Comparing Outcomes of Banana-Shaped and Straight Cages in Transforaminal Lumbar Interbody Fusion for Lumbar Degenerative Diseases: A Systematic Review and Meta-Analysis
Article information
Abstract
Objective
This meta-analysis aims to refine the understanding of the optimal choice between different cage shapes in transforaminal lumbar interbody fusion (TLIF) by systematically comparing perioperative data, radiological outcomes, clinical results, and complications associated with banana-shaped and straight bullet cages.
Methods
A meticulous literature search encompassing PubMed, Embase, Scopus, Web of Science, China Knowledge Network, and Wanfang Data was executed up to October 5, 2023. Inclusion criteria focused on studies comparing banana-shaped and straight bullet cages in TLIF. The quality of included studies was assessed using appropriate tools such as the Newcastle-Ottawa Scale (NOS) for nonrandomized studies. Rigorous evaluations were performed for radiographic outcomes, including disc height (DH), segmental lordosis (SL), lumbar lordosis (LL), subsidence, and fusion rates. Clinical outcomes were meticulously evaluated using visual analogue scale (VAS), Oswestry Disability Index (ODI), and complications.
Results
The analysis incorporated 7 studies, involving 573 patients (297 with banana-shaped cages, 276 with straight cages), all with NOS ratings exceeding 5 stars. No statistically significant differences were observed in operative time, blood loss, or hospitalization between the 2 cage shapes. Banana-shaped cages exhibited greater changes in DH (p = 0.001), SL (p = 0.02), and LL (p = 0.01). Despite statistically higher changes in ODI for straight cages (26.33, p < 0.0001), the actual value remained similar to banana-shaped cages (26.15). Both cage types demonstrated similar efficacy in VAS, complication rates, subsidence, and fusion rates.
Conclusion
Although banana-shaped cages can excel in restoring DH, SL, and LL, straight bullet cages can provide comparable functional improvements, pain relief, and complication rates.
INTRODUCTION
Transforaminal lumbar interbody fusion (TLIF) is a firmly established surgical procedure employed in the management of various lumbar spinal pathologies. These include conditions such as degenerative disc disease, spinal stenosis, and spondylolisthesis [1-3]. TLIF involves the placement of interbody cages within the intervertebral space, which facilitates fusion, restores vertebral height, and decompresses neural structures [4,5]. The choice of cage type, whether banana-shaped or straight bullet cages, has garnered considerable interest in recent years due to its potential impact on clinical and radiological outcomes [6,7].
Numerous studies have explored the advantages and disadvantages of these different cage shapes, with proponents and sceptics on both sides [8-10]. Both cage types aim to maximize endplate contact and minimize risk of subsidence. However, whether cage geometry impacts clinical outcomes remains debated. Some studies report greater improvements in pain and disability scores with banana-shaped cages, attributed to better restoration of segmental alignment and disc height (DH) [11-13]. Other reports show no differences [9]. The ongoing debate surrounding the clinical efficacy and radiological performance of these cage types has led to the need for a comprehensive assessment through meta-analysis.
This meta-analysis aims to provide a comprehensive evaluation of the differences in clinical and radiographic outcomes between banana-shaped and straight bullet cages according to the published literature. The results will help guide surgical decision making and cage selection to optimize patient outcomes after TLIF procedures.
MATERIALS AND METHODS
1. Study Selection
1) Search strategy
The present meta-analysis adhered to the stringent guidelines defined in the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [14], ensuring a comprehensive and rigorous approach to the research synthesis process. A comprehensive literature search was conducted in multiple electronic databases, including PubMed, Embase, Scopus, Web of Science, China Knowledge Network, and Wanfang Data. The search strategy involved a combination of keywords and MeSH (medical subject headings) terms related to “Banana-Shaped,” “Straight,” “Bullet,” “Steerable,” “Cage,” “Transforaminal Lumbar Interbody Fusion,” and “TLIF.” Search for studies published on 5 October 2023.
2) Inclusion criteria
(1) Studies comparing banana-shaped and straight bullet cages in TLIF (1, the presence of unstable low-grade spondylolisthesis [Meyerding grade I or II] of either isthmic or degenerative origin; 2, foraminal stenosis with central stenosis, degenerative disc disease, or recurrent disc herniation; and 3, persistence of symptoms that correlated with radiological findings despite undergoing conservative treatment for a minimum duration of 6 weeks). (2) Studies reporting clinical outcomes (e.g., pain scores, functional improvement) and radiological outcomes (e.g., DH, lumbar lordosis [LL], segmental lordosis [SL], cage subsidence, fusion rates) or providing data from which these outcomes could be calculated. (3) Articles published in English or Chinese.
3) Exclusion criteria
(1) Encompassed patients with metabolic bone disease, infection, spinal trauma, and tumors. (2) Compassed case reports, reviews, correspondence, conference abstracts, and studies that lacked the necessary data for a detailed analysis.
2. Data Extraction
The data retrieval of the encompassed studies adhered to a standardized extraction form designed for this purpose. The extracted data were classified into 2 distinct components for subsequent analysis. The first included details of the baseline study, specifically author names, publication year, journal title, study design, sample size, patient age, operating levels, and cage height. The second component consisted of perioperative parameters (operative duration, estimated blood loss, hospital stay), clinical outcomes (visual analogue scale [VAS] pain scores, Oswestry Disability Index [ODI] functional scores, complication incidence), and radiographic evaluations (DH, SL, LL, spinopelvic parameters, cage subsidence, depth of cage migration, and fusion rates).
Two impartial reviewers conducted a meticulous selection of the identified studies, initially assessing them based on titles and abstracts. Subsequently, the full text articles of potentially eligible studies were systematically evaluated for definitive inclusion. In the event that any disparities arise during data extraction, these were judiciously resolved through discussion and mutual consensus between the 2 investigators.
3. Quality Assessment and Publication Bias
The methodological quality of included studies was assessed using appropriate tools such as Newcastle-Ottawa Scale (NOS) for nonrandomized studies [15]. Consistent with pre-established rating criteria, studies that attained or surpassed a predefined threshold of 5 “stars” were accorded the distinction of being categorized as high-quality literature. Additionally, Egger test was applied to identify possible publication bias. This meta-analysis employed the Grading of Recommendations Assessment, Development and Evaluation (GRADE) method to evaluate the credibility of the evidence presented in the pooled results. The quality of the evidence was classified into 4 levels: high, moderate, low, and very low based on considerations such as the risk of publication bias, outcomes, and treatment effects.
