Prognostic Value in Preoperative Veterans RAND-12 Mental Component Score on Clinical Outcomes for Patients Undergoing Minimally Invasive Lateral Lumbar Interbody Fusion
Article information
Abstract
Objective
To evaluate the effect of Veterans RAND 12-item health survey mental composite score (VR-12 MCS) on postoperative patient-reported outcome measures (PROMs) after undergoing lateral lumbar interbody fusion.
Methods
Retrospective data from a single-surgeon database created 2 cohorts: patients with VR-12 MCS ≥ 50 or VR-12 MCS < 50. Preoperative, 6-week, and final follow-up (FF)- PROMs including VR-12 MCS/physical composite score (PCS), 12-item Short Form health survey (SF-12) MCS/PCS, Patient-Reported Outcomes Measurement Information System Physical Function (PROMIS-PF), Patient Health Questionnaire-9 (PHQ-9), visual analogue scale (VAS)-back/leg pain (VAS-BP/LP), and Oswestry Disability Index (ODI) were collected. ∆6-week and ∆FF-PROMs were calculated. Minimal clinically important difference (MCID) achievement rates were determined from established cutoffs from the literature. For intercohort comparison, chi-square analysis was used for categorical variables, and Student t-test for continuous variables.
Results
Seventy-nine patients were included; 25 were in VR-12 MCS < 50. Mean postoperative follow-up time was 17.12 ± 8.43 months. The VR-12 MCS < 50 cohort had worse VR-12 PCS, SF-12 MCS, PROMIS-PF, PHQ-9, VAS-BP, and ODI scores preoperatively (p ≤ 0.014, all), worse VR-12 MCS/PCS, SF-12 MCS, PROMIS-PF, PHQ-9, and ODI scores at 6-week postoperatively (p ≤ 0.039, all), and worse VR-12 MCS, SF-12 MCS, PROMIS-PF, PHQ-9, VAS-BP, VAS-LP, and ODI scores at FF (p ≤ 0.046, all). The VR-12 MCS < 50 cohort showed greater improvement in VR-12 MCS and SF-12 MCS scores at 6 weeks and FF (p ≤ 0.005, all). The VR-12 MCS < 50 cohort experienced greater MCID achievement for VR-12 MCS, SF-12 MCS, and PHQ-9 (p ≤ 0.006, all).
Conclusion
VR-12 MCS < 50 yielded worse mental health, physical function, pain and disability postoperatively, yet reported greater improvements in magnitude and MCID achievement for mental health.
INTRODUCTION
Lateral lumbar interbody fusion (LLIF) is a widely used and effective surgical technique in the treatment of many different spinal pathologies. In an LLIF, the disc space is accessed via a retroperitoneal approach and has greater potential for improving lordosis. Further, this technique allows for stronger constructs to be implanted compared to other interbody fusion techniques [1,2]. While LLIF is highly efficacious, current spine literature has demonstrated that preoperative mental health scores (Patient Health Questionnaire-9 [PHQ-9], 12-item Short Form health survey [SF-12] mental composite score [MCS], 36-item Short Form health survey [SF-36] MCS) may influence postoperative patient-reported outcome measures (PROMs) across many spine surgeries [2-5]. As such, an accurate understanding on the impact of a patient’s reported psychological state on outcomes following LLIF is imperative [3-5].
Several established and emerging PROMs exist to evaluate a patient’s mental health [6]. One such PROM is the Veterans RAND 12-item health survey (VR-12); a health questionnaire that aims to measure a patient’s perspective on their health-related quality of life [6,7]. The questionnaire consists of 12 items that are used to calculate a physical composite score (PCS) and MCS and allows for 8 major domains to be assessed; general health perceptions, physical functioning, role limitations due to physical and emotional problems, bodily pain, energy-fatigue, social functioning and mental health [6-8]. Data show that the VR-12 MCS is an accurate assessment tool for mental health as it is highly correlated with widely accepted PROMs such as Patient Health Questionnaire-9 (PHQ-9), SF-12 MCS, and SF-36 MCS [8-12]. However, limited data exist on the prognostic value of VR-12 MCS for outcomes postoperatively for spine surgery – specifically for lumbar fusion.
