Does Sacral Slanting Affect Postoperative Shoulder Balance in Patients With Lenke Type 2A Adolescent Idiopathic Scoliosis?
Article information
Abstract
Objective
Even minor sacral slanting can influence T1 tilt and shoulder balance. Yet, the relationship between sacral slanting and postoperative shoulder imbalance (PSI) has not been previously explored. To determine risk factors for PSI in Lenke 2A adolescent idiopathic scoliosis (AIS) patients, with an emphasis on sacral slanting.
Methods
The study encompassed 96 consecutive patients who had undergone posterior correction and fusion surgery for Lenke type 2A AIS. Patients were grouped into PSI(+) and PSI(-) based on postoperative outcomes. Additionally, they were classified into left-sided slanting, no slanting, and right-sided slanting groups according to the degree of sacral slanting. Various radiological measures were compared.
Results
Patients in the PSI(+) group exhibited a smaller preoperative proximal thoracic curve and a higher main thoracic curve correction rate than those in the PSI(-) group. The presence or absence of sacral slanting did not exhibit a significant variation in PSI occurrence. However, the right-sided sacral slanting group showed a larger delta radiologic shoulder height compared to the other 2 groups (7.1 mm vs. 1.5 & 3.3 mm).
Conclusion
Sacral slanting was not directly linked to the development of PSI. Despite the common postoperative elevation of the left shoulder, the shoulder height differences decreased over the follow-up period. Especially in cases with a right-sided tilted sacrum, the PSI demonstrated progressive improvement, with an associated increase in the rightward distal wedging angle, leading to distal adding-on.
INTRODUCTION
Correction surgery for adolescent idiopathic scoliosis (AIS) often leads to shoulder imbalance, a major concern for patients with a double thoracic curve. It has been historically crucial to recognize the proximal thoracic curve (PTC) since neglecting to fuse the PTC can cause coronal decompensation or postoperative shoulder imbalance (PSI) [1-3]. Although previous studies tried to identify the precise indications for PTC fusion, as well as risk factors associated with PSI after surgery, no definite conclusions have been drawn [4-6].
Sacral slanting in patients with AIS is a unique but common finding [7]. The degree of sacral slanting is defined as the angle between the horizontal line and the upper end plate of the sacrum. Because the sacrum is the foundation of the whole spine and the length of lever arm from the sacrum to T1 is long, even a small amount of sacral slanting can affect T1 tilt and cause shoulder imbalance [8]. The relationship between sacral slanting and PSI in patients with Lenke type 2 AIS has yet to be thoroughly researched.
Lenke type 2 scoliosis is a major thoracic curve with a minor structural PTC and a minor nonstructural thoracolumbar/lumbar curve [2]. In a prior study of ours, where we investigated factors influencing PSI in Lenke type 2 AIS patients who underwent surgery, only the Risser grade was identified as a preoperative factor affecting PSI development [9]. This may be due to the heterogeneity of the study population because Lenke type 2 includes various subtypes of lumbar curve, and the magnitude of a lumbar curve may affect shoulder balance in different ways. Therefore, the focus of this study was the effect of sacral slanting among factors on PSI in patients with Lenke type 2 AIS who had lumbar modifier A.
MATERIALS AND METHODS
1. Study Design and Participants
This study enrolled 96 patients who underwent deformity correction and a posterior fusion procedure for Lenke type 2A AIS. All patients were followed up for at least 2 years. Patients with a structural lumbar curve or a specific cause of scoliosis, including neuromuscular or congenital disease, and patients with missing data or those who were lost to follow-up were excluded. Deformity correction in all patients was performed using a pedicle screw-only construct, which was placed by a single surgeon (CSL) at a single institute. Pedicle screws were placed into as many segments as possible, and correction was performed using rod derotation, translation, and compression-distraction.
