis, cortical fixation, pedicle morphology, screw orientation, and screw-thread area [3-8]. Poor fixation can lead to micromovements, fibrous encapsulation, and screw loosening during fusion [9,10]. Screw fixation strength can be assessed objectively or subjectively during intraoperative screw fixation.
However, to date, these crucial factors have mainly been evaluated based on the operator’s subjective perception and feeling of bone resistance during screw insertion. However, this approach relies on subjective tactile sensations and depends heavily on the skill and experience of the surgeon. An objective and a better predictive method for assessing fixation strength is, therefore, required to achieve successful fusion and favorable clinical outcomes.
Previous biomechanical studies have reported a significant correlation between pedicle screw fixation and BMD as well as a significant association between the torque needed for screw insertion and its pullout strength [11-14]. However, a consistent relationship between these 2 factors has not been established [15]. This discrepancy may be attributed to variations in the mechanical response of the trabecular bone to forces exerted during screw insertion.
Recently, a new and reliable alternative tool for assessing bone density was developed using Hounsfield units (HU) obtained using computed tomography (CT). An existing study showed that HU values were positively correlated with vertebral compressive strength and BMD, making them valuable indicators of bone density [16]. Subsequent studies have shown that lower HU values of the vertebral body are associated with nonunion, cage subsidence, and adjacent segment fractures after spinal fusion [17-19]. This present study aimed to explore the technical feasibility of measuring the insertional torque of screws and to establish a relationship between insertional torque and bone density (BMD and HU). Additionally, a subgroup analysis of the patients based on their BMD T scores was conducted to determine whether the correlation exhibited any changes.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board of St. Vincent’s Hospital, The Catholic University of Korea (2022-3531-0001). All methods were performed in accordance with the relevant guidelines and regulations by including a statement in this section. This study included 53 consecutive patients (20 men and 33 women) who underwent thoracolumbar spine surgery, including pedicle screw fixation, between April 2022 and January 2023. The patients’ ages ranged from 37 to 88 years, with a mean age of 65.5 ± 9.8 years.
Patients who underwent dual-energy x-ray absorptiometry (DEXA) scans of the femoral neck and lumbar vertebrae as well as CT scans of the affected vertebrae within 2 months before surgery were included. In addition, postoperative CT was performed immediately after surgery. Patients with a history of spinal instrumentation or vertebroplasty, tumors, infections, or incomplete data were excluded from the study.
1. Measurement of Insertional Torque
In each case, pedicle screw insertion was performed using a conventional posterior approach and freehand technique. Screws were inserted before decompression of the laminae, foramina, and facet joints. The screw insertion point of lumbar spine was the junction of mid-transverse process line and lateral border of superior articular process. For the screw insertion point in the thoracic spine, we adopted the method described by Kim et al. [20].
The insertion process involved creating an entry point with a 4-mm burr, followed by the creation of a pilot hole using a gear shift. Subsequently, tapping was performed using a tool 1-mm thinner than the screw to expand the pilot hole. We utilized 2 types of pedicle screws: Xia (Stryker Spine, Allendale, NJ, USA) and EDEN Spinal Fixation System (JMT Co., Yangju, Korea). The 2 types of screws do not exhibit significant differences in material, thread space, or thread arrangement. The screw driver handle was manual ratchet-type. Screws with a diameter of 6.5 mm and length of 40–50 mm were used throughout the study. Insertional torque was measured using a calibrated torque wrench equipped with a specially designed connector for the spine screw system (Fig. 1). The maximal torque generated during insertion was measured when the screw shank was at a point that passed through the pedicle, which was approximately in the middle of the screw length. A total of 284 screws were analyzed. Intraoperative radiographs were obtained after inserting the screws to verify their locations and directions. Two board-certified neurosurgeons (HJL and ISK) performed all operations.