As such, the goal of this study will be to evaluate the influence of and associations between preoperative VR-12 MCS on postoperative PROMs in patients undergoing elective LLIF.
MATERIALS AND METHODS
1. LLIF Technique
Patients are placed in a lateral decubitus position with the greater trochanter aligned with the table break. Depending on coronal plane deviation, either a left or right lateral decubitus position can be used. Once the patient is aligned, the table is manipulated to flex the patient’s body, improving access to the disc space by increasing the distance between the iliac crest and ribs.
Minimally invasive techniques were utilized by the surgeon in this study. An oblique incision is made that spans from the anterior superior border of the caudal vertebrae to the posterior inferior border of the cephalic vertebrae. If several levels are being fused, the incision spans from the most caudal to the most cephalic vertebrae. Blunt dissection is used to expose the psoas muscle, and special attention is given to protect the iliohypogastric and ilioinguinal nerves. A transpsoatic incision is made ventral to the roots of the lumbar plexus, which are identified using neuromonitoring.
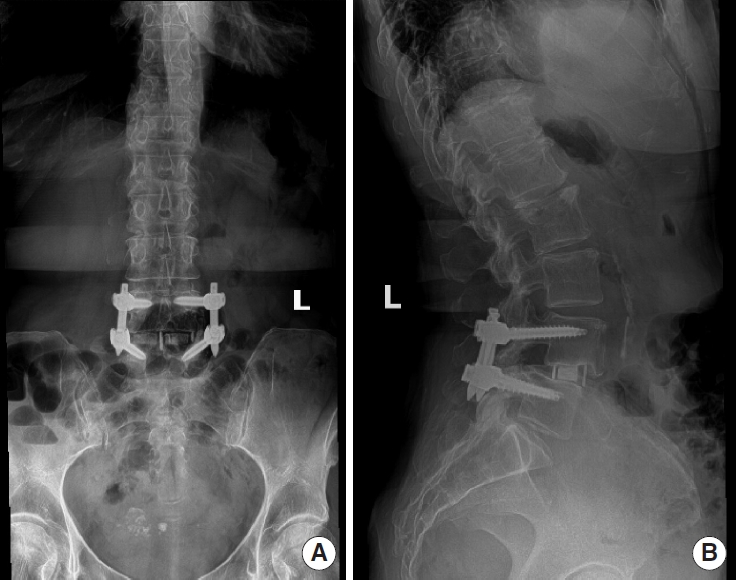
The disc space is then identified and confirmed by placing a probe in the disc space and visualizing positioning via fluoroscopy. A discectomy is then performed and a Cobb elevator is passed along the vertebral endplates to release the annulus fibrosus. The implant is then sized and positioned to span the vertebral body and rest on the apophyseal ring. Fluoroscopy is utilized to confirm proper positioning and appropriate lordosis. Additional screws and plates may be placed depending on the patient to further secure the implant. Case images obtained via magnetic resonance imaging can be viewed in Figs. 1 and 2.