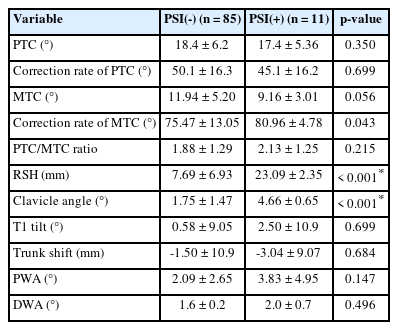
2. Data Collection and Radiographic Analysis
Demographic and radiological data were sourced from patients’ clinical records and the Picture Archiving and Communication System [10]. Radiological parameters were evaluated from whole spine standing anteroposterior radiographs taken preoperatively and postoperatively at 1 month, 6 months, and 1 year, and at final follow-up. Measurements included the Cobb angles of both the proximal and main thoracic curves, radiologic shoulder height (RSH), clavicle angle, T1 tilt, trunk shift, proximal and distal disc wedging angles (PWA and DWA), and the sacral slanting angle. The RSH was defined as the difference in the height between the acromion tips on both sides, whereas the clavicle angle was defined as the angle between a horizontal line and a tangential line connecting the 2 highest points of each clavicle (Fig. 1). The slanting angle between the upper endplate of the sacrum and the horizontal line was also measured. If the angle was >3°, patients were considered to have sacral slanting [7,11]. Parameters like RSH, clavicle angle, sacral slanting angle, and disc wedging angle were deemed positive if the right side was elevated. All assessments were performed by 3 orthopedic surgeons who specialized in spinal surgery. The same surgeons repeated all radiological parameter measurements 2 weeks later, and the mean of all measurements was used for the final analysis to eliminate measurement errors.
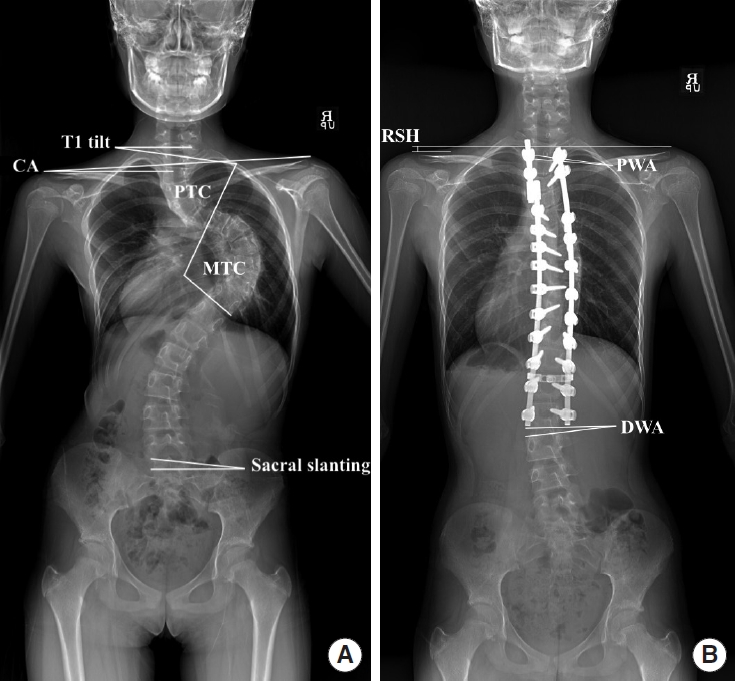
Illustration of key radiographic measurements. Panel A displays the T1 tilt, clavicle angle (CA), proximal thoracic curve (PTC) angle, main thoracic curve (MTC) angle, and sacral slanting angle. Panel B highlights the radiological shoulder height (RSH), proximal wedge angle (PWA), and distal wedge angle (DWA).
This study was approved by the Ethics Committee of Asan Medical Center (IRB number: 2021-1127), which waived the requirement for informed consent owing to the retrospective nature of the study.
The PSI was deemed positive when the absolute value of RSH was > 20 mm, and patients were stratified according to the presence PSI(+) or absence PSI(-) of PSI at the final follow-up. Radiographic parameters were compared, and changes (Δ) in RSH and DWA in both groups were tracked during the postoperative follow-up period. In addition, patients were divided into 3 groups based on slanting angle and direction: left-sided slanting (Lt.>3°), no slanting (0°–3°), and right-sided slanting (Rt.> 3°). Radiographic parameters were compared between the sacral slanting(+) and sacral slanting(-) groups, and ΔRSH and ΔDWA were tracked during the postoperative follow-up period in each slanting group.