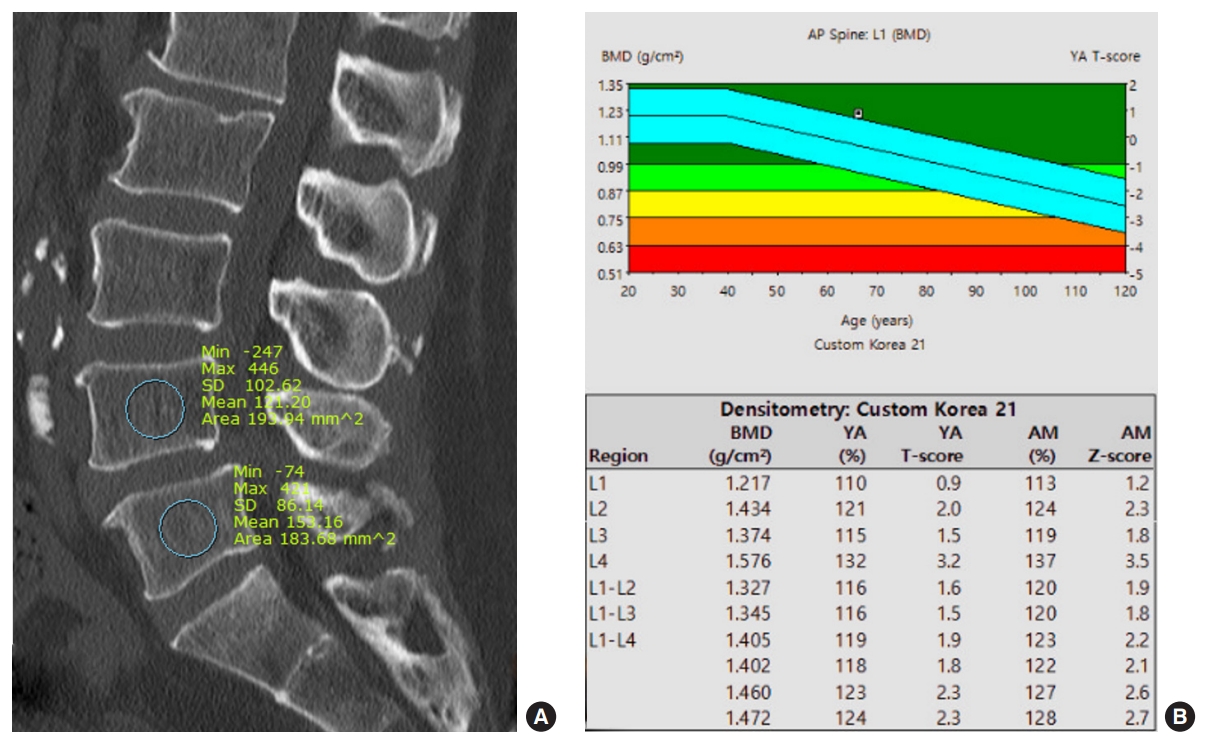
2. Measurement of Hounsfield Units
All radiological measurements were performed using a picture archiving and communication system (M-view 5.4; Marosis Technologies Inc., Seoul, Korea). CT scans were performed using a 256-slice scanner with a 2-mm axial image thickness (Siemens Medical Solutions, Erlangen, Germany), and sagittal reconstruction images were obtained using 1.25-mm-thick slices. In the present study, midsagittal reconstruction images of the vertebral bodies were selected to measure the HU. The HU values for each vertebral body, inserted per screw, were determined by measuring the trabecular portion of the vertebral body. HU measurements for each vertebra were obtained using a circletype region of interest (≥ 50 mm2), excluding the cortical bone margin (Fig. 2). The measurements were performed by 2 boardcertified neurosurgeons (HJL and ISK). And they cross-validated the results.
3. Correlation of Insertional Torque With BMD and HU
The insertional torque of each screw was analyzed using 2 parameters: T value (BMD) and HU of the vertebral body. As part of the subgroup analysis, the patients were categorized into the following groups based on the mean BMD of the lumbar vertebrae: normal (nonosteoporotic) (T value> -1.0), osteopenia (-2.5< T value< -1.0), and osteoporosis (T value< -2.5). Afterward, the insertional torque of each screw was analyzed in these 3 groups.
4. Statistical Analysis
All results were presented as means ± standard deviation. Statistical analyses were conducted using IBM SPSS Statistics ver. 25.0 (IBM Co., Armonk, NY, USA). Continuous variables were expressed as means ± standard deviation. Pearson correlation coefficient was used to assess the correlation between different groups. The threshold for determining significant differences was set at p < 0.05.
RESULTS
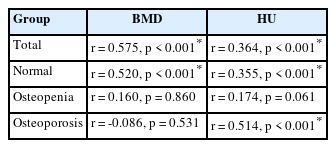
The mean torque generated during pedicle screw insertion was 105.55 ± 58.08 N∙cm, with 104.75 ± 56.69 N∙cm on the right side and 106.34 ± 59.63 N∙cm on the left. The correlation coefficient (r) between the left and right sides was 0.816 (p < 0.001), indicating a strong positive correlation between torque values on both sides. The mean T value was -1.14 ± 1.49 and mean HU value was 136.37 ± 57.59. Overall, there were positive correlations between torque and BMD (r = 0.575, p < 0.001) and between torque and HU (r = 0.364, p < 0.001) (Table 1). These findings showed that, in general, screw insertional torque had a stronger positive correlation with BMD than it did with HU values.