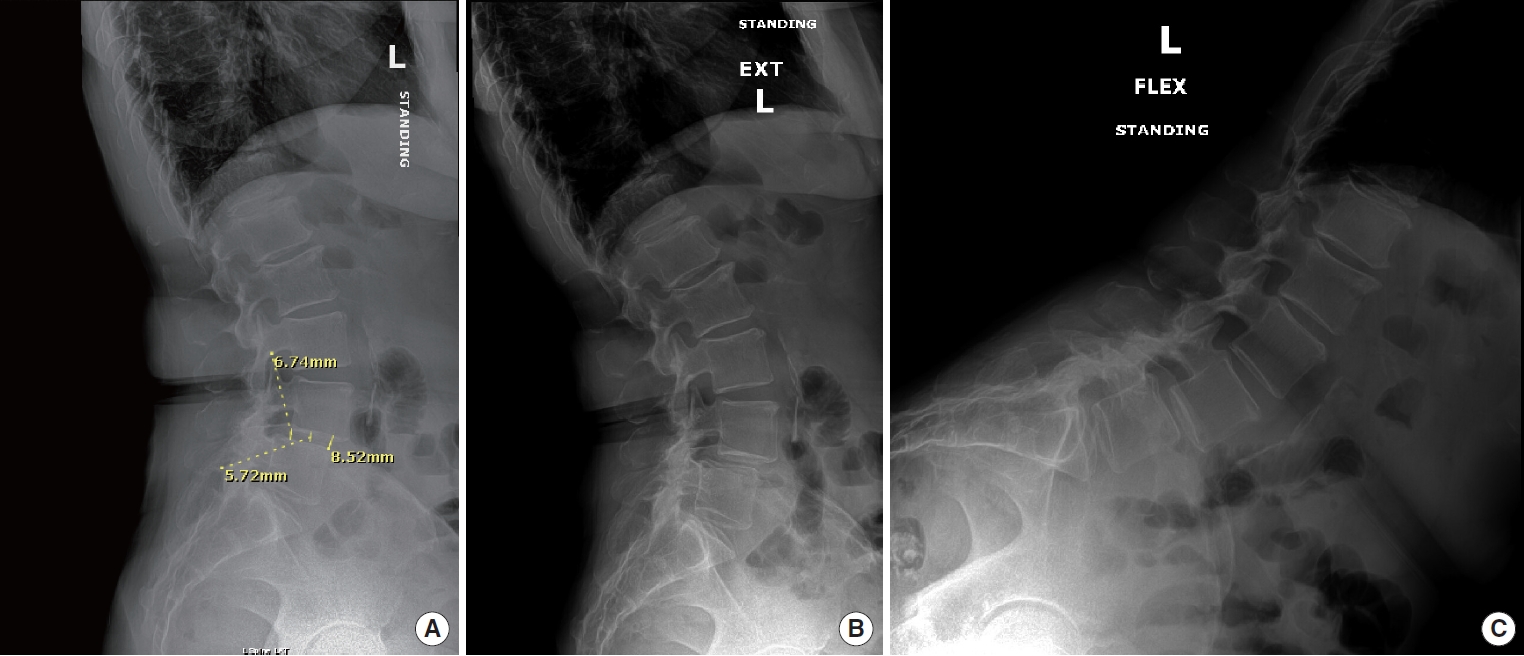
Preoperative lateral lumbar interbody fusion lumbosacral x-rays at L4–5. (A) Standing lateral view. (B) Lateral in extension. (C) Lateral in flexion.
2. Patient Population
A retrospective search of a prospectively maintained single orthopedic spine surgeon’s database was used to obtain patient data. Inclusion criteria consisted of patients who had undergone an elective LLIF. Patients were included if they had a VR-12 MCS preoperatively. Exclusion criteria consisted of patients with missing VR-12 MCS or patients with nonelective surgical indications such as acute trauma, infection, or neoplasms. Included patients underwent surgery between July 2014 and November 2022. All data for this current study were obtained with patient consent. Institutional Review Board approval was obtained prior to the start of this study (ORA #14051301).
3. Data Collection
Data consisting of demographics, perioperative characteristics, and PROMs were collected from the single-surgeon database. Demographic data included age, sex, body mass index (BMI), ethnicity, comorbidities (smoking, hypertension, and diabetes), American Society of Anesthesiologists (ASA) physical status classification, Charlson Comorbidity Index score, and insurance type.