3. Statistical Analysis
In our study, continuous variables, specifically radiological and demographical parameters between the PSI(-) and PSI(+) groups, were analyzed using the Mann-Whitney test. For categorical variables, Fisher exact test was utilized. This was specifically applied to assess the incidence and distribution of PSI among the different patient groups, categorized according to their sacral slanting orientation (left-sided, no slanting, and right-sided). Fisher exact test was selected due to its appropriateness for smaller sample sizes in each subgroup, providing a more precise evaluation of categorical data. The Kruskal-Wallis test was used to compare changes in RSH and DWA between the different slanting groups. IBM SPSS Statistics ver. 21.0 (IBM Co., Armonk, NY, USA) was used for all statistical analyses. A p-value of < 0.05 was considered statistically significant.
RESULTS
1. Demographic Data and Characteristics of Curves
The study population comprised 26 males and 70 females, with a mean age at the time of surgery of 15 years and 6 months. The mean height of the patients was 160.9 ± 0.8 cm, and the mean weight was 50.1 ± 0.9 kg. The mean follow-up period was 32.6 ± 1.2 months. The specific Lenke types were 2AN (54 patients), 2A- (41 patients), and 2A+ (1 patient). Of the 96 patients, 11 had a > 20-mm RSH difference; these were classified as the PSI(+) group. A difference of > 15 mm was observed in 25 patients. Of the participants, 57 (59.3%) had sacral slanting exceeding 3° (39 leaning left and 18 right), while 32 (38.8%) showed slanting of 5° or more (21 leaning left and 11 right).
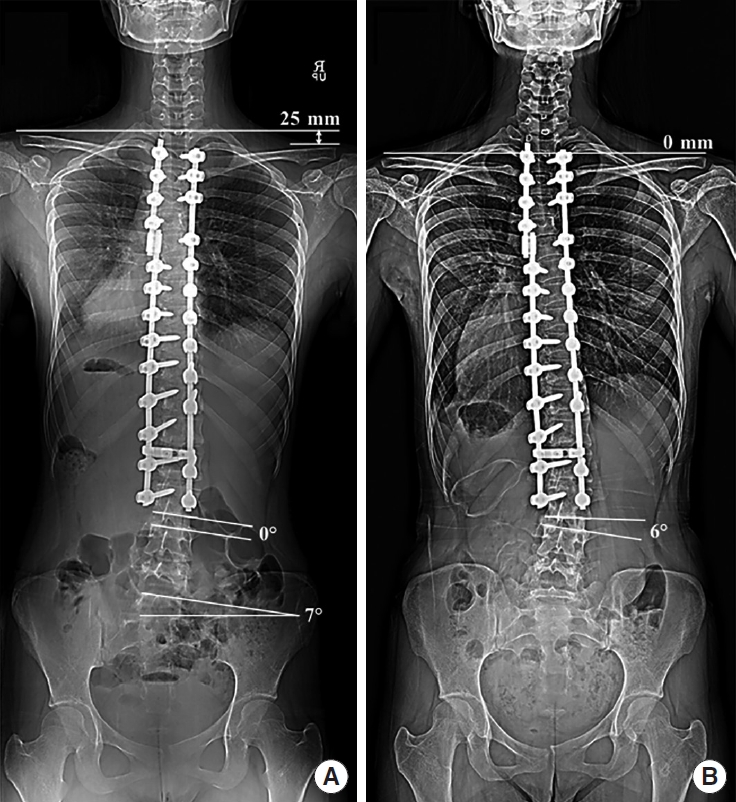
2. Comparison of the PSI and Non-PSI Groups
An analysis of the demographic data and preoperative radiographic parameters between the PSI(+) and PSI(-) groups is detailed in Table 1. Out of the 96 participants in the study, 85 were categorized under the PSI(-) group and 11 in the PSI(+). When comparing these 2 groups, the preoperative PTC in the PSI(+) group was significantly smaller (p = 0.019) than in the PSI(-) group. Both groups displayed similar age, height, weight, and other metrics, with no substantial variations. Table 2 illustrates the radiographic parameter comparisons at the final follow-up. While most values between the groups showed minimal differences, the PSI(+) group had a statistically significant higher MTC correction rate (p = 0.043). Notably, the PSI(+) group exhibited pronounced differences in RSH and clavicle angle.
