Sacropelvic Fixation for Adult Deformity Surgery Comparing Iliac Screw and Sacral 2 Alar-Iliac Screw Fixation: Systematic Review and Updated Meta-Analysis
Article information
Abstract
Objective
Two commonly used techniques for spinopelvic fixation in adult deformity surgery are iliac screw (IS) and sacral 2 alar-iliac screw (S2AI) fixations. In this article, we systematically meta-analyzed the complications of sacropelvic fixation for adult deformity surgery comparing IS and S2AI.
Methods
The PubMed, Embase, Web of Science, and Cochrane clinical trial databases were systematically searched until March 29, 2023. The proportion of postoperative complications, including implant failure, revision, screw prominence, and wound complications after sacropelvic fixation, were pooled with a random-effects model. Subgroup analyses for the method of sacropelvic fixation were conducted.
Results
Ten studies with a total of 1,931 patients (IS, 925 patients; S2AI, 1,006 patients) were included. The pooled proportion of implant failure was not statistically different between the IS and S2AI groups (21.9% and 18.9%, respectively) (p = 0.59). However, revision was higher in the IS group (21.0%) than that in the S2AI group (8.5%) (p = 0.02). Additionally, screw prominence was higher in the IS group (9.6%) than that in the S2AI group (0.0%) (p < 0.01), and wound complication was also higher in the IS group (31.7%) than that in the S2AI group (3.9%) (p < 0.01).
Conclusion
IS and S2AI fixations showed that both techniques had similar outcomes in terms of implant failure. However, S2AI was revealed to have better outcomes than IS in terms of revision, screw prominence, and wound complications.
INTRODUCTION
Treatment of spinal deformities affecting the lumbosacral junction has progressed to a significant dependence on pelvic fixation to establish a more stable base, leading to improved fusion outcomes and decreased instances of lumbosacral fixation failure [1]. Many methods have been documented throughout the years, but the iliac screw (IS) and sacral 2 alar-iliac screw (S2AI) fixations are the most frequently performed methods, with more biomechanical stability than other techniques [1-4].
IS is inserted at the posterior superior iliac spine (PSIS) independent of other points of fixation, targeting the superior acetabular notch or anterior superior iliac spine. However, the placement of IS requires more extensive soft-tissue dissection and complex connector systems during the operation and leads to instrumentation pain, screw prominence, and wound complications, postoperatively [5,6]. Therefore, the S2AI was introduced in 2007 to overcome the challenges associated with IS fixation. This approach utilizes a lower profile and more medialized screw head than IS and has been supported by several studies demonstrating lower complication rates [1,7-9]. Theoretically, the S2AI offers several potential advantages over the IS technique. Its insertion point is deeper, and offset use is typically unnecessary because the starting point of an S2AI screw aligns with that of the S1 pedicle screw at the S2 alar [10]. Several comparative studies have evaluated the outcomes of IS and S2AI techniques in spinal pelvic fixation. Nevertheless, the findings of these studies have been inconclusive. While some studies [11,12] have shown that the S2AI technique has lower rates of implant failure and revision surgery than those of IS fixation, other studies [13,14] have not found consistent results [15-17]. As pelvic fixation techniques have become more popular in recent years, several multicenter studies with large numbers of patients have been conducted [18,19].
The objective of the current study was to perform a meta-analysis comparing IS and S2AI fixation techniques in patients with adult deformities, with a focus on postoperative outcomes, considering recent multicenter studies with large numbers of patients.
MATERIALS AND METHODS
This research was conducted in accordance with the PRISMS (preferred reporting items for systematic reviews and meta-analyses) guidelines [20]. We performed a meta-analysis and systematic review of clinical studies on sacropelvic fixation for deformity surgeries comparing IS and S2AI fixations.
1. Search Strategy
We searched records in PubMed, Embase, Web of Science, and Cochrane clinical trial databases since their inception until March 29, 2023. The following search queries were included: IS and S2AI synonyms and related terms, including (iliac) AND (S2AI OR [sacral 2 alar iliac] OR [S2 alar iliac] OR [sacral two alar iliac]). In addition, we reviewed the references of all the chosen articles to identify any other relevant studies. Two reviewers (HKS and JHP) conducted the literature search and selection independently. In case of disagreements between the reviewers, consensus was achieved through a thorough discussion.