4. Statistical Analysis
Statistical meta-analyses were performed using Review Manager 5.3 (Cochrane Collaboration, Oxford, UK). For continuous data, the weighted mean difference (WMD) and the 95% confidence interval (CI) were calculated. Dichotomous outcomes were expressed as odds ratio (OR) with 95% CI. Heterogeneity was assessed using the chi-square (Q) test. In the absence of statistical heterogeneity (p > 0.1, I2 < 50%), a fixed effects model was used for pooling. In contrast, in the presence of substantial heterogeneity (p < 0.1, I2 ≥ 50%), sensitivity analyses were performed to explore sources of variability. On the basis of these findings, subgroup analyses were subsequently performed. When an underlying cause for heterogeneity could not be identified, a random effects model was applied for meta-analysis or, in some cases, pooling was abandoned in favor of descriptive analysis alone. A leave-one-out analysis was conducted on outcomes with I2 ≥ 50%. Statistical significance was defined as p < 0.05.
To evaluate publication bias, funnel plots providing visual representations of asymmetry were included as part of the analytical process.
RESULTS
1. Search Results and Study Characteristics
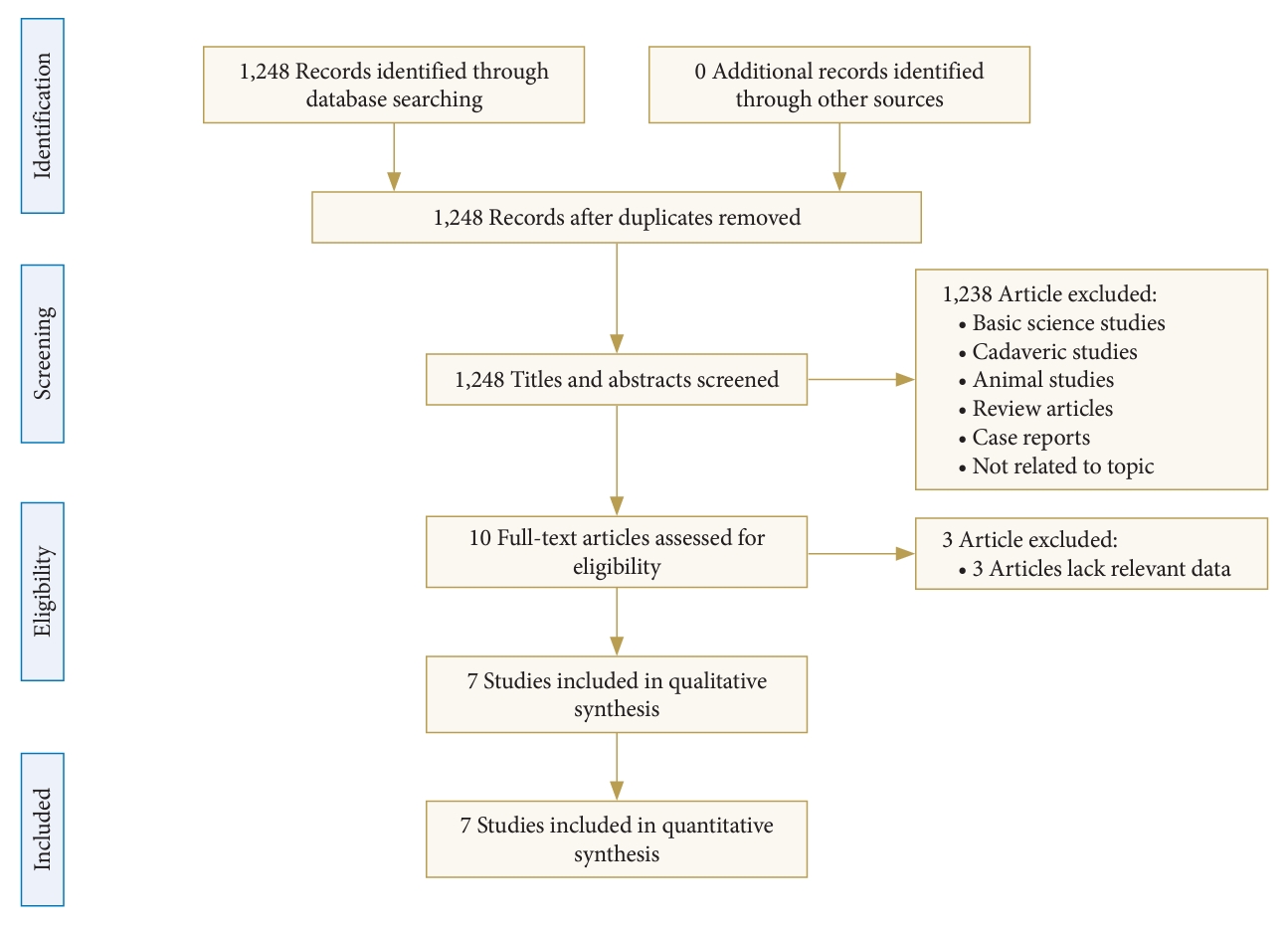
The comprehensive literature search yielded 7 studies meeting predetermined inclusion criteria for quantitative analysis [8,9,11-13,16,17]. The literature search identified 7 retrospective comparative studies that met the eligibility criteria, which were included for quantitative synthesis (Fig. 1).
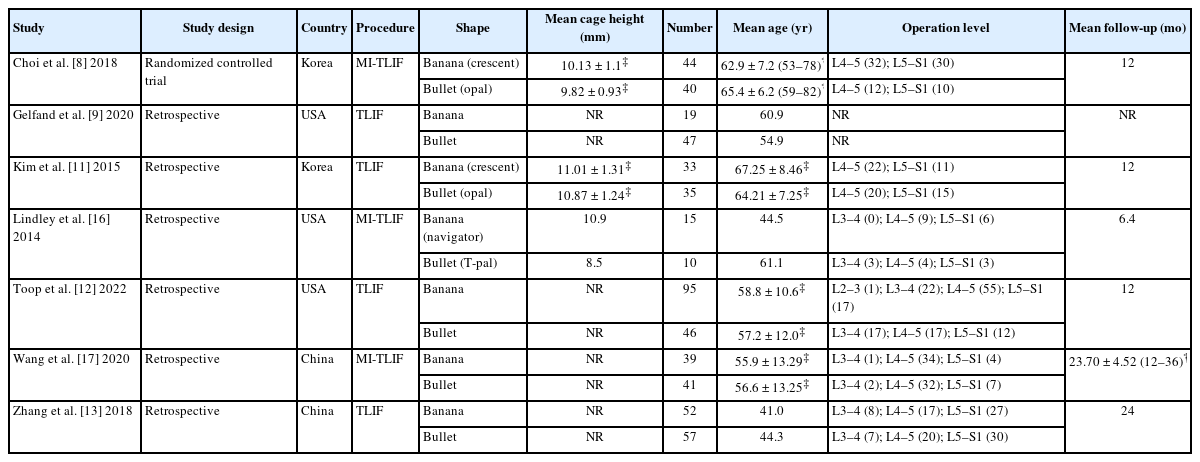
Table 1 summarizes the key characteristics of the included retrospective comparative studies. The cumulative study population in all included studies consisted of 573 subjects who underwent TLIF. Of these, 297 subjects were treated with banana-shaped interbody cages and 276 subjects received straight bullet-shaped interbody cages. Regarding study locations, 3 studies originated in the United States, 2 were conducted in China, and 2 in South Korea. Among the combined study cohorts, the level of the lumbar spinal that was the most frequently undergoing TLIF was L4–5. The mean height of the inserted cage used intraoperatively was 10.68 mm in the banana-shaped cage group compared to 9.73 mm in the straight bullet-shaped cage group.
