 |
 |
- Search
|
|
||
Abstract
Methods
Patients who underwent minimally invasive lumbar fusion for degenerative pathology using floor-mounted robot (ExcelsiusGPS) were included. Pedicle screw accuracy, proximal level violation rate, pedicle screw size, screw-related complications, and robot abandonment rate were analyzed.
Results
Two hundred twenty-nine patients were included. Most surgeries were primary single-level fusion. Sixty-five percent of surgeries had intraoperative computed tomography (CT) workflow, 35% had preoperative CT workflow. Sixty-six percent were transforaminal lumbar interbody fusion, 16% were lateral, 8% were anterior, and 10% were a combined approach. A total of 1,050 screws were placed with robotic assistance (85% in prone position, 15% in lateral position). Postoperative CT scan was available for 80 patients (419 screws). Overall pedicle screw accuracy rate was 96.4% (prone, 96.7%; lateral, 94.2%; primary, 96.7%; revision, 95.3%). Overall poor screw placement rate was 2.8% (prone, 2.7%; lateral, 3.8%; primary, 2.7%; revision, 3.5%). Overall proximal facet and endplate violation rates were 0.4% and 0.9%. Average diameter and length of pedicle screws were 7.1 mm and 47.7 mm. Screw revision had to be done for 1 screw (0.1%). Use of the robot had to be aborted in 2 cases (0.8%).
Conclusion
Usage of floor-mounted robotics for the placement of lumbar pedicle screws leads to excellent accuracy, large screw size, and negligible screw-related complications. It does so for screw placement in prone/lateral position and primary/revision surgery alike with negligible robot abandonment rates.
Given that anatomical landmarks are poorly visualized or palpated in minimally invasive spine surgery (MISS), both decompression and instrumentation heavily rely on intraoperative imaging [1,2]. Over the last 2 decades, there has been an evolution of newer navigation technologies in MISS with an intent to help reduce radiation exposure and increase pedicle screw accuracy [3-7].
The advent and application of robotic navigation in MISS in recent years has led to an improvement in pedicle screw accuracy, mainly because of planning of the screw trajectory and size and real-time visualization during placement [8,9]. The ability to plan the screw beforehand also allows placing screws with greater length and diameter, possibly increasing the stability of the construct. In addition, the robotic arm increases the reproducibility of screw placement by mitigating human error and decreasing surgeon fatigue as a result of favorable ergonomics. For lumbar interbody fusion surgeries, the utilization of the robot has gone beyond just pedicle screw placement to also assist with the identification of the disc space, disc preparation, and planning and placement of the interbody device using the navigational system of the robot [10].
Although studies have been conducted on the usage of robotic systems in MISS [11], literature regarding floor-mounted robots specifically requires more evidence to establish their utility. A floor-mounted robot does not attach to the bed or patient and hence, allows for easy in and out of the operating room (OR). Also, it better facilitates the placement of pedicle screws in the lateral position and sacral screws. The purpose of this study was to analyze the usage of a floor-mounted robotic system with integrated navigation capability and a rigid arm (ExcelsiusGPS, Globus Medical, Inc., Audubon, PA, USA) in minimally invasive lumbar spine fusion for degenerative lumbar pathology. This is the largest reported series in the literature of lumbar pedicle screw placement utilizing the ExcelsiusGPS robotic system. Our hypothesis was that the utilization of a floor-mounted robot leads to excellent accuracy of pedicle screw placement with negligible screw-related complications and robot abandonment rates.
This study was an Institutional Review Board (IRB)-approved retrospective review of prospectively collected data (Hospital for Special Surgery IRB approval number: 2018-1142) that was exempt from the informed consent requirement. Consecutive patients who underwent primary or revision minimally invasive lumbar fusion for degenerative lumbar pathology in the form of transforaminal lumbar interbody fusion (TLIF), lateral lumbar interbody fusion (LLIF), anterior lumbar interbody fusion (ALIF), or a combination of interbody fusion types (irrespective of the number of levels) (Qureshi-Louie class IIŌĆōV) [12] using ExcelsiusGPS robotic system (Globus Medical Inc., Audubon, PA, USA) between February 2019 and November 2021 were included. ExcelsiusGPS is a current-generation floor-mounted robot with a fully integrated navigation platform that allows for K-wireless placement of pedicle screws [13]. Indications of primary surgery included unstable/isthmic spondylolisthesis, up-down foraminal stenosis, degenerative scoliosis, and need for alignment/lordosis restoration. Indications for revision surgery included pseudarthrosis, adjacent segment disease, and failure of prior decompression. Surgeries included were all performed by 3 fellowship-trained spine surgeons with practices dedicated to MISS (experience with the robotic platform ŌĆō 3 years, 2 years, and 1 year, respectively) and the surgeonsŌĆÖ techniques did not change over the study course.