2. Study Selection
Patients, interventions, outcomes, and study design (PICOS) criteria were used to choose inclusion for the studies. PICOS criteria in this article were as follows: (1) “patients” with adult deformity surgery using iliac fixation, (2) IS or S2AI as the “intervention,” (3) no relevant “comparator,” (4) complications as the “outcome,” and (5) original articles for “study design.” The exclusion criteria included the following: (1) nonoriginal articles; (2) not in the field of interest; (3) no comparative study between IS and S2AI; (4) biomechanical, technical, or cadaveric studies; (5) overlap in study population; and (6) not written in English. When research populations overlapped, the study with the most comprehensive data was included. If the data were not sufficient to calculate the effect sizes accurately, contingency tables and/or individual data were requested from the corresponding author.
3. Extraction of Data
We collected demographic data and postoperative complications for both the IS and S2AI techniques. Demographic data of the included studies were extracted using a standardized form, including author, publication year, study period, country, study design, multicenter or not, the number of patients, age, sex, and follow-up period. Postoperative complications were analyzed as follows in each study: implant failure (pelvic screw breakage, pelvic screw loosening, pseudoarthrosis, and rod breakage), revision, screw prominence, and wound complications (wound infection and dehiscence).
4. Quality Assessment
The Risk of Bias In Nonrandomized Studies of Interventions (ROBINS-I) tool was utilized to evaluate the methodological quality of the included studies [21]. This tool evaluates 7 domains that can impact the quality and potential biases of the research, including confounder, subject selection, classification of interventions, deviations in interventions, missing data, biased measurements, and biased reporting. Each domain is rated on a scale of low, moderate, serious, or critical potential for bias. The data extraction and quality evaluation were conducted by 2 reviewers independently, and any differences were resolved through discussion.
5. Statistical Analysis