Comparison of demographic data and preoperative radiographic parameters between the PSI(+) and PSI(-) groups
Preoperative assessments typically revealed an elevated right shoulder. However, postoperatively, in most cases, the right shoulder appeared lower than its left counterpart. Tracking the RSH evolution, the PSI(-) group demonstrated a consistent reduction, averaging 7.7 mm by the final follow-up. In contrast, the PSI(+) group showed a notable RSH of 23.3 mm one month postsurgery, which decreased over the year but surged again at the final evaluation. Table 3 underscores these shifts: one month after surgery, the PSI(+) group’s RSH was notably higher and this significant difference between the groups persisted until the final follow-up. By the end, the PSI(+) group’s RSH remained considerably higher, marking a difference especially when compared to the gradual decrease observed in the PSI(-) group.
3. Comparison of the Sacral Slanting Subgroups
Upon evaluating sacral slanting, 3 distinct subgroups were identified based on slanting angles: Lt.> 3°, 0°–3°, and Rt.> 3°. The incidence of PSI in these groups was 12.8%, 15.6%, and 5.5%, respectively. The analysis showed no statistically significant differences in PSI occurrence among these groups, as indicated by a p-value of 0.648 (Table 4). Further examination of the radiographic parameters, both preoperative and postoperative, revealed consistent patterns across all slanting categories, as seen in Table 5, where parameters such as PTC, MTC, and RSH remained similar across groups. The DWA for the slanting (Rt. > 3°) group was noticeably higher both postoperatively and at the final follow-up compared to the other groups. Moreover, the delta DWA in the right-sided slanting group exhibited a larger increase, indicating a progressive expansion of the DWA to the right in this group.
When comparing the 3 groups delineated by sacral slanting—Lt. ≥ 3°, 0°–3°, and Rt. ≥ 3°—it became evident that the right-sided slanting group experienced the most pronounced change in RSH (ΔRSH) during the follow-up period. At the final assessment, the RSH measurements across these groups were closely matched at 10.7 mm, 9.6 mm, and 8.7 mm, respectively. Notably, all groups showed a depressed right shoulder 1-month postsurgery. This trend reversed over time, indicating an improvement in balance. The data from Table 6 further accentuates that the most significant reduction in RSH was particularly evident in the right-sided sacral slanting group.
DISCUSSION
Sacral slanting is a unique but not rare phenomenon occurring in patients with AIS, but few studies have investigated it. Our previous study showed that 59.3% of patients with Lenke type 1A scoliosis had more than 3° of sacral slanting [7]. Sacral slanting affects distal adding-on in Lenke type 1A AIS, and in the L4-R type, right-sided sacral slanting tends to lower the last touching vertebra; thus the fusion level might be shorter [8]. Sacral slanting is also a critical consideration when selecting the distal fusion level when planning the correction of structural lumbar curves. Given its evident impact on coronal spinal deformities, we postulated a strong correlation between sacral slanting and shoulder balance post-AIS surgical correction. Contrary to our expectations, our results indicate that sacral slanting does not exert a direct influence on shoulder balance in Lenke type 2 AIS.
Past research has highlighted numerous factors related to PSI [12]. Significant among these are the clavicle angle and PTC, both shown to be pivotal in predicting postoperative shoulder balance [9,13]. In addition, a difference in the preoperative clavicle chest cage angle has been reported among patients with PSI [5]. Furthermore, recent findings suggest that the correction ratios of PTC and MTC are emerging as crucial predictors of post-surgical PSI [14,15]. We initially hypothesized that sacral slanting, given its significant impact on the body’s coronal orientation, would influence PSI. While our hypothesis was partially validated, particularly in the right-sided sacral slanting group with a notably larger delta RSH showing a pronounced elevation of the right shoulder over time, it did not directly correlate with the final lateral shoulder balance, as demonstrated in Table 6. However, the ultimate determinants of PSI(+), as seen in Tables 1 and 2, were a smaller preoperative PTC and a significant MTC correction rate.