(1) Prone or lateral positioning of the patient on the Jackson table after induction of general anesthesia.
(2) Prepping and draping in a sterile fashion.
(3) Placement of the dynamic reference base (DRB) in the right posterior superior iliac spine (PSIS) with a small stab incision.
(4) Placement of a surveillance marker in the left PSIS with a stab incision.
(5) Attachment of a temporary intraoperative computed tomography (CT) fixture to the DRB.
(6) Three-dimensional (3D) fluoroscopic spin with Ziehm Vision RFD 3D (Ziehm Imaging, Inc., Orlando, FL, USA) (intraoperative CT workflow). In cases with preoperative CT workflow, this step was not needed and instead a preoperative CT scan was performed.
(7) Transfer of images to the ExcelsiusGPS robot.
(8) Intraoperative planning of pedicle screw and interbody placement.
(9) Registration of navigated instruments with the system.
(10) Utilization of a foot pedal by the surgeon to bring the robotic arm at the desired position.
(11) Placement of headless screws through the rigid end-effector under real-time visualization.
(12) Docking of the tubular retractor through a separate incision (posterior for TLIF, lateral for LLIF) using robotic navigation.
(13) Anteroposterior and lateral x-rays to confirm the positioning of screws and tube.
(14) TLIF or LLIF was performed as described previously in the literature [14-20]. Robotic navigation was utilized for disc preparation and interbody placement.
(15) Passage of rods under lateral fluoroscopy.
(16) X-rays to confirm good positioning of all hardware.
(17) For ALIF, the robot was used only for bilateral percutaneous pedicle screw placement in the prone position after anterior interbody placement was done with the patient supine.
Data was collected and managed using REDCap (Research Electronic Data Capture) [21,22] hosted at Weill Cornell Medicine Clinical and Translational Science Center supported by the National Center For Advancing Translational Science of the National Institute of Health under award number: UL1 TR002384. REDCap is a secure, HIPAA (Health Insurance Portability and Accountability Act)-compliant web-based software platform designed to support data capture and data management for research studies.
Patient demographics, including age, sex, body mass index (BMI), and American Society of Anesthesiologists (ASA) physical status classification were obtained from electronic medical records. Surgical data that were analyzed included type of surgery (primary/revision), type of fusion, and number of levels operated.
The outcome measures included: (1) pedicle screw accuracy, (2) proximal level facet and endplate violation rate, (3) pedicle screw size, (4) screw-related complications, and (5) robot abandonment rate. Pedicle screw accuracy was assessed separately for placement in prone/lateral positions and primary/revision surgeries according to the CT-based Gertzbein-Robbins Scale which grades screws depending on the extent of pedicle cortical breach (grade A: 0 mm, grade B: < 2 mm, grade C: < 4 mm, grade D: < 6 mm, grade E: > 6 mm) [23]. Grade A and B screws were deemed as accurate and grade C, D, and E screws as inaccurate [24,25]. The screws were also assessed according to the Simplified Screw Grading System (good: no pedicle, tip, facet, or endplate breach; acceptable: pedicle breach within the radiographic safe zone, ant distance of tip breach; poor: any breach outside of the radiographic safe zone i.e. Ōēź 4 mm of superior/lateral breach or Ōēź 2 mm of inferior/medial breach or violating the facet/endplate affecting the superior unfused level) [26,27]. CT scans were performed at 1-year postsurgery (as part of standard of care to assess fusion) and were evaluated for pedicle screw placement by 3 independent reviewers, an orthopedic spine fellow, and 2 orthopedic surgery residents. Operative time, recorded as time of incision to time of closure, was assessed for 1-level TLIF, LLIF, and ALIF which included insertion of pedicle screws with robotic assistance.
For descriptive analysis, categorical variables were summarized as ŌĆ£number (percentage),ŌĆØ normally and nonnormally distributed continuous variables were summarized as ŌĆ£mean┬▒ standard deviationŌĆØ and ŌĆ£median (interquartile range)ŌĆØ respectively. All analyses were performed using IBM SPSS Statistics ver. 22.0 (IBM Co., Armonk, NY, USA).