To examine the association of combined results, we calculated the percentage along with a 95% confidence interval (CI) for the included studies. The proportions were pooled using meta-analysis utilizing the random-effects model (DerSimonian-Laird method) with logit transformation for computing weights [22]. The Cochran Q and Higgins I2 tests were performed to assess heterogeneity between the studies. To assess the presence of publication bias, funnel plots and Egger tests were used [23]. All tests were 2-sided, and statistical significance was considered when the p-value was equal to or less than 0.05. The statistical analysis was carried out using R ver. 4.0.4 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
1. Literature Search
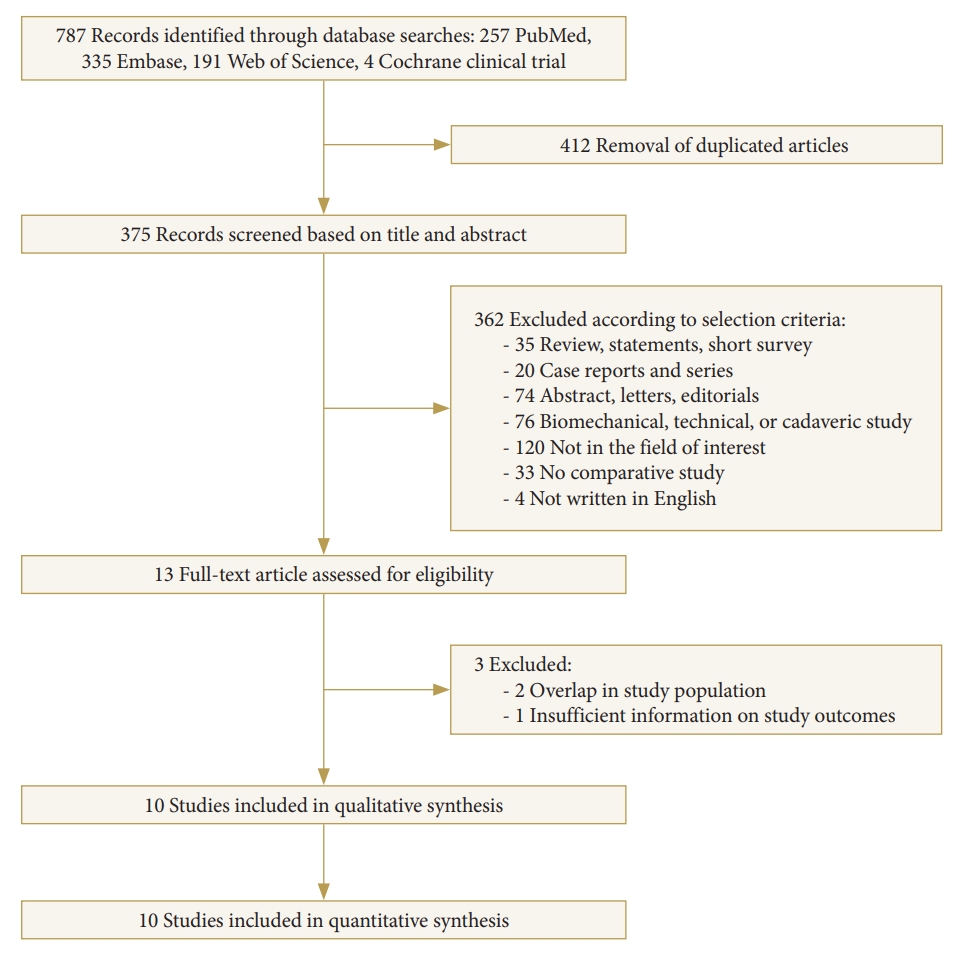
The subject headings were used to conduct a preliminary literature search, resulting in 257 articles from PubMed, 335 studies from Embase, 191 studies from Web of Science, and 4 studies from the Cochrane clinical trial databases. After removing 412 duplicates from the 787 studies, 375 titles and abstracts were evaluated. Among them, 362 studies were deemed ineligible according to the exclusion criteria. Of the remaining 13 studies, 3 were excluded due to either overlapping study populations (n = 2) or insufficient information on study outcomes (n = 1). Finally, a total of 10 studies were included in this meta-analysis [11,13,14,18,19,24-28]. The detailed selection process is illustrated in Fig. 1.
2. Study Characteristics
The baseline characteristics of the included studies are summarized in Table 1. Overall, the included 10 studies comprised of 1,931 patients (925 IS and 1,006 S2AI). Five studies were published before 2020, and the remaining 5 studies were published after 2020. Most studies had a retrospective design, except 1 study, which had a prospective design. Three studies were multicenter studies, and 7 studies were single center studies. The mean follow-up period was 2–3 years after surgery.
3. Quality Assessment
The overall risk of bias for quality assessment using the 7 domains of the ROBINS-I tool is shown in Supplementary Table 1 and Supplementary Fig. 1. Overall, a shortage of information in specific cause of implant failure caused serious risk of bias in the domain of biased reporting in 4 of the 10 studies. As 3 studies were multicenter studies, the baseline confounding was evaluated as serious, and classification of interventions and deviations in interventions were evaluated as moderate.