Perioperative characteristics included number of fused levels, spinal pathology, operative time, estimated blood loss (mL), postoperative length of stay (hours), and postoperative day 0 (POD 0) patient measures. Spinal pathologies included degenerative spondylolisthesis, isthmic spondylolisthesis, recurrent herniated disc, central stenosis, and foraminal stenosis. POD 0 measures included patient-reported visual analogue scale (VAS) pain and narcotic consumption in oral morphine equivalents.
PROMs assessed included VR-12 MCS, VR-12 PCS, SF-12 MCS, SF-12 PCS, Patient-Reported Outcomes Measurement Information System physical function (PROMIS-PF), PHQ-9, VAS back pain (VAS-BP), VAS leg pain (VAS-LP), and Oswestry Disability Index (ODI). PROMs were obtained preoperatively, at 6 weeks postoperatively and at final follow-up. Mean time to final follow-up was 17.12± 8.43 months.
4. Statistical Analysis
Patients were placed into 2 cohorts: better mental health (VR12 MCS score≥ 50) and worse mental health (VR-12 MCS score < 50). Demographic and perioperative characteristics were compared using chi-square tests and independent samples t-tests for categorical and continuous variables, respectively. Independent samples t-tests were used to compare preoperative PROMs, postoperative PROMs, and ΔPROMs between groups. ΔPROMs were calculated by determining raw change in PROM scores from preoperative baseline to 6-week postoperative and final postoperative timepoints. The magnitude of score improvement for individual patients was used to determine achievement of minimal clinically important differences (MCIDs) through comparison to threshold values as found in previous spine literature. The MCID values used for this current study were as follows: VAS-BP: 1.8, VAS-LP: 2.4, ODI: 14.9, SF-12 MCS: 10.1, SF-12 PCS: 2.5, VR-12 MCS: 11.2, VR-12 PCS: 4.1, PROMIS-PF: 4.2, PHQ-9: 3.0 [13-17]. MCID achievement rates were compared between the 2 cohorts using chi-square tests. Bivariate Pearson correlation tests were used to calculate the degree of potential relationship between VR-12 and the other PROMs surveyed including VR-12 PCS, SF-12 MCS/PCS, PROMIS-PF, VAS-BP/LP, and ODI. All statistical analyses were performed using Stata 17.0 (StataCorp LP, College Station, TX). A p-value of < 0.05 was used to denote significance.
RESULTS
1. Descriptive Analyses
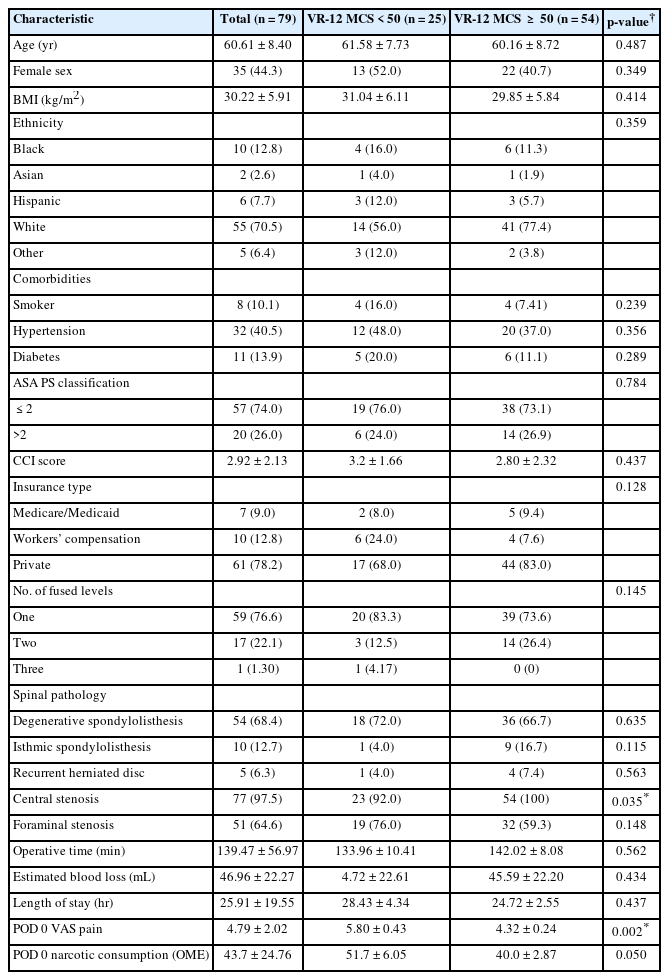
Seventy-nine patients met the inclusion criteria for this study, with 25 patients falling into the worse mental health cohort and 54 patients into the better mental health cohort. The mean age of the study population was 60.6 years and 44.3% self-identified as female. The mean BMI of the overall population was 30.2 kg/m2. A larger number of patients in the better mental health cohort were diagnosed with central stenosis and reported lower POD 0 VAS pain scores as compared to the MCS< 50 cohort. Other demographic and perioperative characteristics were statistically similar between both cohorts and can be referenced in Table 1.