On a theoretical basis, one might anticipate the shoulders of sacral slanting patients to lean towards the slanting direction. Yet, our findings revealed no discernible differences in RSH between the preoperative and postoperative slanting groups. Although sacral slanting might influence spinal curvature and T1 tilt, it appears not to directly affect the clavicle balance. The shoulder’s anatomical complexity, involving the clavicle, scapula, humerus, and associated musculoskeletal components, suggests that multiple factors might counteract the postural changes induced by sacral slanting [16]. In light of this, while sacral slanting does impact body orientation, its influence on the ultimate lateral shoulder balance seems indirect.
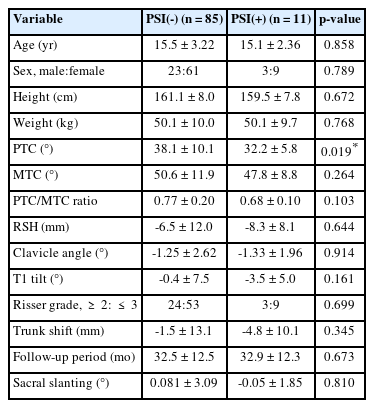
In the current study, there was no difference in the RSH before surgery between the PSI(+) and PSI(-) groups; however, PSI developed in some patients. Although the postoperative RSH tended to decrease with time in all groups, there might be a high possibility that patients with a large RSH immediately after surgery will experience persistent PSI. Notably, the decreasing tendency of RSH was greatest in the right-sided slanting group. Cao et al. [13] reported a positive correlation between PSI and distal adding-on in patients with Lenke type 2 scoliosis. Given the notably larger delta RSH in the right-sided sacral slanting group compared to the others, it is plausible that distal adding-on acted as a compensatory mechanism to rectify shoulder height after surgery (Table 6). This compensation might have mitigated the influence on the final PSI (Fig. 2).
Radiographs of a patient with Lenke 2A scoliosis. (A) The patient exhibited a right-sided sacral slanting of 7°. After undergoing surgical correction and fusion targeting the proximal and main thoracic curves, her right shoulder was notably depressed after surgery of 25 mm, with a nearly neutral distal wedging angle (DWA). (B) At 4-year follow-up, while the shoulder imbalance significantly decreased, the DWA increased to 6°, resulting on distal adding-on.
The orientation of the DWA in patients with sacral slanting is pivotal in deciphering compensatory mechanisms. When adjusting for an elevated left shoulder, an increase in the right DWA and a decrease in the left DWA are anticipated. In the cohort with right-sided sacral slanting, 17 patients demonstrated a rightward shift in DWA, while only one leaned leftward. Both the delta in DWA (from 1-month postoperation to the final follow-up) and the DWA observed at the final check were more pronounced in individuals with right-sided sacral slanting. This suggests that modifications in DWA beneath the lowest instrumented vertebra might counterbalance the effects of sacral slanting, aiding in the reduction of shoulder imbalance.
Shoulder balance is an important factor that affects patient satisfaction after surgery. In this study, however, shoulder imbalance was analyzed based on radiographic parameters only, and the apparent shoulder height difference was not analyzed. Further studies need to include actual gross shoulder height difference, as well as patient functional outcome scores evaluating subjective shoulder balance. While the values of sacral slanting and DWA are relatively modest, they do pose concerns regarding potential measurement inaccuracies. In addition, these parameters may be influenced by patient factors such as leg length discrepancy or pelvic rotation. Nonetheless, sacral slanting definitely exists in a substantial number of patients with scoliosis, and physicians treating coronal deformities must consider it when determining fusion levels and when evaluating patients during the postoperative follow-up period.
CONCLUSION
While sacral slanting doesn’t have a direct correlation with the development of PSI, its influence on postoperative shoulder rebalancing is evident, especially in cases of right-sided slanting. In particular, when the sacrum is slanted to the right, there appears to be an adaptive change in the DWA over time to accommodate shoulder height discrepancies, indicative of a distal adding-on process.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: CJH, HRL; Formal analysis: CJH; Visualization: SKL, SYS, JHC, DHL, CSL; Writing - original draft: CJH; Writing - review & editing: HRL.