4. Implant Failure
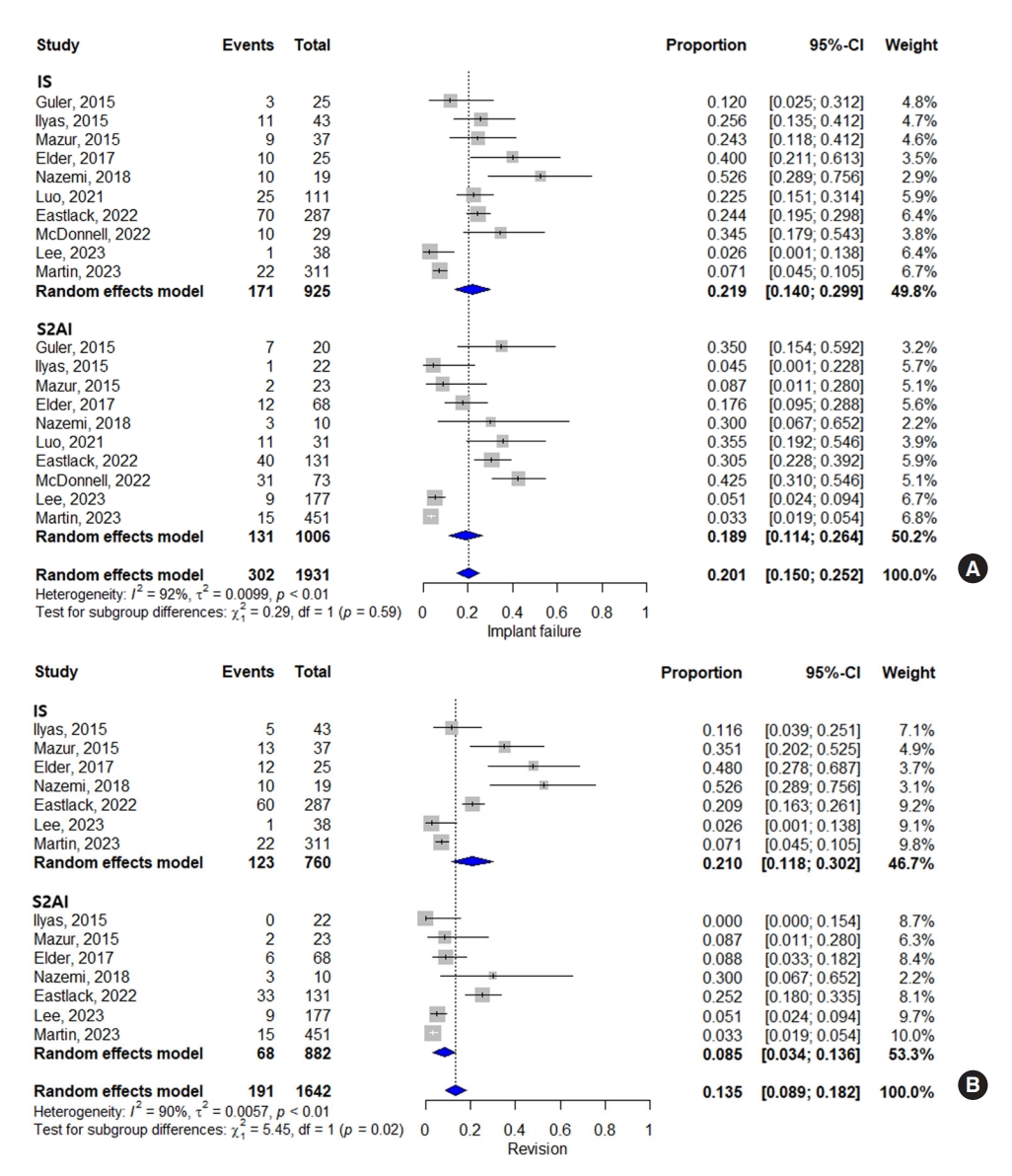
All 10 studies demonstrated implant failure, such as pelvic screw breakage, pelvic screw loosening, pseudoarthrosis, or rod breakage. We analyzed the total rates of implant failure rather than focusing on the individual cause of implant failure because the causes frequently overlap, which results from the spectral interaction of each cause [27]. The total rates of implant failure after pelvic fixation are illustrated in Fig. 2A. For both IS and S2AI methods, the pooled proportion of implant failure was 20.1% (95% CI, 15.0%–25.2%). The Higgins I2 statistics revealed significant heterogeneity (I2= 92%). The subgroup analysis showed that the proportion of implant failure was not statistically different between the IS and S2AI groups (p = 0.59) (proportion, 21.9%; 95% CI, 14.0%–29.9% and proportion, 18.9%; 95% CI, 11.4%–26.4%, respectively). The funnel plot and Egger test showed no publication bias (Supplementary Fig. 2; Intercept= -0.86, p = 0.20).
5. Revision
Seven studies assessed the proportion of revision in both IS and S2AI techniques. For all 7 studies, the pooled proportion of revision in the IS group was 13.5% (95% CI, 8.9%–18.2%). The subgroup analysis showed that the proportion of revision was higher in the IS group than that in the S2AI group (proportion, 21.0%; 95% CI, 11.8%–30.2% and proportion, 8.5%; 95% CI, 3.4%–13.6%, respectively), with statistical significance (p = 0.02) (Fig. 2B). The funnel plot and Egger test showed no publication bias (Supplementary Fig. 3; Intercept= -1.24, p = 0.26).
