1. James SL, Theadom A, Ellenbogen RG, et al. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019;18:56-87.


3. National Spinal Cord Injury Statistical Center. Spinal cord injury facts and figures at a glance. Birmingham (AL): University of Alabama at Birmingham; 2022.
4. DeJong G, Tian W, Hsieh CH, et al. Rehospitalization in the first year of traumatic spinal cord injury after discharge from medical rehabilitation. Arch Phys Med Rehabil 2013;94(4 Suppl 2):S87-97.


5. Bourassa-Moreau É, Mac-Thiong JM, Li A, et al. Do patients with complete spinal cord injury benefit from early surgical decompression? Analysis of neurological improvement in a prospective cohort study. J Neurotrauma 2016;33:301-6.


6. Badhiwala JH, Wilson JR, Witiw CD, et al. The influence of timing of surgical decompression for acute spinal cord injury: a pooled analysis of individual patient data. Lancet Neurol 2021;20:117-26.


7. Vale FL, Burns J, Jackson AB, et al. Combined medical and surgical treatment after acute spinal cord injury: results of a prospective pilot study to assess the merits of aggressive medical resuscitation and blood pressure management. J Neurosurg 1997;87:239-46.


9. Fehlings MG, Tetreault LA, Aarabi B, et al. A clinical practice guideline for the management of patients with acute spinal cord injury: recommendations on the type and timing of rehabilitation. Global Spine J 2017;7(3 Suppl):231S238S.
12. Goulet J, Richard-Denis A, Thompson C, et al. Relationships between specific functional abilities and health-related quality of life in chronic traumatic spinal cord injury. Am J Phys Med Rehabil 2019;98:14-9.


13. Tator CH, Fehlings MG. Review of the secondary injury theory of acute spinal cord trauma with emphasis on vascular mechanisms. J Neurosurg 1991;75:15-26.


14. Rowland JW, Hawryluk GW, Kwon B, et al. Current status of acute spinal cord injury pathophysiology and emerging therapies: promise on the horizon. Neurosurg Focus 2008;25:E2.

16. Kakulas BA. Pathology of spinal injuries. Cent Nerv Syst Trauma 1984;1:117-29.


17. Bunge RP, Puckett WR, Becerra JL, et al. Observations on the pathology of human spinal cord injury. A review and classification of 22 new cases with details from a case of chronic cord compression with extensive focal demyelination. Adv Neurol 1993;59:75-89.

18. Bunge RP, Puckett WR, Hiester ED. Observations on the pathology of several types of human spinal cord injury, with emphasis on the astrocyte response to penetrating injuries. Adv Neurol 1997;72:305-15.

19. Fehlings MG, Vaccaro AR, Boakye M. Essentials of spinal cord injury: basic research to clinical practice. New York: Thieme; 2012.
21. Waters RL, Adkins R, Yakura J, et al. Prediction of ambulatory performance based on motor scores derived from standards of the American Spinal Injury Association. Arch Phys Med Rehabil 1994;75:756-60.


22. Brown PJ, Marino RJ, Herbison GJ, et al. The 72-hour examination as a predictor of recovery in motor complete quadriplegia. Arch Phys Med Rehabil 1991;72:546-8.

24. Morrison SA, Lorenz D, Eskay CP, et al. Longitudinal recovery and reduced costs after 120 sessions of locomotor training for motor incomplete spinal cord injury. Arch Phys Med Rehabil 2018;99:555-62.


25. Popovich PG, Hickey WF. Bone marrow chimeric rats reveal the unique distribution of resident and recruited macrophages in the contused rat spinal cord. J Neuropathol Exp Neurol 2001;60:676-85.


26. Popovich PG, Wei P, Stokes BT. Cellular inflammatory response after spinal cord injury in Sprague-Dawley and Lewis rats. J Comp Neurol 1997;377:443-64.


31. Brennan FH, Hall JCE, Guan Z, et al. Microglia limit lesion expansion and promote functional recovery after spinal cord injury in mice. bioRxiv 2018;410258[Preprint]. 2018. Available from:
https://doi.org/10.1101/410258.

33. Carlson SL, Parrish ME, Springer JE, et al. Acute inflammatory response in spinal cord following impact injury. Exp Neurol 1998;151:77-88.