1. Subgroup Analysis: Comparison of the Correlations Among the Normal, Osteopenia, and Osteoporosis Groups
Patients and screws were categorized based on BMD as follows: normal (21 patients, 112 screws), osteoporosis (21 patients, 117 screws), and osteopenia (11 patients, 55 screws). The mean insertional torque for each grade of spinal osteoporosis was 137.86 ± 65.78 N∙cm, 88.76 ± 43.45 N∙cm, and 75.45 ± 32.09 N∙cm for the normal, osteopenia, and osteoporosis groups, respectively. The mean BMD for each grade of spinal osteoporosis was 0.29 ± 1.25 for the normal group, -1.69 ± 0.37 for osteopenia group, and -2.85 ± 0.46 for osteoporosis group. The mean HU for each grade of spinal osteoporosis were 152.79 ± 53.08 for the normal group, 142.51 ± 59.30 for osteopenia group, and 89.85 ± 34.52 for osteoporosis group. In patients with normal bone density, BMD (r = 0.520, p < 0.001) and HU (r = 0.355, p < 0.001) were positively correlated with insertional torque, with BMD displaying a stronger correlation. In the osteopenia group, all variables showed very low correlations with insertional torque, including BMD (r = 0.160, p = 0.860) and HU (r = 0.174, p = 0.061). Neither BMD nor HU showed a significant correlation with insertional torque.
In the osteoporosis group, BMD (r = -0.086, p = 0.531) showed no significant correlation with insertional torque. However, HU (r = 0.514, p < 0.001) demonstrated a reliable and significant positive correlation with insertional torque (Table 2).
DISCUSSION
Several studies have investigated the correlation between bone density as assessed by BMD and the fixation strength of pedicle screws. However, the findings of these studies have been inconsistent; and to date, no study has included the HU value. In the present study, we aimed to explore the relationship between insertion torque and radiographic values (BMD and HU) that reflect the representative bone density.
The pullout strength is typically influenced by 3 important factors. The first is the intrinsic properties of the surgical instrumental components such as screw length, screw diameter, type of alloy, and thread design. Second, a patient’s medical condition, including factors such as bone quality, bone density, and underlying medical diseases, is an important determinant of fixation strength. The last factor is the surgeon’s skill and surgical techniques, including medial convergence of the screw, fixation level, tapping procedure, bone dust filling into the pedicle, and use of bicortical fixation [21,22].
The insertional torque of the screw, primarily generated by the shearing force and friction at the bone-screw interface, represents the angular moment of the force needed to advance the screw into the bone. Several factors can affect the insertional torque of a pedicle screw, including variations in the insertion point, type and size of the instrument used screw track enlargement, and design of the screwdriver handle used for measurement [23]. To minimize potential measurement errors in the present study, the screw track was enlarged by 2 surgeons using the same instrument and screwdriver handle. This standardized approach ensured consistency and accuracy in the assessment of insertional torque.
Perren [24] discovered a correlation between the maximum axial compression force and insertional torque of cortical screws in bovine cancellous bone. Additionally, cadaveric studies have reported a significant correlation between the insertional torque of pedicle screws and BMD and pullout strength [25-27]. Moreover, Zdeblick et al. [13] stated that screws with insertional torque < 4-inch pounds resulted in early pullout failure based on their cyclic cephalocaudal toggling test in vitro. Furthermore, Daftari et al. [28] demonstrated a strong correlation between the insertional torque and pullout strength of pedicle screws in a study using synthetic bone material and calf vertebrae. They concluded that if the insertional torque was measured intraoperatively, an anticipated load failure for the screw could be predicted using a mathematical relationship; however, they did not propose a specific threshold [29].
However, torque-measuring devices are not routinely used during spine surgeries. Instead, the surgeon relies on subjective tactile sensations to judge the insertional torque, which may lead to inaccuracies [14]. This subjective perception-based determination of insertional torque is prone to variability and may not provide precise information.
The measurement of insertional torque is beneficial not only for evaluating pullout strength, but also for assessing bone density (quality) and ensuring rigid fixation in real time during surgery. By incorporating torque measurements, surgeons can obtain valuable and objective data to guide informed decisions and enhance overall surgical outcomes.
In the present study, we successfully implemented a suitable technical method for determining the objective strength of the screw insertional torque in general spine fusion surgery. We observed a positive correlation between patients’ BMD, HU, and insertional torque values. Although most of the insertional torque values for different fusion levels in the same patient remained similar, there were some cases with significant deviations (range, 80–200 N∙cm). The variability in insertional torque values of a patient proved to be valuable in guiding decisions regarding additional surgical techniques. For example, based on torque measurement, we determined the need for techniques such as autobone packing in the pedicle hole, omitting tapping, and employing bicortical first sacrum (S1) screw fixation or extension of the fusion. Moreover, the insertional torque data provided important insights for postoperative decisions, such as the medical management of osteoporosis, determination of the immobilization period, and selection of the appropriate brace. Furthermore, torque measurement offers a means to prevent screw malposition, particularly lateral breach, and enables the verification of bicortical purchases during surgery. Overall, objective strength assessment through torque measurement has proven to be a valuable tool for enhancing surgical decision-making, optimizing postoperative care, and ensuring good spinal fusion outcomes (Fig. 3).