6. Screw Prominence
Three articles assessed the screw prominence in both IS and S2AI techniques. Meta-analytic pooling of all 3 studies regarding the screw prominence indicated that the pooled proportion was 2.7% (95% CI, 0%–6.5%). The subgroup analysis showed that the pooled estimate for screw prominence was higher in the IS group than that in the S2AI group (proportion, 9.6%; 95% CI, 3.2%–16.0% and proportion, 0%; 95% CI, 0%–1.9%, respectively), with statistical significance (p < 0.01) (Fig. 3A). The funnel plot and Egger test showed no publication bias (Supplementary Fig. 4; Intercept= -0.86, p = 0.06).
7. Wound Complications
Five studies assessed the proportion of wound complications in both IS and S2AI techniques. Wound complications included both wound infection and dehiscence. For all 5 studies, the pooled proportion of wound complications in both the IS and S2AI groups was 18.1% (95% CI, 8.9%–27.4%). The subgroup analysis demonstrated that the proportion of wound complications was higher in the IS group than that in the S2AI group (proportion, 31.7%; 95% CI, 11.5%–51.9% and proportion, 3.9%; 95% CI, 0%–7.9%, respectively), with statistical significance (p < 0.01) (Fig. 3B). The funnel plot and Egger test showed no publication bias (Supplementary Fig. 5; Intercept=0.45, p = 0.05).
Detailed characteristics of complications in the included studies are demonstrated in Table 2.
DISCUSSION
There are multiple ways to achieve spinopelvic fixation, but 2 of the most commonly used techniques are IS and S2AI fixations. Extended fusions reaching the sacrum, cases involving revision of previous fusions, deformities, and other similar cases can all receive extra advantages in terms of biomechanical strength by using instrumentation that extends down to the pelvic ring [1]. Traditionally, IS fixation has demonstrated greater biomechanical stability than previously introduced spinopelvic fixation techniques [3]. However, screw prominence and wound complications are considerable problems due to superficially located entry point at PSIS. Consequently, the strategies and approaches for IS placement have undergone development to enhance efficiency and alleviate the previously perceived limitations of this technique. The modified technique of IS fixation, which removes a section of the PSIS where the screw head was positioned and driving the screw head deeper, was introduced with better clinical outcomes [29]. In addition, to address this issue, alternative techniques, such as the S2AI, have been introduced. While the IS is typically connected to a midline rod-screw structure via rod connectors [14], the S2AI is simpler to connect to proximal instrumentation and has a deeper and more medial entry point, reducing tissue dissection with a lower-profile screw head [6]. Additionally, recent studies suggest that S2AI fixation minimizes the risk of revision surgery and wound infection [14,24].
In this meta-analysis, we pooled data from 10 cohort studies comparing the IS and S2AI fixation techniques in adult patients [11,13,14,18,19,24-28]. Analysis of the outcomes based on the implant failure showed that the pooled proportion of patients with implant failure was not statistically different between the 2 techniques: 21.9% with IS and 18.9% with S2AI, respectively (p = 0.59). However, analysis based on revision, screw prominence, and wound complications showed that the pooled proportion of patients with each complication was higher in the IS group than that in the S2AI group (revision, IS: 21.0% vs. S2AI: 8.5%, p = 0.02; screw prominence, IS: 9.6% vs. S2AI: 0.0%, p < 0.01; wound complications, IS: 31.7% vs. S2AI: 3.9%, p < 0.01). These results suggest that, although the mechanical stability of the 2 techniques is not different, the risk of invasive complications is higher in IS than those in S2AI.