2. Primary Outcome Measures
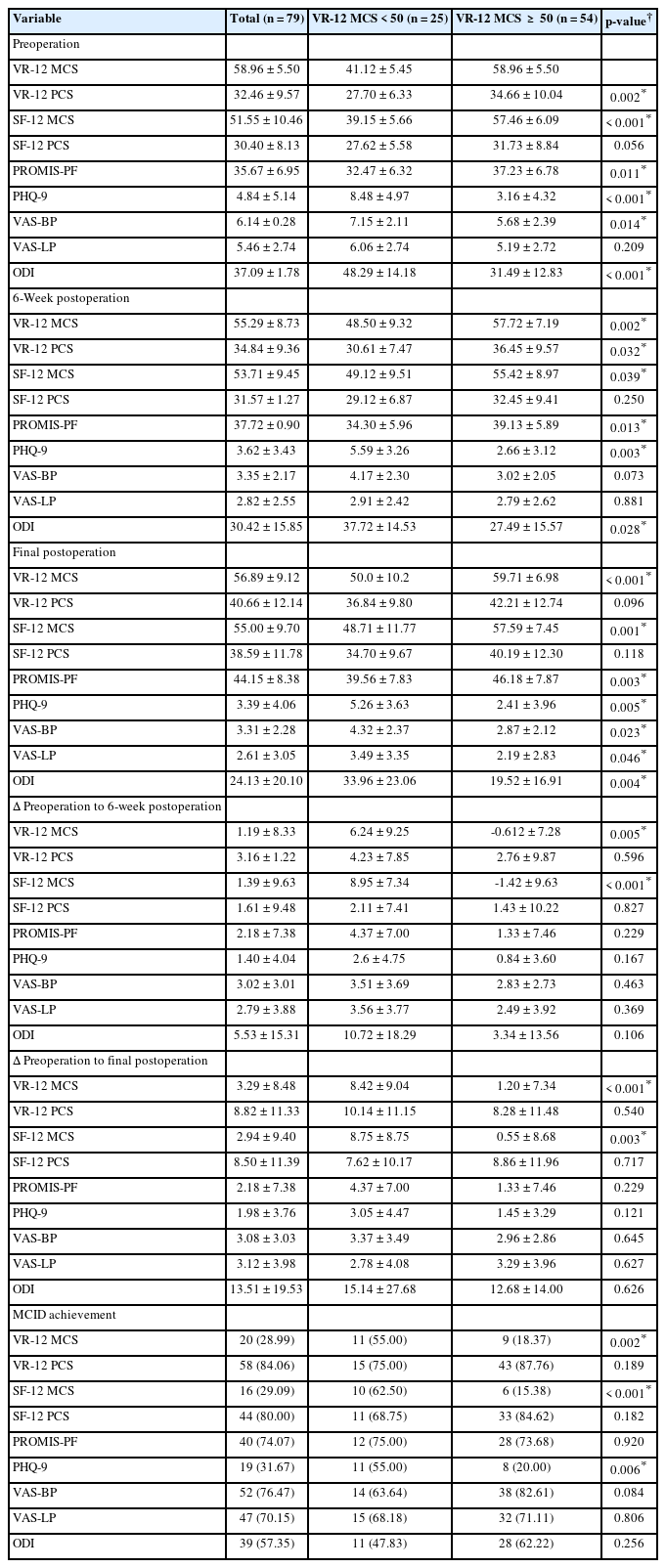
Patients in the better mental health cohort reported superior preoperative VR-12 PCS, SF-12 MCS, PROMIS-PF, PHQ-9, VAS-BP, and ODI scores (p≤ 0.014, all). At 6 weeks postoperatively, the better mental health cohort reported superior VR-12 MCS, VR-12 PCS, SF-12 MCS, PROMIS-PF, PHQ-9, and ODI scores (p≤ 0.039, all). This trend continued at the final follow-up, with the better mental health cohort reporting superior scores in VR-12 MCS, SF-12 MCS, PROMIS-PF, PHQ-9, VAS-BP, VAS-LP, and ODI (p≤ 0.046, all). From the preoperative baseline to the 6-week follow-up, the worse mental health cohort experienced a greater magnitude of improvement in VR-12 MCS and SF-12 MCS (p≤ 0.005, both) as compared to the better mental health cohort, which saw a decrease in scores. Furthermore, from preoperative baseline to the final follow-up, the worse mental health cohort again saw a greater magnitude of improvement in VR-12 MCS and SF-12 MCS (p ≤ 0.003, both). All other ΔPROM-6W and ΔPROM-FF demonstrated statistically similar improvements in both cohorts. MCID achievement rates for VR-12 MCS, SF-12 MCS, and PHQ-9 (p≤ 0.006, all) were higher in the worse mental health cohort. Further information on PROMs and MCID achievement can be found in Table 2.
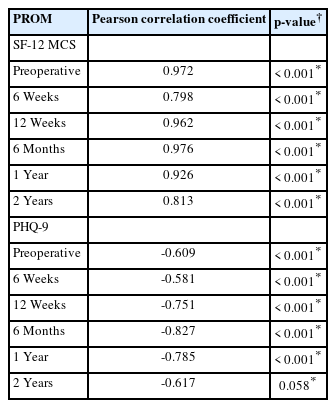