Preoperative axial (A) and sagittal (B) magnetic resonance images of a patient with severe spinal stenosis at the L4–5 level. After undergoing lumbar fusion surgery, postoperative anterior-posterior (C) and lateral (D) simple spine x-ray images show the surgical outcome and placement of the screws. The red circle in image D highlights the left L5 screw, where the initial insertional torque measurement was 80 N·cm, which was significantly lower than other measurements. Intraoperative C-arm imaging revealed that the screw had a lateral breach. After proper reinsertion, the insertional torque was 200 N·cm, indicating a successful correction of the screw placement.
Quantitative CT (QCT) and DEXA are currently the representative methods for evaluating osteoporosis. DEXA is the most commonly used test method; however, its results may be less reliable than those of QCT owing to superimposition effects (bone spur, aortic calcification, and sclerotic changes) [30-35]. However, the QCT is not commonly used because of its high cost and high-dose radiation exposure. Consequently, a specific testing method is determined based on the preferences of each medical institution, considering their respective advantages and disadvantages [36].
The use of HU in routine preoperative CT reduces the superimposition effects and indirectly measures osteoporosis, thus complementing the information obtained from DEXA [37]. Some studies have demonstrated a close relationship between thoracolumbar CT and DEXA results [16,38]. Therefore, HU measurement from CT scans was selected as the method for assessing bone quality in this study.
In the present study, BMD and HU were positively correlated with insertional torque. However, as bone quality decreased, the correlation of BMD and HU with insertional torque rapidly declined, and only HU demonstrated a meaningful correlation with insertional torque in patients of osteoporosis. These findings are consistent with those of previous studies, which also reported a poor correlation between insertional torque and BMD in patients with osteoporosis [13,23]. This suggests that, as bone quality deteriorates, HU becomes a more reliable indicator of insertional torque.
The reasons for the poor correlation of insertional torque with BMD in patients with osteoporosis may be multifaceted. One potential reason for this could be the limitations of the torque-measuring instruments used in the present study. Below a certain bone quality threshold, the precision of the torque-measuring instrument may decrease, leading to less accurate measurements of screw fixation strength. Another reason was that the meanings and expressions of the numbers in the T score (standard deviation) and HU (unrefined) were different. In healthy patients, the absolute HU values tended to change significantly.
Additionally, BMD was measured throughout the vertebral body, including both the cortical and cancellous bone portions. However, the bone-screw interface at the trabecular bone inside the pedicle is the critical region affecting torque, and this specific area may not be adequately reflected in the overall BMD measurements.
Meanwhile, HU may have demonstrated a significant correlation with torque in osteoporosis owing to certain advantages it offers over BMD. HU measurements do not include the cortical bone portion and can reduce the superimposition effect, leading to a more precise reflection of the properties of the trabecular bone, which directly influence the torque. This finer resolution at the trabecular level may explain the stronger correlation observed between HU and torque in patients with osteoporosis.
Considering these factors, the use of HU measurements may prove advantageous for assessing bone quality and predicting screw fixation strength in patients with osteoporosis. However, further research and validation studies are necessary to confirm these findings and explain the intricate relationship between bone quality measurements and screw fixation outcomes.
This study had several limitations that should be considered. First, although the study had a relatively large sample size compared to other in vivo studies [23,39,40] the lack of a prospective assessment of the sample size might have implications for the statistical power and generalizability of the results. Future studies with prospectively determined sample sizes could strengthen the findings of the present study. Second, the individual pedicle size was not considered a variable in this study. Generally, pedicle size plays a role in determining insertional torque because smaller pedicles tend to yield higher torque values. While a constant screw diameter was used (6.5 mm) and insertion methods were unified to control other variables. Third, BMD was assessed using the average value (T score) of the lumbar vertebrae, while HU were measured in each individual vertebra where screw insertions took place. Because we aimed to exclude the possibility that individual factors such as bony islands, hemangiomas, aortic calcification, and others could function as variables. Fourth, the analysis did not include mid-and long-term clinical outcomes. Further studies examining the relationships among insertional torque, bone quality, and long-term clinical outcomes is warranted.
CONCLUSION
The present study is the first to investigate the correlation between HU and BMD and torque measurements in thoracolumbar fusion surgery. The measurement of insertional torque, which allows for the direct evaluation of rigid fixation during surgery, has great clinical significance. In particular, HU can be more advantageous than BMD for assessing bone quality and predicting screw fixation strength in patients with poor bone quality. Understanding these correlations can aid informed decision-making regarding perioperative management.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: JBL, HJL, ISK; Data curation: BHO, JYK, HJL; Writing - original draft: BHO; Writing - review & editing: JBL, JTH, JHS, KDT, HJL, ISK.