The comparison of implant failure between IS and S2AI has been the subject of several studies. Differences in positioning and biomechanics between IS and S2AI techniques may result in varying rates and types of failures. However, biomechanical studies have shown that both constructs have similar stability in terms of stiffness and load to failure [30-32]. In a human cadaveric study by O’Brien et al. [9], the biomechanical strength of IS and S2AI fixations was compared. They found that S2AI was as stable as IS in all loading modes and shorter S2AI was equivalent in strength to longer IS in achieving spinal fixation. As IS is predominantly placed in a cancellous bone bed, while S2AI encounters the cortical bone of the sacroiliac joint articulation, S2AI provides additional fixation strength despite the shorter length. Burns et al. [31] conducted a biomechanical study using cadavers to investigate the torsional stiffness of IS and S2AI during extension, forward flexion, and lateral flexion. They revealed that there were no significant differences in torsional stiffness between the 2 types of screws. Some of the mechanical advantages of S2AI over IS include obviation of the offset connector, which eliminates a potential point of failure, greater cortical purchase, and anterior location to the lumbosacral pivot point [1,14,32]. Furthermore, results from the study by Shin et al. [33] show that the maximum equivalent stress on the screw and bone in S2AI fixation was lower than that in IS fixation, highlighting its efficacy as a preferred method of sacropelvic fixation. However, the medial starting point of the S2AI may result in an acute angle between the screw head and shaft, which can create strain and potentially lead to failure, particularly in cases of extreme headshaft angulation [13,26].
Clinical studies have reported conflicting results regarding implant failure. Some studies have found that S2AI has a lower risk of implant failure than that of IS, whereas others have found the opposite. A recent multicenter study found a slightly higher rate of screw failure with IS than that with S2AI in the univariate analysis, with no significant difference in the multivariate analysis [19]. Another recent multicenter study found higher loosening rate of pelvic screw in the S2AI group than that in the IS group and higher rod fracture rate in the IS group than that in the S2AI group [18]. In a study by Cho et al. [34], involving 45 cases, the S2AI had a higher failure rate than the IS (35% vs. 12%). Ilyas et al. [11] found an 18.6% rate of traditional IS loosening, while none was evident in their S2AI cohort. In the meta-analysis by Guler et al. [13], loosening of pelvic fixation was more prevalent after the use of IS, with an IS loosening rate of 17.6% compared with 5.1% with S2AI. Elder et al. and Ishida et al. both found similar rates of loosening when comparing the types of screws [24,35,36]. Therefore, given the conflicting evidence in the literature and similar results of the current meta-analysis, the evidence regarding implant failure is mixed, and further studies are needed to determine which construct is superior.
In the pooled analysis for the revision surgery in this meta-analysis, the rates of revision surgery were significantly higher in the IS group (21.0%) than that in the S2AI group (8.5%) (p = 0.02). This is concordant with most previous studies [11,14,24]. Mazur et al. [14] reported a revision rate of 35% for IS compared to 8.6% for S2AI. Elder et al. [24] reported a revision rate of 48% in the IS group compared to 8.8% in the S2AI group. The higher rates of revision surgery were because of prominent IS head, causing wound infection or dehiscence, or implant failures, such as rod fracture, or distal device breakage [24,36]. Recently, Martin et al. [19] discovered that out of the 37 revision surgeries carried out due to acute failure of iliac fixation, 6 (16%) required an additional revision surgery after experiencing a second failure. This result highlights the challenges involved in achieving a stable status following iliac fixation. In addition, Ishida et al. [12] discovered that the duration between the surgery and revision surgery after iliac fixation was considerably shorter in the case of IS than that of S2AI. As this finding demonstrated relatively inferior clinical outcomes of IS compared to S2AI, these findings suggest that the use of S2AI screw instrumentation may provide potential benefits for patients who are prone to experiencing difficulties maintaining stability or wound complications, particularly the elderly [36].
Patients who undergo instrumented fusions for adult spinal deformities often experience pain due to implant prominence, which is a common reason for reoperation [37,38]. This particularly occurs in patients who have the IS, which requires offset connectors for instrumentation [6]. According to the study conducted by Tsuchiya et al. [6], in IS fixation, approximately one-third of the patients had to undergo removal of IS due to painful prominence. In addition, O’Shaughnessy et al. [39] studied that 78.3% of the patients who had elective removal of IS due to hip and buttock pain reported a significant improvement of pain after the screw removal. This form of pain typically occurs several months to years after the surgery [38]. In contrast, the starting point for the S2AI is located approximately 15 mm deeper than that for the IS, and due to its more medial position on the sacrum, a greater amount of soft tissue covers the S2AI with much less prominence complications [10].