37. Pineau I, Sun L, Bastien D, et al. Astrocytes initiate inflammation in the injured mouse spinal cord by promoting the entry of neutrophils and inflammatory monocytes in an IL-1 receptor/MyD88-dependent fashion. Brain Behav Immun 2010;24:540-53.


38. Smith GM, Silver J. Transplantation of immature and mature astrocytes and their effect on scar formation in the lesioned central nervous system. Prog Brain Res 1988;78:353-61.

40. Snow DM, Lemmon V, Carrino DA, et al. Sulfated proteoglycans in astroglial barriers inhibit neurite outgrowth in vitro. Exp Neurol 1990;109:111-30.


42. McKeon RJ, Hoke A, Silver J. Injury-induced proteoglycans inhibit the potential for laminin-mediated axon growth on astrocytic scars. Exp Neurol 1995;136:32-43.


44. Monnier PP, Sierra A, Schwab JM, et al. The Rho/ROCK pathway mediates neurite growth-inhibitory activity associated with the chondroitin sulfate proteoglycans of the CNS glial scar. Mol Cell Neurosci 2003;22:319-30.


45. Chan CC, Wong AK, Liu J, et al. ROCK inhibition with Y27632 activates astrocytes and increases their expression of neurite growth-inhibitory chondroitin sulfate proteoglycans. Glia 2007;55:369-84.


47. Park E, Velumian AA, Fehlings MG. The role of excitotoxicity in secondary mechanisms of spinal cord injury: a review with an emphasis on the implications for white matter degeneration. J Neurotrauma 2004;21:754-74.


48. Liu D, Thangnipon W, McAdoo DJ. Excitatory amino acids rise to toxic levels upon impact injury to the rat spinal cord. Brain Res 1991;547:344-8.


50. McAdoo DJ, Xu GY, Robak G, et al. Changes in amino acid concentrations over time and space around an impact injury and their diffusion through the rat spinal cord. Exp Neurol 1999;159:538-44.


53. Grossman SD, Rosenberg LJ, Wrathall JR. Temporal-spatial pattern of acute neuronal and glial loss after spinal cord contusion. Exp Neurol 2001;168:273-82.


56. Baumann N, Pham-Dinh D. Biology of Oligodendrocyte and myelin in the mammalian central nervous system. Physiol Rev 2001;81:871-927.


61. Lytle JM, Vicini S, Wrathall JR. Phenotypic changes in NG2+ cells after spinal cord injury. J Neurotrauma 2006;23:1726-38.


62. Lytle JM, Wrathall JR. Glial cell loss, proliferation and replacement in the contused murine spinal cord. Eur J Neurosci 2007;25:1711-24.


63. Rabchevsky AG, Sullivan PG, Scheff SW. Temporal-spatial dynamics in oligodendrocyte and glial progenitor cell numbers throughout ventrolateral white matter following contusion spinal cord injury. Glia 2007;55:831-43.


64. Tripathi R, McTigue DM. Prominent oligodendrocyte genesis along the border of spinal contusion lesions. Glia 2007;55:698-711.


65. Goldstein EZ, Church JS, Hesp ZC, et al. A silver lining of neuroinflammation: Beneficial effects on myelination. Exp Neurol 2016;283:550-9.


67. Zai L, Wrathall JR. Cell proliferation and replacement following contusive spinal cord injury. Glia 2005;50:247-57.


73. Plemel JR, Keough MB, Duncan GJ, et al. Remyelination after spinal cord injury: is it a target for repair? Prog Neurobiol 2014;117:54-72.


74. Hill CE. A view from the ending: axonal dieback and regeneration following SCI. Neuroscience Letters 2017;652:11-24.


78. Coleman MP, Perry VH. Axon pathology in neurological disease: a neglected therapeutic target. Trends Neurosci 2002;25:532-7.


79. Fung EK, Loré JM Jr. Randomized controlled trials for evaluating surgical questions. Arch Otolaryngol Head Neck Surg 2002;128:631-4.


80. McDonald PJ, Kulkarni AV, Farrokhyar F, et al. Ethical issues in surgical research. Can J Surg 2010;53:133-6.


81. Chikuda H, Koyama Y, Matsubayashi Y, et al. Effect of early vs delayed surgical treatment on motor recovery in incomplete cervical spinal cord injury with preexisting cervical stenosis: a randomized clinical trial. JAMA Netw Open 2021;4:e2133604.