2. Perioperative Measurements
1) Mean operative time (minutes)
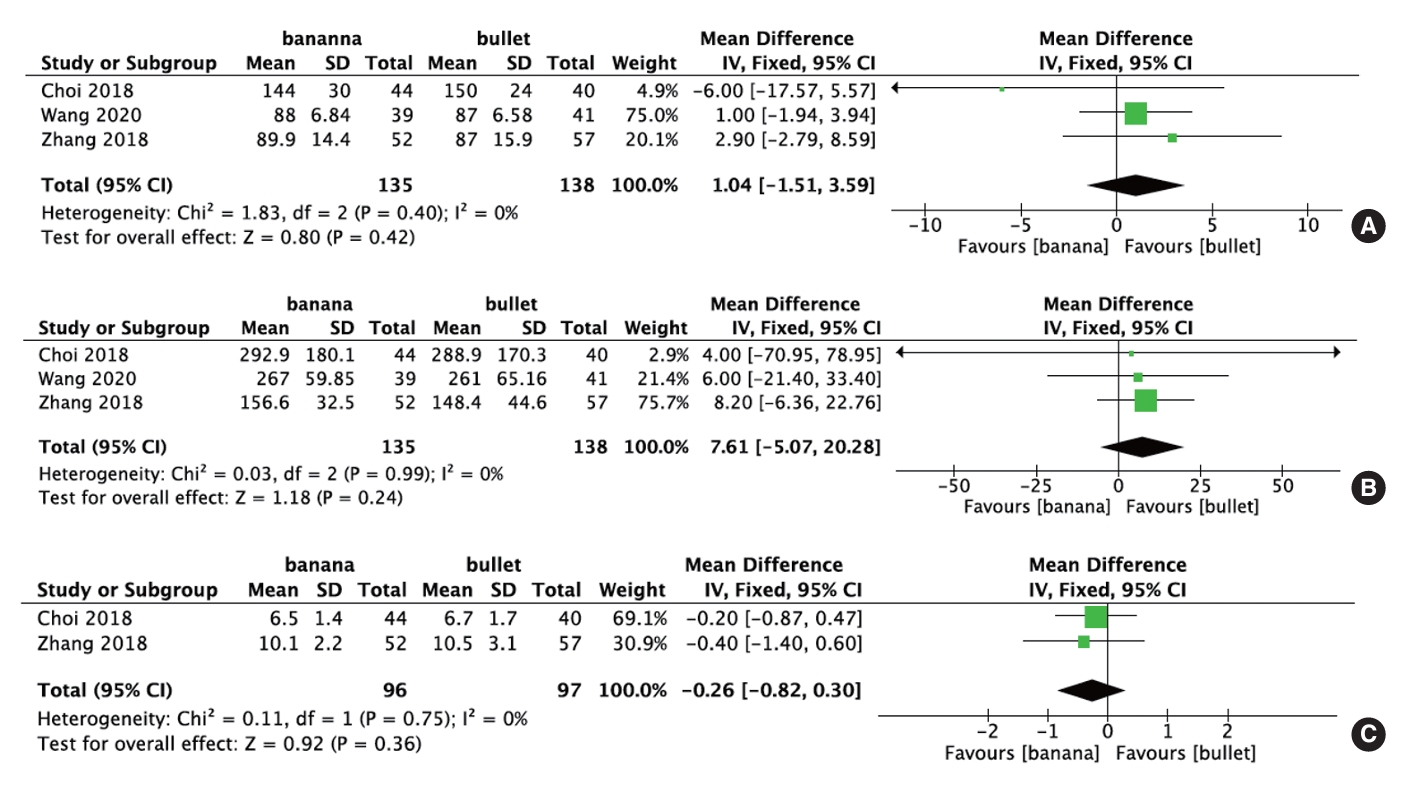
Three independent studies, comprising a total of 273 subjects, provided data on the mean duration of the operation. The results of this analysis revealed a lack of statistically significant differences between the use of straight bullet cages and banana-shaped cages in terms of operating time (p = 0.42; WMD, 1.04; 95% CI, -1.51 to 3.59) (Fig. 2A).
2) Estimated blood loss (mL)
Three independent studies, which comprised a collective cohort of 273 subjects, provided data on the estimated mean blood loss. The findings of this investigation indicated a lack of statistically significant distinctions between the use of straight bullet cages and banana-shaped cages in relation to blood loss (p = 0.24; WMD, 7.61; 95% CI, -5.07 to 20.28) (Fig. 2B).
3) Hospital length of stay (days)
Two distinct studies, encompassing a total of 193 subjects, contributed data concerning the mean duration of hospitalization. The results derived from this examination revealed a lack of statistically significant distinctions between the use of straight bullet cages and banana-shaped cages with respect to hospital stay (p = 0.36; WMD, -0.26; 95% CI, -0.82 to 0.30) (Fig. 2C).