Two hundred twenty-nine patients were included. The mean age was 61 years and the mean BMI was 28.4 kg/m2. Eightythree percent of patients were ASA physical status classification grade II. Most surgeries were primary single-level fusion. Sixtysix percent were TLIF, 16% were LLIF, 8% were ALIF, and 10% were a combination of interbody fusion types. A total of 1,050 pedicle screws were placed with robotic assistance (85% in prone position, 15% in lateral position). Sixty-five percent of surgeries had the intraoperative CT workflow and 35% had the preoperative CT workflow. The average time for 1-level TLIF, LLIF, and ALIF including insertion of robotic screws were 104, 119, and 154 minutes, respectively (Table 1).
Postoperative CT scan was available for 80 patients (419 screws). The overall pedicle screw accuracy rate was 96.4% (screws placed in prone position: 96.7%; screws placed in lateral position: 94.2%; primary surgery: 96.7%; revision surgery: 95.3%). The overall poor screw placement rate was 2.8% (screws placed in prone position: 2.7%; screws placed in lateral position: 3.8%; primary surgery: 2.7%; revision surgery: 3.5%). The overall proximal facet and proximal endplate violation rates were 0.4% and 0.9%, respectively. These findings are detailed in Tables 2 and 3.
The average diameter and length of pedicle screws were 7.1 mm and 47.7 mm, respectively. > 50% screws had a diameter of Ōēź 7.5 mm and length of Ōēź 50 mm (Table 4). Return to the OR for screw revision had to be done for 1 screw (0.1%) placed in the prone position (L5 pedicle grade B inferior breach leading to neurological deficit). There was no major wound-related complication in any case. The use of the robot had to be aborted in 2 cases (0.8%) (array was bumped in one, calibration error in the other).
The ExcelsiusGPS robot was approved by the U.S. Food and Drug Administration in 2017. Its advantages over previously described robotic systems include K-wireless screw placement due to the rigidity of the external arm, detection of an offset > 1 mm by the surveillance marker and skiving forces by the sensor in the end-effector, fully integrated navigation capability, and portability [13]. Studies conducted on the use of ExcelsiusGPS robotic system in spine surgery and their findings are summarized in Table 5 [28-36]. The current study aimed to assess the utilization of this floor-mounted robotic system in the placement of pedicle screws in the prone/lateral position and in primary/revision surgery. It also analyzed the rates of screw-related complications and robot abandonment.
A floor-mounted robot has several advantages over a tablemounted robot in spine surgery. It is portable and can be shifted or moved during the surgery. It provides a more open and wider working field to the surgeon and may improve ergonomics. It better facilitates single-position surgery in the lateral position and insertion of sacral screws. One of its drawbacks is that it has a greater working distance compared to a table-mounted robot and this may lead to less accuracy in pedicle screw insertion. However, the findings of this study show that floor-mounted robotic screw insertion has excellent accuracy and negligible screw-related complications.
Pedicle screw placement using the conventional freehand and 2-dimensional fluoroscopy techniques has been reported to have comparatively higher rates of misplacement, which can in turn lead to neurovascular injury, chronic low back pain, and decreased pullout strength [37-39]. Two recent meta-analyses comparing robot-assisted versus freehand or fluoroscopy-based pedicle screw placement showed superior accuracy with robotic assistance [40,41]. Roser et al. [42] demonstrated higher accuracy for robotic versus navigated screw placement (99% vs. 92%). Previous studies conducted on pedicle screw placement using ExcelsiusGPS robot demonstrated an accuracy ranging from 96.6% to 100% and zero screw-related intraoperative or postoperative complications [28-36]. (Table 5). The current study, including screws placement both in prone and lateral positions and in primary and revision surgeries, showed similar findings with an overall pedicle screw accuracy of 96.4%, poor screw placement rate of 2.8%, and a single incident (0.1%) of screw-related complication that required a return to the OR for screw revision. One of the major issues that can compromise the accuracy of robotic screws is skiving. It can be reduced if the drill is started off of the bone and then advanced into the vertebral body until a point just beyond the end of the pedicle [43]. In addition, the ExcelsiusGPS robotic platform has a unique sensor to detect excessive lateral force [13].