82. Morrison CA, Horwitz IB, Carrick MM. Ethical and legal issues in emergency research: barriers to conducting prospective randomized trials in an emergency setting. J Surg Res 2009;157:115-22.


84. Williamson TL, Cutler A, Cobb MI, et al. Autograft-derived spinal cord mass in the cervical spine following transplantation with olfactory mucosa cells for traumatic spinal cord injury: case report. J Neurosurg Spine 2020 Nov;1-5.
https://doi.org/10.3171/2020.6.SPINE20251. [Epub].


85. Freedman B. Equipoise and the ethics of clinical research. N Engl J Med 1987;317:141-5.


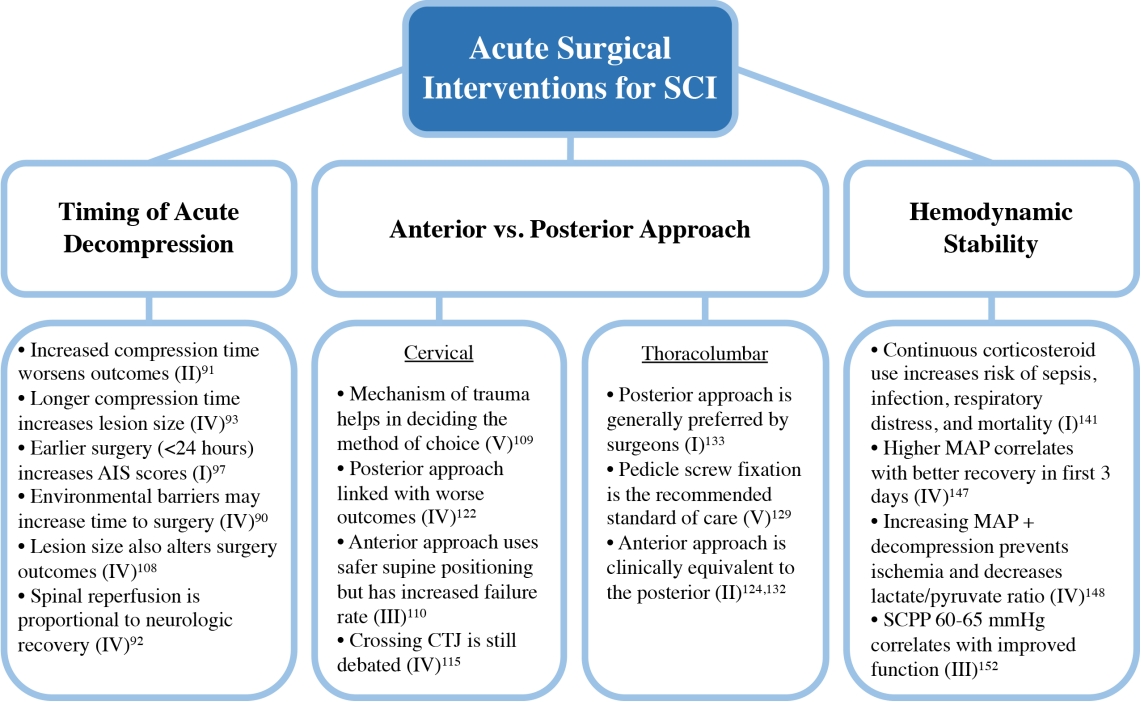
91. Dimar JR 2nd, Glassman SD, Raque GH, et al. The influence of spinal canal narrowing and timing of decompression on neurologic recovery after spinal cord contusion in a rat model. Spine (Phila Pa 1976) 1999;24:1623-33.


92. Carlson GD, Minato Y, Okada A, et al. Early time-dependent decompression for spinal cord injury: vascular mechanisms of recovery. J Neurotrauma 1997;14:951-62.


93. Carlson GD, Gorden CD, Oliff HS, et al. Sustained spinal cord compression: part I: time-dependent effect on longterm pathophysiology. J Bone Joint Surg Am 2003;85:86-94.

94. Vaccaro AR, Daugherty RJ, Sheehan TP, et al. Neurologic outcome of early versus late surgery for cervical spinal cord injury. Spine (Phila Pa 1976) 1997;22:2609-13.


95. Papadopoulos SM, Selden NR, Quint DJ, et al. Immediate spinal cord decompression for cervical spinal cord injury: feasibility and outcome. J Trauma 2002;52:323-32.