3. Clinical Outcomes
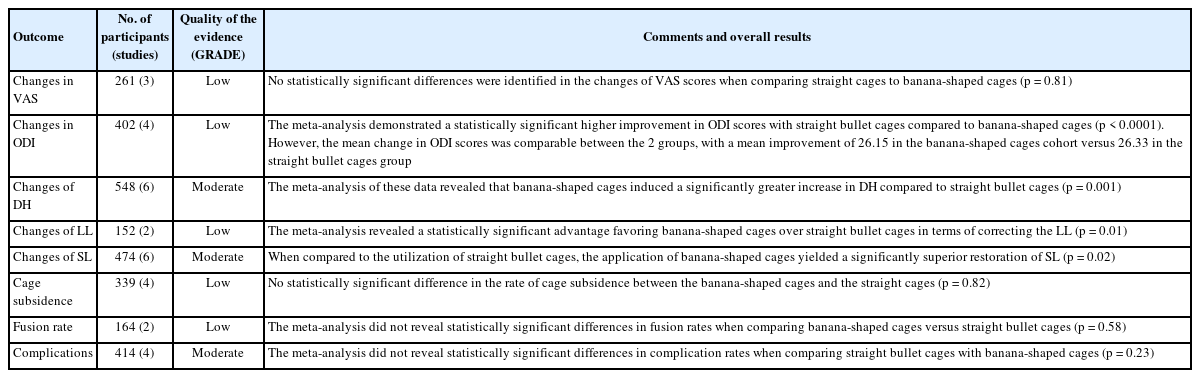
1) Changes in VAS
Three studies comprising 261 patients reported VAS scores before and after surgery. Meta-analysis did not demonstrate statistically significant differences in the changes in VAS scores when comparing straight bullet cages versus banana-shaped cages (p = 0.81; WMD, 0.08; 95% CI, -0.57 to 0.73) (Fig. 3A).
Forest plots comparing changes in VAS (A), changes in ODI (B), and complications (C) between banana-shaped cages and straight bullet cages in transforaminal lumbar interbody fusion. VAS, visual analogue scale; ODI, Oswestry Disability Index; SD, standard deviation; IV, inverse variance; M-H, Mantel-Haenszel; CI, confidence interval; df, degrees of freedom.
2) Changes in ODI
Four studies comprising 402 patients provided preoperative and postoperative ODI scores. Meta-analysis revealed a statistically significant increase in ODI scores with straight bullet cages compared to banana-shaped cages after TLIF (p < 0.0001; WMD, -2.54; 95% CI, -3.12 to -1.96) (Fig. 3B). However, the mean change in ODI scores was comparable between the groups, with a mean improvement of 26.15 in the banana-shaped cage cohort versus 26.33 in the straight bullet cage group.
3) Complications
Four studies comprising 414 patients reported postoperative complication data. The meta-analysis did not reveal statistically significant differences in complication rates when comparing bullet cages with banana-shaped cages (p = 0.23; OR, 0.60; 95% CI, 0.27–1.37) (Fig. 3C).
4. Radiographic Assessments
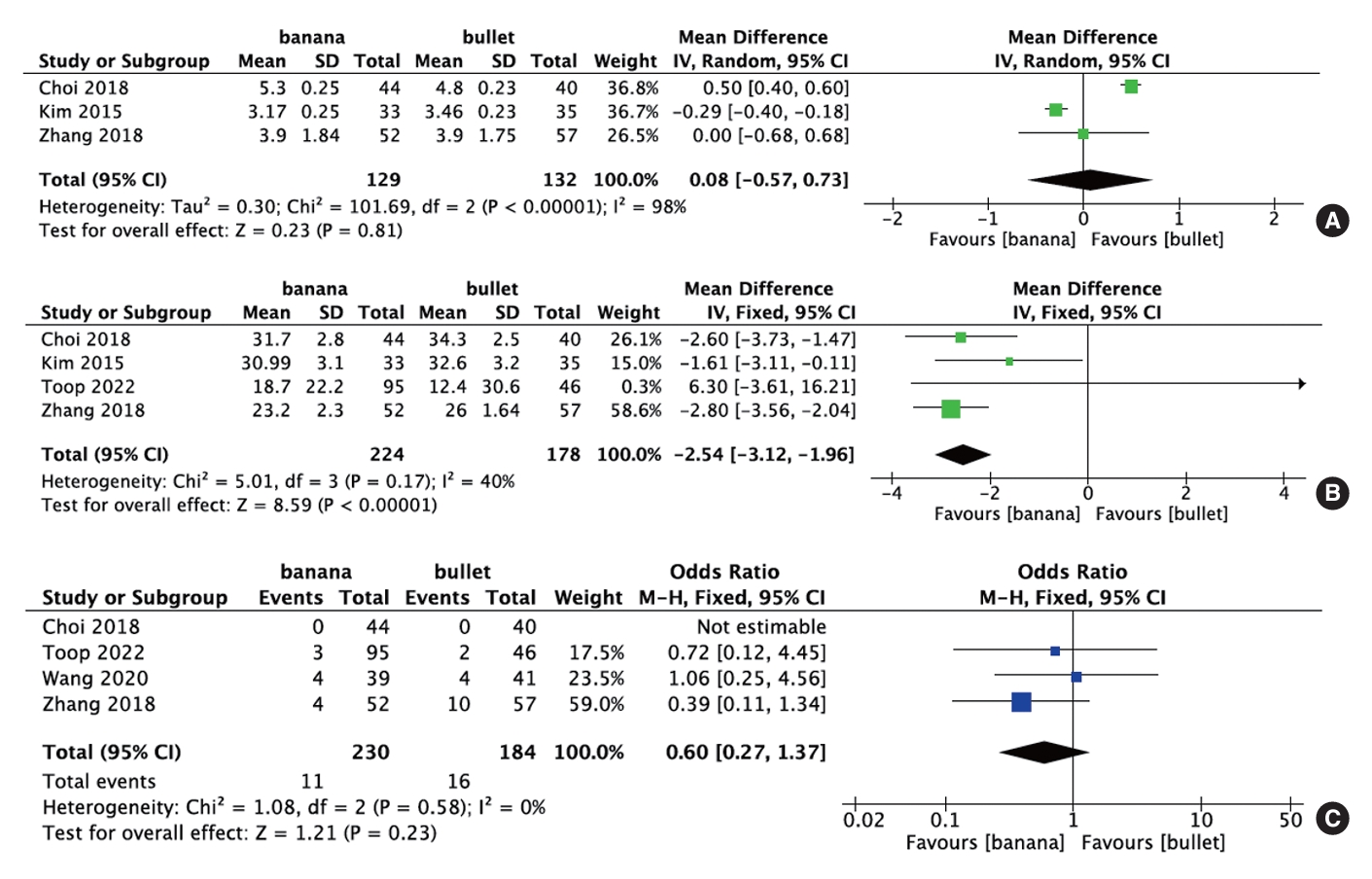
1) Changes in DH
Six studies comprising 548 patients reported preoperative and postoperative DH. Meta-analysis of these data showed that banana-shaped cages caused a significantly greater increase in postoperative DH compared to straight bullet cages (p = 0.001; WMD, 0.54; 95% CI, 0.21–0.87) (Fig. 4A).