Data also showed a significant correlation between VR-12 MCS and all other assessed PROMs preoperatively (range, -0.626 to 0.972; p≤ 0.040, all). VR-12 MCS and the other mental health PROMs assessed (SF-12 MCS and PHQ-9) maintained a significant correlation throughout all follow-up periods up to 2 years postoperatively (range, -0.827 to 0.976; p< 0.001, all) except for PHQ-9 at 2 years postoperatively. VR-12 MCS also demonstrated a significant correlation with physical function, pain, and disability PROMs at several time points throughout the 2-year follow-up period. VR-12 MCS was significantly correlated with PROMIS-PF throughout all follow-up timepoints (range, 0.374–0.637; p≤ 0.019, all) and with ODI scores up to 1 year postoperatively (range, -0.626 to -0.292; p≤ 0.038, all). The VR-12 MCS scores were also intermittently significantly correlated with SF-12 PCS at 6 weeks and 6 months postoperatively (range, 0.333–0.692; p ≤ 0.021, both) and VR-12 PCS at 6 weeks, 12 weeks, 6 months, and 2 years postoperatively (range, 0.385–0.674; p≤ 0.039, all). The VR-12 MCS and VAS-B scores were significantly correlated from 6-week to 6-month (range, -0.779 to -0.287; p≤ 0.041, all) and VR-12 MCS and VAS-LP were intermittently significantly correlated at 12 weeks, 6 months, and 2 years postoperatively (range, -0.578 to -0.498; p≤ 0.001, all). Additional information on correlations can be referenced in Tables 3 and 4.