The present meta-analysis revealed that individuals who underwent S2AI fixation exhibited a statistically significant reduction in the occurrence of wound complications in comparison to those who received IS fixation (IS: 31.7% and S2AI: 3.9%, p < 0.01). This may be related to decreased soft-tissue dissection in the S2AI approach since there is no dissection over the subcutaneous tissue over the iliac crest or sacral paraspinous muscles, whereas IS is accompanied by more dissection in this area, which leads to wound healing problems [10,40]. Additionally, higher incidence of wound complications in the IS group may be due to the proximity of devices from the skin, which is related with screw prominence and slightly longer operative times [24].
There were some limitations to this study. First, there was heterogeneity among the included studies. One such example was the study conducted by Mazur et al. [14], where they employed image-guidance stereotaxy for placing S2AI, possibly contributing to higher precision. However, fluoroscopic guidance was used for placing IS, which could have impacted the results differently. Second, the IS technique evolved during the study period. Due to unsatisfactory clinical outcomes related to screw prominence in early studies, a modified technique for IS placement was introduced. Kasten et al. [29] described a method involving the removal of a portion of the PSIS and the countersinking of the IS head into the iliac crest, which resulted in a reduction in complication rates. In addition, a new modification for IS placement, known as the subcrestal IS technique, has been recently introduced [41]. However, the potential differential effects of these modifications on clinical outcomes were not accounted for in this meta-analysis. Third, despite the probability of S2AI having inferior clinical outcomes in certain aspects, statistical analysis was difficult due to the rarity of the investigations. For example, both SI joint pain [26] and S1 screw loosening [18] are reported to be more prevalent in S2AI. However, these complications are each described in only one article among the 10 included articles. Fourth, the present study is concerning on the clinical outcomes rather than radiological outcomes. As the previous results of radiological outcomes have been inconsistent, further research on this topic is necessary [17,26]. Fifth, the definition of implant failure was different between the studies. Some studies defined failure as any revision to the pelvic screws [19,28]. However, other studies defined failure radiographically regardless of revision or not [18,27]. Besides, as some studies delineated each screw-related complication without utilizing the term “failure,” we aggregated each complication to conduct an analysis of implant failure [11,25,26,42]. Therefore, it is required to take into consideration these disparities when comparing rates of implant failure. Lastly, as most studies had a mean follow-up period of less than 3 years, the long-term effects of different fixation methods remain uncertain. Therefore, more research is required to overcome these limitations, especially studies with large sample sizes with longer follow-up periods that take into account updated iliac fixation techniques.
CONCLUSION
In this meta-analysis, we examined 10 studies that compared the outcomes of IS and S2AI fixations for spinopelvic fusion in adult deformity surgeries. The results showed that both techniques had similar outcomes in terms of implant failure. However, S2AI was found to be better than IS in terms of revision, screw prominence, and wound complications. Based on these findings, S2AI appears to be a better option for adult deformity surgeries than IS. However, it is also important to note that this study did not consider modified techniques of the IS. Thus, future randomized trials, which controls each surgical method, would be helpful in providing more insights on this subject.
Supplementary Material
Supplementary Materials: Supplementary Table 1 and Figs. 1-5 can be found via https://doi.org/10.14245/ns.2346654.327.
Table of risk of bias using the Cochrane ROBINS-I Tool
Graph of risk of bias assessment using the ROBINS-I (Risk Of Bias In Nonrandomized Studies of Interventions) tool.
Funnel plot for the proportion of implant failure.
Funnel plot for the proportion of revision.
Funnel plot for the proportion of screw prominence.
Funnel plot for the proportion of wound complications.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: HKS, JHP; Data curation: SRJ, SWR, DJJ, SJH, YJC; Formal analysis: HKS, JHP; Methodology: SRJ, SWR, DJJ, SJH, YJC; Project administration: YJC; Writing - original draft: HKS; Writing - review & editing: JHP.