Forest plots comparing changes in disc height (A), changes in lumbar lordosis (B), and segmental lordosis (C) between banana-shaped cages and straight bullet cages in transforaminal lumbar interbody fusion. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
2) Changes in LL
Two studies involving a cohort of 152 patients provided preoperative and postoperative LL data. Subsequent meta-analysis revealed a statistically significant advantage favoring banana-shaped cages over straight bullet cages in terms of correcting the lumbar lordotic angle (p = 0.01; WMD, 7.61; 95% CI, -5.07 to 20.28) (Fig. 4B).
3) Changes in SL
Incorporating data from 6 distinct studies involving a total of 474 patients, this analysis included preoperative and postoperative measurements of SL. The results of this comprehensive investigation demonstrated that, compared to the use of straight bullet cages, the application of banana-shaped cages produced a significantly superior restoration of SL (p = 0.02; WMD, 2.39; 95% CI, 0.33–4.44) (Fig. 4C).
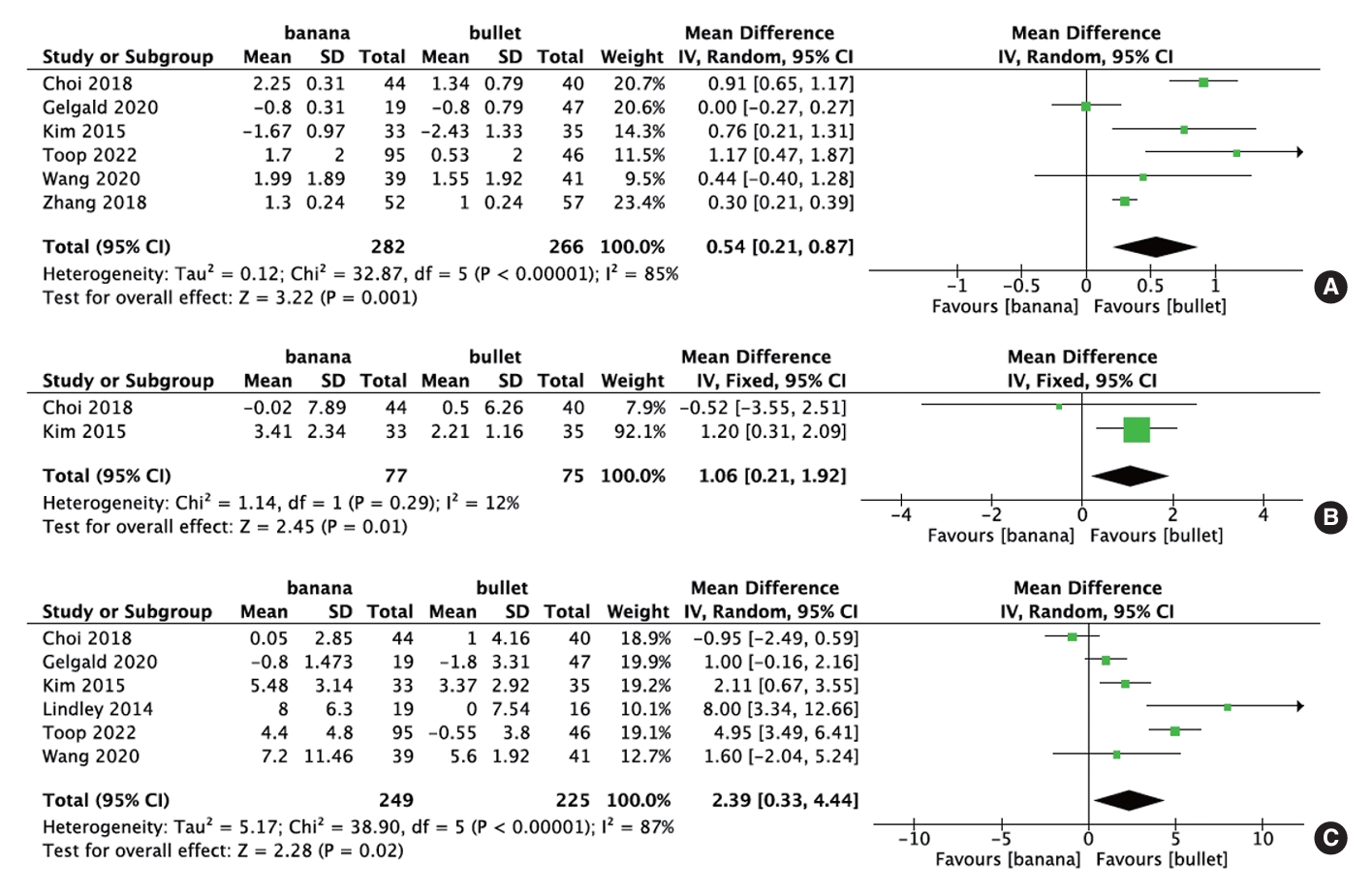
4) Changes in spinopelvic sagittal parameters
Two studies comprising 152 patients evaluated preoperative and postoperative pelvic tilt. The meta-analysis did not show statistically significant differences in changes in pelvic tilt when comparing straight bullet cages versus banana-shaped cages for TLIF (p = 0.84; WMD, -0.19; 95% CI, -2.00 to 1.62) (Fig. 5A).
Forest plots comparing changes in pelvic tilt (A), changes in pelvic incidence (B), and sacral slope (C) between banana-shaped cages and straight bullet cages in transforaminal lumbar interbody fusion. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
Two studies, including 152 patients, evaluated preoperative and postoperative pelvic incidence. The meta-analysis did not reveal statistically significant differences in changes in pelvic incidence when comparing straight bullet cages with banana-shaped cages (p = 0.47; WMD, -0.14; 95% CI, -0.51 to 0.23) (Fig. 5B).
Two studies including 152 patients evaluated preoperative and postoperative sacral slope. The meta-analysis did not reveal statistically significant differences in sacral slope changes when comparing straight bullet cages versus banana-shaped cages (p = 0.72; WMD, 0.31; 95% CI, -1.37 to 1.99) (Fig. 5C).
5) Cage subsidence
Four studies comprising 339 subjects provided postoperative cage subsidence data. The results of our meta-analysis indicate that there was no statistically significant difference in the subsidence rate of the cage between the banana-shaped cages and the straight fusion cage after the surgical procedure (p = 0.82; OR, 0.86; 95% CI, 0.23–3.26) (Fig. 6A).