DISCUSSION
In this present study, we demonstrated the prognostic value of the VR-12 MCS for postoperative outcomes for patients undergoing LLIF. We found that patients with a VR-12 MCS< 50 (worse mental health) reported worse postoperative mental health, physical function, disability, and pain. Yet, this cohort reported similar improvement in PROMs and rates of MCID achievement in physical function, perceived pain, and disability. Interestingly, the worse mental health cohort reported a greater magnitude of improvement and higher rates of MCID achievement in postoperative mental health PROMs. Additionally, VR-12 MCS scores were found to be significantly correlated with all PROMs assessed preoperatively. There was also a significant correlation with other mental health PROMs postoperatively. The VR-12 MCS scores were also correlated with other PROMs assessed in domains such as physical function, pain, and disability, however, significance varied slightly based on PROM and time point assessed.
These results add to previous literature supporting worse preoperative mental health being associated with inferior surgical outcomes [4,9,18-21]. Much literature currently exists for the lower VR-12 MCS being correlated with diminished outcomes in other orthopedic surgeries such as joint arthroplasties [9,21,22]. However, few studies have examined specifically the correlation between VR-12 MCS and postoperative PROMs in lumbar spine surgery as in the present study.
In our study, the worse mental health cohort reported increased perceived pain on POD 0. Prior literature supports this finding with worse baseline mental health being identified as a serious comorbidity linked to increased postoperative pain [3,23-28]. Another study that followed patients for 2 years post lumbar surgery found that worse scores on the Beck Depression Inventory were correlated with inferior scores in VAS pain across the entire follow-up period [25]. Several systematic reviews also described the correlation between mental health issues and increased sensitivity to acute and chronic pain [18,29]. Thus, it may be beneficial to develop more effective perioperative pain management protocols, potentially including psychosocial interventions for use in patients with worse mental health.
Beyond worse perioperative pain, patients with worse mental health reported significantly worse postoperative PROMs in mental health, physical function, and perceived disability and pain. These results are supported by studies that demonstrated worse mental health being associated with inferior postoperative outcomes after both cervical and lumbar spine surgery, as demonstrated by poorer VAS-BP, ODI, and Neck Disability Index (NDI) scores [30,31]. One study found that patients with depression or anxiety reported inferior scores in PROMs such as NDI, VAS-neck pain, and SF-12 MCS after elective posterior cervical discectomy and fusion [23]. Studies also found that patients with worse baseline mental health continued to report inferior mental health scores and experienced more psychiatric complications postoperatively [19]. Similar findings have been reported regarding lumbar spinal surgery. One study found that postoperative mental health conditions can also lead to inferior postoperative outcomes in pain, physical function, and satisfaction with surgery after lumbar surgery [20]. Though prior literature has not utilized the VR-12 MCS as a prognostic indicator, it has been well-established that patients with worse baseline mental health continue to report inferior outcomes for mental health, physical function, perceived disability, and pain. These prior findings support those of the present study in which VR-12 MCS was used to determine baseline mental health.
Even with inferior postoperative PROMs, patients with worse mental health experienced greater improvement and higher rates of MCID achievement in mental health scores in our study. It is likely that patients with worse mental functioning have greater potential for improvement following surgery, and thus have higher MCID achievement rates. We noted similar magnitudes of improvement and MCID achievement rates in physical function, pain, and disability domains. Prior literature currently provides conflicting evidence for this trend. A study that followed patients for 5 years after MIS-TLIF found that the magnitude of improvements and MCID achievement for physical function, pain, and disability domains were similar regardless of mental health status, similar to the present findings [32]. In contrast, a prior study found that patients with better mental health were more likely to experience superior improvements in pain levels as identified via VAS pain scores after lumbar spine surgery [24]. Likewise, another study also reported evidence that patients with higher a MCS were more likely to achieve MCID in postoperative PROMs related to disability and surgical satisfaction [33]. These studies did not utilize the VR-12 questionnaire and had varied follow-up times, which could be possible explanations for these differences. Furthermore, as mental health is highly dynamic, it is possible that postoperative changes in mental health status confound the relationship between baseline mental health and postoperative outcomes. Future studies should aim to evaluate the continual influence of mental health throughout the postoperative period to address this possibility.