99. Sewell MD, Vachhani K, Alrawi A, et al. Results of early and late surgical decompression and stabilization for acute traumatic cervical spinal cord injury in patients with concomitant chest injuries. World Neurosurg 2018;118:e161-5.


100. Mattiassich G, Gollwitzer M, Gaderer F, et al. Functional outcomes in individuals undergoing very early (< 5h) and early (5-24h) surgical decompression in traumatic cervical spinal cord injury: analysis of neurological improvement from the austrian spinal cord injury study. J Neurotrauma 2017;34:3362-71.


101. Jug M, Kejžar N, Vesel M, et al. Neurological recovery after traumatic cervical spinal cord injury is superior if surgical decompression and instrumented fusion are performed within 8 hours versus 8 to 24 hours after injury: a single center experience. J Neurotrauma 2015;32:1385-92.


104. Chen L, Yang H, Yang T, et al. Effectiveness of surgical treatment for traumatic central cord syndrome. J Neurosurg Spine 2009;10:3-8.


105. Fehlings MG, Rabin D, Sears W, et al. Current practice in the timing of surgical intervention in spinal cord injury. Spine (Phila Pa 1976) 2010;35(21 Suppl):S166-73.


107. Tator CH, Fehlings MG, Thorpe K, et al. Current use and timing of spinal surgery for management of acute spinal surgery for management of acute spinal cord injury in North America: results of a retrospective multicenter study. J Neurosurg 1999;91:12-8.

108. Aarabi B, Akhtar-Danesh N, Chryssikos T, et al. Efficacy of ultra-early (< 12h), early (12-24h), and late (>24-138.5h) surgery with magnetic resonance imaging-confirmed decompression in American Spinal Injury Association Impairment Scale grades A, B, and C cervical spinal cord injury. J Neurotrauma 2020;37:448-57.


109. Dvorak MF, Fisher CG, Fehlings MG, et al. The surgical approach to subaxial cervical spine injuries: an evidencebased algorithm based on the SLIC classification system. Spine (Phila Pa 1976) 2007;32:2620-9.

110. Johnson MG, Fisher CG, Boyd M, et al. The radiographic failure of single segment anterior cervical plate fixation in traumatic cervical flexion distraction injuries. Spine (Phila Pa 1976) 2004;29:2815-20.


111. Reindl R, Ouellet J, Harvey EJ, et al. Anterior reduction for cervical spine dislocation. Spine (Phila Pa 1976) 2006;31:648-52.


112. Wang JC, Hart RA, Emery SE, et al. Graft migration or displacement after multilevel cervical corpectomy and strut grafting. Spine (Phila Pa 1976) 2003;28:1016-21. discussion 21-2.


114. Nagashima K, Koda M, Abe T, et al. Implant failure of pedicle screws in long-segment posterior cervical fusion is likely to occur at C7 and is avoidable by concomitant C6 or T1 buttress pedicle screws. J Clin Neurosci 2019;63:106-9.


115. Huang KT, Harary M, Abd-El-Barr MM, et al. Crossing the cervicothoracic junction in posterior cervical decompression and fusion: a cohort analysis. World Neurosurg 2019;131:e514-20.


118. Terao Y, Matsumoto S, Yamashita K, et al. Increased incidence of emergency airway management after combined anterior-posterior cervical spine surgery. J Neurosurg Anesthesiol 2004;16:282-6.


123. Verlaan JJ, Diekerhof CH, Buskens E, et al. Surgical treatment of traumatic fractures of the thoracic and lumbar spine: a systematic review of the literature on techniques, complications, and outcome. Spine (Phila Pa 1976) 2004;29:803-14.

124. Hao D, Wang W, Duan K, et al. Two-year follow-up evaluation of surgical treatment for thoracolumbar fracture-dislocation. Spine (Phila Pa 1976) 2014;39:E1284-90.


125. Wood KB, Li W, Lebl DR, et al. Management of thoracolumbar spine fractures. Spine J 2014;14:145-64.


129. Zeng J, Gong Q, Liu H, et al. Complete fracture-dislocation of the thoracolumbar spine without neurological deficit: a case report and review of the literature. Medicine (Baltimore) 2018;97:e0050.