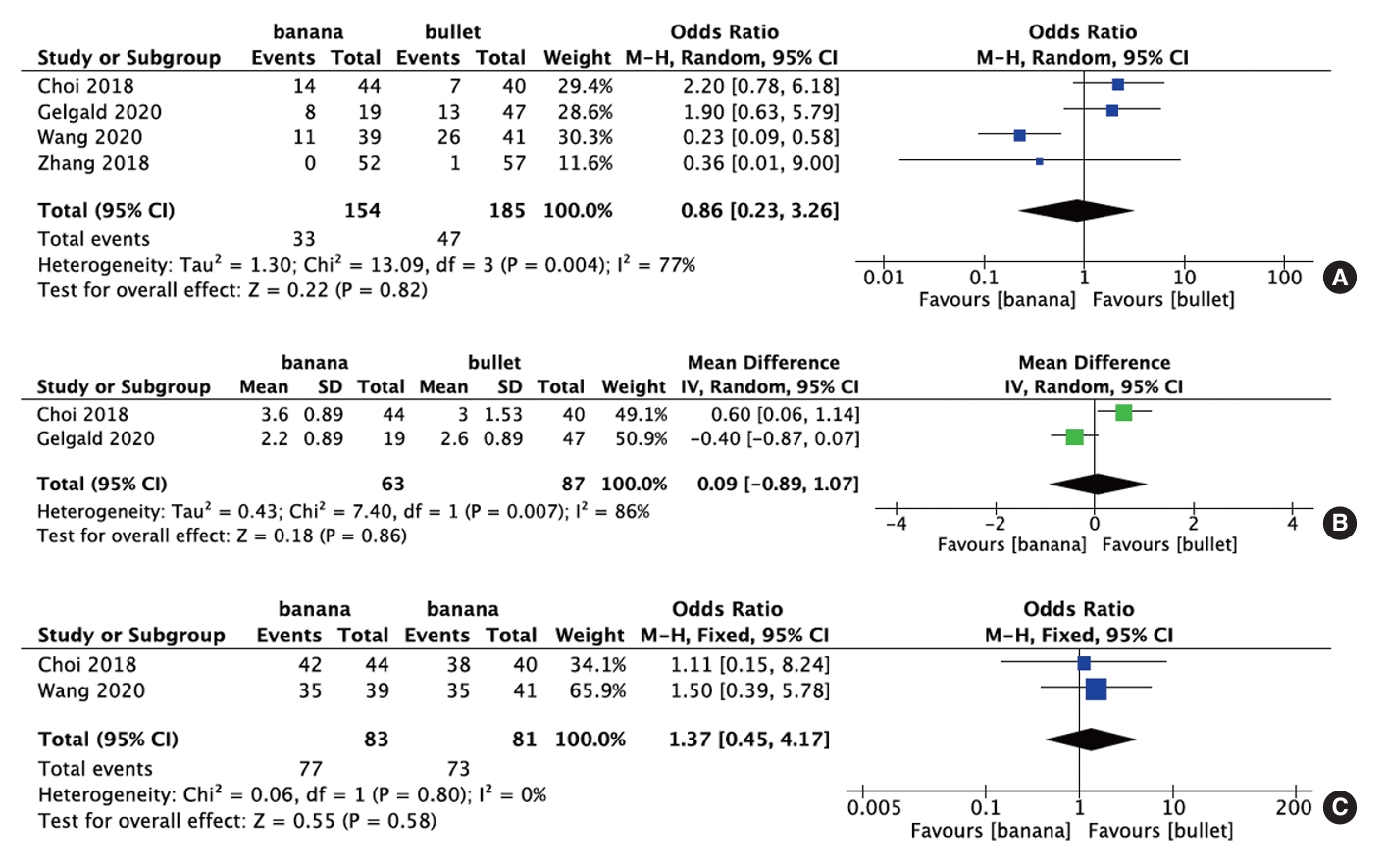
Forest plots comparing cage subsidence (A), depth of cage migration (B), and fusion rate (C) between banana-shaped cages and straight bullet cages in transforaminal lumbar interbody fusion. SD, standard deviation; IV, inverse variance; M-H, Mantel-Haenszel; CI, confidence interval; df, degrees of freedom.
Two studies comprising 150 subjects provided data on the depth of cage migration. The meta-analysis did not show significant differences in the depth of subsidence when comparing banana-shaped cages versus straight bullet cages (p=0.86; WMD, 0.09; 95% CI, -0.89 to 1.07) (Fig. 6B).
6) Fusion
Two studies comprising 164 patients reported fusion rates (12 months postoperatively). The meta-analysis did not reveal statistically significant differences in fusion rates when comparing banana-shaped cages versus straight bullet cages (p = 0.58; WMD, 1.37; 95% CI, 0.45–4.17) (Fig. 6C).
5. Quality Analysis and Publication Bias
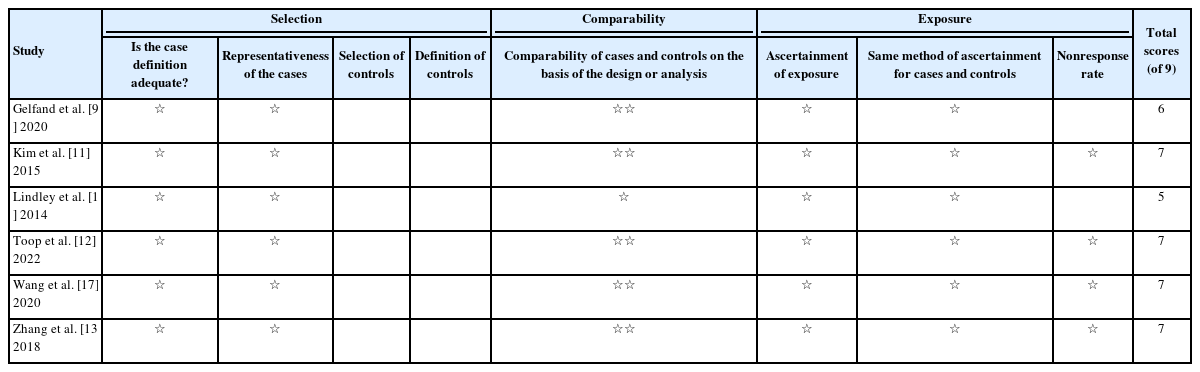
The results of the risk of bias assessment for all included studies are summarized in Table 2. Importantly, each study met the predetermined quality threshold of 5 or more stars on the NOS, reflecting the overall high methodological quality of the evidence synthesized in this meta-analysis (Supplementary Table 1).