It has been demonstrated that VR-12 MCS scores are highly correlated with other legacy mental health PROMs such as SF-12 MCS, PROMIS mental health, EuroQoL-5 dimension (EQ-5D), and PHQ-9 scores in spine surgery establishing it as an accurate tool [10,12,34]. Moreover, there have also been several advantages identified in using the VR-12 MCS over other legacy PROMs. As compared to surveys such as the PHQ-9 which solely evaluate depressive symptoms, the VR-12 MCS surveys a broader picture of mental health by assessing both anxiety and depression, both of which are associated with inferior outcomes [23,35]. Furthermore, as compared to the EQ-5D, the VR-12 was able to better discriminate levels of comorbidity burden, allowing for a superior understanding of a patient’s true mental health status [10]. Additionally, the brevity of the VR-12 MCS mitigates survey fatigue, a well-documented phenomena which entails lower response rates and patients providing less accurate data if they are administered too many questionnaires [36].
The present findings suggest that VR-12 MCS is a useful prognostic tool for postoperative outcomes in patients undergoing elective LLIF. The superior PROMs of the better mental health cohort at 6 weeks postoperatively and at final follow-up show that a higher baseline VR-12 MCS is correlated with better surgical outcomes. Of note, even patients with lower preoperative VR-12 MCS still saw significant improvement and MCID achievement in all PROMs as compared to the other cohort, and even had a greater magnitude of improvement and higher rates of MCID achievement in mental health domains. Thus, our results show that patients with worse mental health measured by VR-12 MCS should not be excluded from consideration for surgery as they can still experience clinically significant improvement.
Several limitations do exist in this study. To measure primary outcomes, PROMs are utilized which are subject to recall and patient bias. Furthermore, the patient data was collected from a single-surgeon database. The demographic characteristics of the sample were relatively homogenous rendering the generalizability of these findings limited. Future studies should aim to analyze a more diverse patient population. To help mitigate these limitations, a larger multisurgeon and multisite database should be utilized for future studies. Additionally, it may be useful to have more uniform follow-up periods to better define the temporal limit to prognostic efficacy of the VR-12 MCS. As mental health may change postoperatively, assessing baseline mental health may not be sufficient to fully characterize its impact on outcomes. It is unknown how many patients had formal mental health diagnoses and were receiving treatment, introducing additional confounds.
CONCLUSION
Patients who underwent elective LLIF and had worse baseline VR-12 MCS were more likely to report inferior postoperative PROMs in mental health, physical function, and perceived disability and pain. VR-12 MCS and other mental health PROM scores also demonstrated a significant correlation throughout several time points. While both cohorts ultimately saw improvements in all baseline PROMs, the worse mental health cohort saw comparable magnitude of improvement and MCID achievement for physical health domains, and greater improvement and MCID achievement for mental health domains.
Notes
Conflict of Interest
The authors have nothing to disclose.
Funding/Support
This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contribution
Conceptualization: IK, FNA, AMR, VPF, GDL, AJS, KS; Data curation: IK, FNA, AMR, SSM, ACL, KRM, OOO, EZ, AK, JCW; Formal analysis: IK, FNA, AMR; Methodology: IK, FNA, AMR, VPF, GDL, AJS, KS; Project administration: SSM, ACL, KRM, OOO, EZ, AK, JCW, KS; Visualization: IK, FNA, AMR; Writing - original draft: IK, FNA, AMR; Writing - review & editing: IK, FNA, AMR, SSM, ACL, KRM, OOO, EZ, AK, JCW, VPF, GDL, AJS, KS.