130. Evans LJ. Thoracolumbar fracture with preservation of neurologic function. New Engl J Med 2012;367:1939.


132. Wang F, Zhu Y. Treatment of complete fracture-dislocation of thoracolumbar spine. J Spinal Disord Tech 2013;26:421-6.


133. Okuyama K, Abe E, Chiba M, et al. Outcome of anterior decompression and stabilization for thoracolumbar unstable burst fractures in the absence of neurologic deficits. Spine (Phila Pa 1976) 1996;21:620-5.


134. McDonough PW, Davis R, Tribus C, et al. The management of acute thoracolumbar burst fractures with anterior corpectomy and Z-plate fixation. Spine (Phila Pa 1976) 2004;29:1901-8. discussion 9.


135. Bracken MB, Shepard MJ, Collins WF Jr, et al. Methylprednisolone or naloxone treatment after acute spinal cord injury: 1-year follow-up data. Results of the second National Acute Spinal Cord Injury Study. J Neurosurg 1992;76:23-31.

136. Bracken MB, Shepard MJ, Collins WF, et al. A randomized, controlled trial of methylprednisolone or naloxone in the treatment of acute spinal-cord injury. Results of the Second National Acute Spinal Cord Injury Study. New Engl J Med 1990;322:1405-11.

137. Bracken MB, Shepard MJ, Holford TR, et al. Administration of methylprednisolone for 24 or 48 hours or tirilazad mesylate for 48 hours in the treatment of acute spinal cord injury. Results of the Third National Acute Spinal Cord Injury Randomized Controlled Trial. National Acute Spinal Cord Injury Study. JAMA 1997;277:1597-604.


138. Braughler JM, Hall ED. Correlation of methylprednisolone levels in cat spinal cord with its effects on (Na+ + K+)-ATPase, lipid peroxidation, and alpha motor neuron function. J Neurosurg 1982;56:838-44.


139. Braughler JM, Hall ED, Means ED, et al. Evaluation of an intensive methylprednisolone sodium succinate dosing regimen in experimental spinal cord injury. J Neurosurg 1987;67:102-5.


140. Young W. Blood flow, metabolic and neurophysiological mechanisms in spinal cord injury. In: Becker DP, Povlishock JTet al., editors. Central nervous system trauma status report. Rockville (MD): National Institutes of Health; 1985. p. 463-73.
144. Chu D, Qiu J, Grafe M, et al. Delayed cell death signaling in traumatized central nervous system: hypoxia. Neurochem Res 2002;27:97-106.

145. Walters BC, Hadley MN, Hurlbert RJ, et al. Guidelines for the management of acute cervical spine and spinal cord injuries: 2013 update. Neurosurgery 2013;60:82-91.

148. Kwon B. Optimizing hemodynamic support of acute spinal cord injury based on injury mechanism. Annual rept 30 Sep 2014 - 29 Sep 2015; Fort Belvoir, (VA), Defense Technical Information Center. 2015.
149. Werndle MC, Saadoun S, Phang I, et al. Monitoring of spinal cord perfusion pressure in acute spinal cord injury: initial findings of the injured spinal cord pressure evaluation study*. Crit Care Med 2014;42:646-55.

150. Saadoun S, Chen S, Papadopoulos MC. Intraspinal pressure and spinal cord perfusion pressure predict neurological outcome after traumatic spinal cord injury. J Neurol Neurosurg Psychiatry 2017;88:452-3.


151. Squair JW, Bélanger LM, Tsang A, et al. Empirical targets for acute hemodynamic management of individuals with spinal cord injury. Neurology 2019;93:e1205-e11.


152. Squair JW, Bélanger LM, Tsang A, et al. Spinal cord perfusion pressure predicts neurologic recovery in acute spinal cord injury. Neurology 2017;89:1660-7.


153. Coleman WP, Geisler FH. Injury severity as primary predictor of outcome in acute spinal cord injury: retrospective results from a large multicenter clinical trial. Spine J 2004;4:373-8.

155. Aarabi B, Hadley MN, Dhall SS, et al. Management of acute traumatic central cord syndrome (ATCCS). Neurosurgery 2013;72:195-204.


158. Visagan R, Hogg FRA, Gallagher MJ, et al. Monitoring spinal cord tissue oxygen in patients with acute, severe traumatic spinal cord injuries. Crit Care Med 2022;50:e477-86.