Publication bias was evaluated by visual inspection of a funnel plot using changes in DH as an example outcome (Supplementary Fig. 1). The scatterplot showed general symmetry within the funnel plot, indicating a low risk of publication bias. Further, the Egger test method detects publication bias (Supplementary Fig. 2). According to leave-one-out analysis (Supplementary Fig. 3), a notable alteration in the results following the exclusion of papers by Choi et al. [8] implies a potential lack of robustness in the meta-analysis of changes in VAS. Leave-one-out analysis for DH, SL, and subsidence indicated stability, with no discernible impact on the overall results.
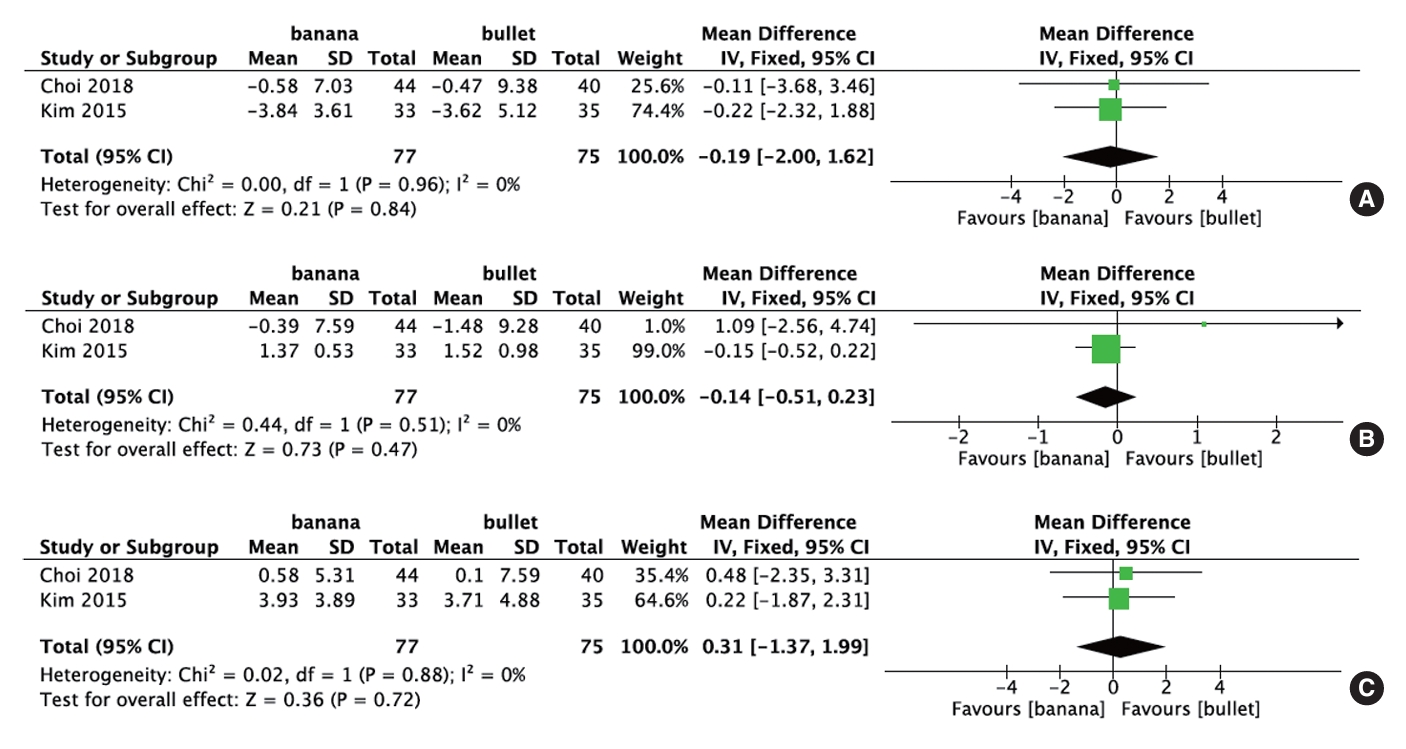
The overall assessment of the results using the GRADE approach is described in Table 3.
DISCUSSION
The utilization of various interbody fusion cages within the TLIF procedure has the potential to yield distinct results (Supplementary Table 2). Several studies have been conducted in this regard, revealing varying and inconsistent results [9,18-20]. Therefore, the main objective of this meta-analysis was to systematically assess and compare the clinical and radiological outcomes attributed to the deployment of straight and banana-shaped cages in the context of TLIF. This comprehensive assessment seeks to improve our knowledge and provide a more informed understanding of the relative advantages and potential implications associated with these 2 types of cages in the field of TLIF.
A previous meta-analysis showed that straight bullet cages provided better recovery of DH and SL after TLIF compared to banana-shaped cages [10]. However, the present study is contrary to the results of the previous study. Our meticulous analysis revealed that postoperative recovery of essential radiographic parameters, particularly DH, SL, and LL, showed a superior trend in cases involving the deployment of banana-shaped cages in contrast to their straight bullet cage counterparts. There are several potential explanations for the observed findings which we aimed to summarize and analyze as follows. First, the superior postoperative SL and LL associated with the banana-shaped cage can be attributed to its inherent design of the anterior convexity angle. Second, an additional point to consider is the slightly higher mean inserted cage height used in banana-shaped cages (10.68 mm) compared to straight bullet cages (9.73 mm), although this difference did not reach statistical significance. Although not definitive, this finding suggests that the greater distraction from disc space and the SL achieved with banana-shaped cages could be partially attributed to the larger heights used, rather than to the geometry of the cage alone. Lastly, the more anterior positioning of the banana-shaped cage within the disc space, as compared to the straight bullet cage, facilitates greater recovery of the SL. Furthermore, this anterior placement of the cage plays a role in reducing the probability of the cage subsidence. Previous studies have consistently indicated that the anterior and posterior portions of the endplate exhibit greater structural robustness compared to central position [21,22]. The subcutaneous caesarean section is a critical concern in spinal fusion surgery, as it can lead to loss of DH and spinal alignment. Our analysis did not identify a significant difference in cage subsidence rates between the 2 cage types.
In theory, banana-shaped cages have the potential for a higher fusion rate compared to bullet-shaped cages. This is because banana-shaped cages require thorough removal of both the ipsilateral and contralateral anterior discs during implantation, which ultimately facilitates the incorporation of more autogenous bone around the cage and a larger graft footprint, which is advantageous for improving fusion rates [6]. Our study found that there were no significant differences in fusion rates between the 2 groups, both achieving a rate of 90%. However, it should be noted that this may be attributed to the limited number of studies reporting fusion rates as an outcome, as only 2 articles [8,17] were available for analysis.
Patients with spinal disorders seek surgery primarily to alleviate discomfort. This meta-analysis did not find significant differences in pain relief between banana-shaped and straight bullet cages. This suggests that both types of cages effectively achieve equivalent decompression effects and spinal stabilization. The lack of significant differences in VAS underscores the importance of addressing the primary clinical concern, which is pain relief, rather than focusing solely on the geometry of the cages. Although banana-shaped cages theoretically offer advantages such as better anatomical fit and indirect foraminal decompression, these advantages may not translate into meaningful long-term clinical benefits compared to straight bullet cages.
However, the analysis of ODI scores yielded different results. Patients who received straight bullet cages exhibited a significantly greater improvement in ODI scores compared to those who received banana-shaped cages. This finding suggests that straight bullet cages may offer advantages in terms of functional recovery and quality of life, as reflected by reduced disability levels. However, it is important to note that the clinical significance of this difference, although statistically significant, may not be substantial. This is because the mean change in the ODI scores was comparable between the 2 groups, with a mean improvement of 26.15 in the banana-shaped cage cohort versus 26.33 in the straight bullet cage cohort. Despite statistical significance, the small absolute difference in disability change scores suggests a minimal clinical distinction between the 2 cage types to improve functional impairment after TLIF.
Perioperative data constitute critical clinical information to assess any surgical intervention, including TLIF. Our meta-analysis did not demonstrate statistically significant differences in operative duration, intraoperative blood loss, or postoperative hospital stay when comparing banana-shaped versus straight bullet cages. This suggests that cage geometry does not substantially influence these intraoperative metrics. Surgeons can select between these 2 cage configurations for TLIF procedures without concern for adverse impacts on procedural times, blood loss risk, or hospitalization needs postoperatively. Patient comorbidities, nuances of surgical technique, and standardized postoperative protocols likely exert greater effects on perioperative outcomes. Our findings imply that cage choice should be dictated by other radiographic and clinical factors, without fear of negatively affecting key perioperative parameters. More research is still warranted to definitively establish the comparability of banana and straight TLIF cages with respect to operating times, blood loss, and hospital stays using high-quality comparative trials with larger sample sizes.
Insertion techniques differ between bullet-shaped and banana-shaped interbody cages in TLIF procedures. The banana-shaped cage is introduced through a posterolateral approach, advanced anteriorly, rotated laterally, and then advanced further into position. This multistep process aims to locate the contoured banana-shaped cage so that it matches the angle and curvature of the natural disc. On the contrary, the straight bullet cage can be inserted directly into the contralateral anterolateral corner of the intervertebral space in one simple motion during implantation. This streamlined insertion technique for bullet cages may confer an advantage by reducing surgical strain on neural structures and dura. The resulting decreases in intraoperative manipulation and tension could hypothetically reduce the risks of inadvertent epidural fibrosis or dural injury as potential postoperative complications. Contrary to the theoretical risks described above, our meta-analysis found no significant differences in postoperative complication rates when comparing bullet-shaped cages versus banana-shaped cages, based on data from the 4 included studies. Despite potential variations in procedural insertion techniques between these 2 cage types, the current quantitative evidence synthesis does not demonstrate a significant effect on the incidence of complications.
The present study has several notable strengths. Specifically, it exclusively incorporates studies that directly compare banana-shaped and straight bullet cages in TLIF procedures, thus mitigating the risks associated with surgical and matching bias. Furthermore, the screening process used is notably stringent and selective. However, certain limitations are intrinsic to this investigation. First, the overall number of studies included in this analysis is rather limited, comprising a total of 7 studies with only 573 patients enrolled. This limited sample size imparts reduced statistical power, potentially impairing the ability to discern subtle differences between the 2 groups. Second, the paucity of high-quality research is evident, as only one study assumes the form of a randomized controlled trial, while the remainder adopt a retrospective design. Third, divergence in the measurement methodologies for key metrics, including DH and subsidence, within the raw data, coupled with the nonuniformity of surgical segments, may introduce potential sources of heterogeneity in pooled results within the meta-analysis. Finally, the data amalgamated for analysis were aggregated, preventing access to individual patient data and consequently limiting the scope for a more comprehensive analysis.
CONCLUSION
In the context of patients undergoing TLIF surgery, a review of existing evidence suggests that banana-shaped cages exhibit a superior capacity to recover radiographic parameters, particularly DH, SL, and LL, compared to their straight bullet cages. However, it should be noted that banana-shaped and straight-shaped cages appear to produce similar results in terms of pain alleviation, the incidence of complications, the maintenance of sagittal alignment, subsidence rates, and the achievement of fusion success.
To provide further insight into this matter, it is imperative that future investigations involve additional extensive prospective randomized trials, encompassing a broader spectrum of clinical and imaging parameters.
Supplementary Material
Supplementary Tables 1, 2 and Figs. 1-3 can be found via https://doi.org/10.14245/ns.2347078.539.
Detailed evaluation rationale for each column of the NOS rating
Characteristics of banana-shaped cage and straight bullet cage
Funnel plots of changes in disc height. SE, standard error; MD, mean difference.
Egger test for publication bias. (A) Mean operative time. (B) Mean estimated blood loss. (C) Change of disc height. (D) Change of segmental lordosis. (E) Change of VAS. (F) Change of ODI. (G) Subsidence. (H) Complications. The p-value of the Egger test for all groups except the (F) was greater than 0.05. VAS, visual analogue scale; ODI, Oswestry Disability Index.
The “leave-one-out” sensitivity analysis was conducted to assess the stability of the results. A noteworthy alteration in the results following the exclusion of papers by Choi et al. implies a potential lack of robustness in the meta-analysis of changes in visual analogue scale (A). The leave-one-out analysis for disc height (B), segmental lordosis (C), and subsidence (D) indicated stability, with no discernible impact on the overall results.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This research was funded by the Natural Science Foundation of Fujian Province, grant number 2021J05282; funded by Xiamen Municipal Bureau of Science and Technology (3502Z20224033). The funder had no role in the design of the study or collection, analysis, or interpretation of data or in writing the manuscript.
Author Contribution
Conceptualization: GXL; Data curation: LRH; Formal analysis: JNN; Funding acquisition: WBX, KX, ZQ; Methodology: WBX, ZQ; Project administration: MTZ; Visualization: SWJ; Writing - original draft: GXL; Writing - review & editing: CMC, GR.
Acknowledgements
The author Guang-Xun Lin would like to give thanks for the “Xiamen Health High-Level Talent Training Program (2021).”