LLIF often requires the addition of a pedicle screw construct to provide stability. Traditionally, it involves an intraoperative flip to the prone position following the lateral surgery, which, in turn, increases the operative time. Lately, the concept of singleposition surgery has gained traction where screws are put in the lateral position without needing a flip. Robotics has been the main driver behind this as it enables placing screws in ergonomically difficult and unfamiliar positions (especially the down-sided screws) by providing a defined trajectory through the rigid arm [44,45]. Huntsman et al. [34], using the ExcelsiusGPS robotic system, had reported a high pedicle accuracy rate of 98% with no screw-related complications in their study of 55 patients who had undergone single-position LLIF surgery. The current study had similar findings of high pedicle screw accuracy (94.2%), low poor screw placement rate (3.8%), and no screw-related complication.
Placement of pedicle screws in revision surgeries can be challenging due to altered anatomy and existing instrumentation. Ando et al. [46] had found a high rate of pedicle breaches when placing freehand pedicle screws in revision surgeries and concluded that due to a high potential for malposition, these screws should be placed carefully. Bederman et al. [47], on the other hand, found a high accuracy of pedicle screws in revision surgeries when using robotic guidance and concluded that it can benefit surgeons in navigating altered bony anatomy. The current study demonstrated a high pedicle screw accuracy (95.3%), low poor screw placement rate (3.5%), and no screw-related complications in revision surgeries.
Proximal unfused level violation can lead to adjacent segment disease compromising long-term clinical outcomes [26,48-50]. The robot allows planning of the screw trajectory and hence, prevents violation of the superior facet joint or endplate at the upper instrumented level. Zhang et al. [51] found that, compared to the freehand technique, robot-guided spinal surgery had significantly less facet joint violations (5.8% vs. 27.3%) and larger screw-facet distance (4.16 mm vs. 1.92 mm). Two meta-analyses also demonstrated decreased proximal facet joint violation with robotic assistance [41,52]. Using ExcelsiusGPS, Wallace et al. [30] reported no evidence of superior facet joint violation in any case. In the current study, 6 screws (1.3%) had affected the proximal unfused level by violating the facet (2 screws, 0.4%) or the endplate (4 screws, 0.9%).
Although the stability of the pedicle screw construct is largely dependent on the bone quality of the patient, screw size is also an important contributing factor. Previous studies have shown an increase in fixation strength with increasing screw diameter and length [53]. Shafi et al. [27], in their comparative study of robotics and navigation, found that robotic assistance allows for placement of pedicle screws with greater diameter and length, with similarly high accuracy. The current study found that the pedicle screws had an average diameter of 7.1 mm and an average length of 47.7 mm, with > 50% of screws having a diameter of Ōēź 7.5 mm and length of Ōēź 50 mm.
Although robotic platforms in spine surgery have been previously associated with increasing time demand, these studies do not seem to be completely reliable because of drawbacks like inconsistent definition of operative time and use of older robotic systems. The findings of this study showed that the average time for 1-level TLIF, LLIF, and ALIF including insertion of robotic screws were 104, 119, and 154 minutes, respectively. Our previously published papers demonstrated operative times of 112, 103, and 93 minutes with fluoroscopy, robotics, and navigation, respectively, for 1-level TLIF [3,6]. There was no significant difference in the total OR time between robotics and navigation. This shows that robotics does not increase the operative time demand compared to conventional spine surgery techniques. Each surgeon goes through a learning curve when adopting a new technology and we believe that once the learning curve is over, robotics actually leads to a more efficient operative workflow than traditional techniques.
The limitations of this study include its retrospective design, lack of a control group, and unavailability of the postoperative CT scans for pedicle screw assessment for > 50% of patients. The learning curve of the surgeons with robotics was unaccounted for. The results were not stratified by intraoperative/preoperative CT workflow or surgeon experience with the robotic platform. Three of the included patients had Ōēź 5 levels of fusion and included thoracic pedicle screws that may have led to heterogeneity of the dataset. For assessing screw size, stratified analysis was not done according to specific levels. In terms of the operative time demand, we did not have the data separately for screw insertion and interbody procedure or the data for time per screw. Hence, only the overall time from incision to closure (operative time) could be calculated. Comparative studies with larger sample sizes should be conducted to assess the outcomes and cost-effectiveness of robotics in MISS.
The use of current-generation floor-mounted robot for the placement of lumbar pedicle screws leads to excellent accuracy, large screw size, and negligible screw-related complications. It does so for screw placement in prone/lateral position and primary/revision surgery alike with negligible robot abandonment rates.
NOTES
Funding/Support
No direct funding was received for this study. However, the study used REDCap (Research Electronic Data Capture) hosted at Weill Cornell Medicine Clinical and Translational Science Center supported by the National Center For Advancing Translational Science of the National Institute of Health (NIH) under award number: UL1 TR002384.
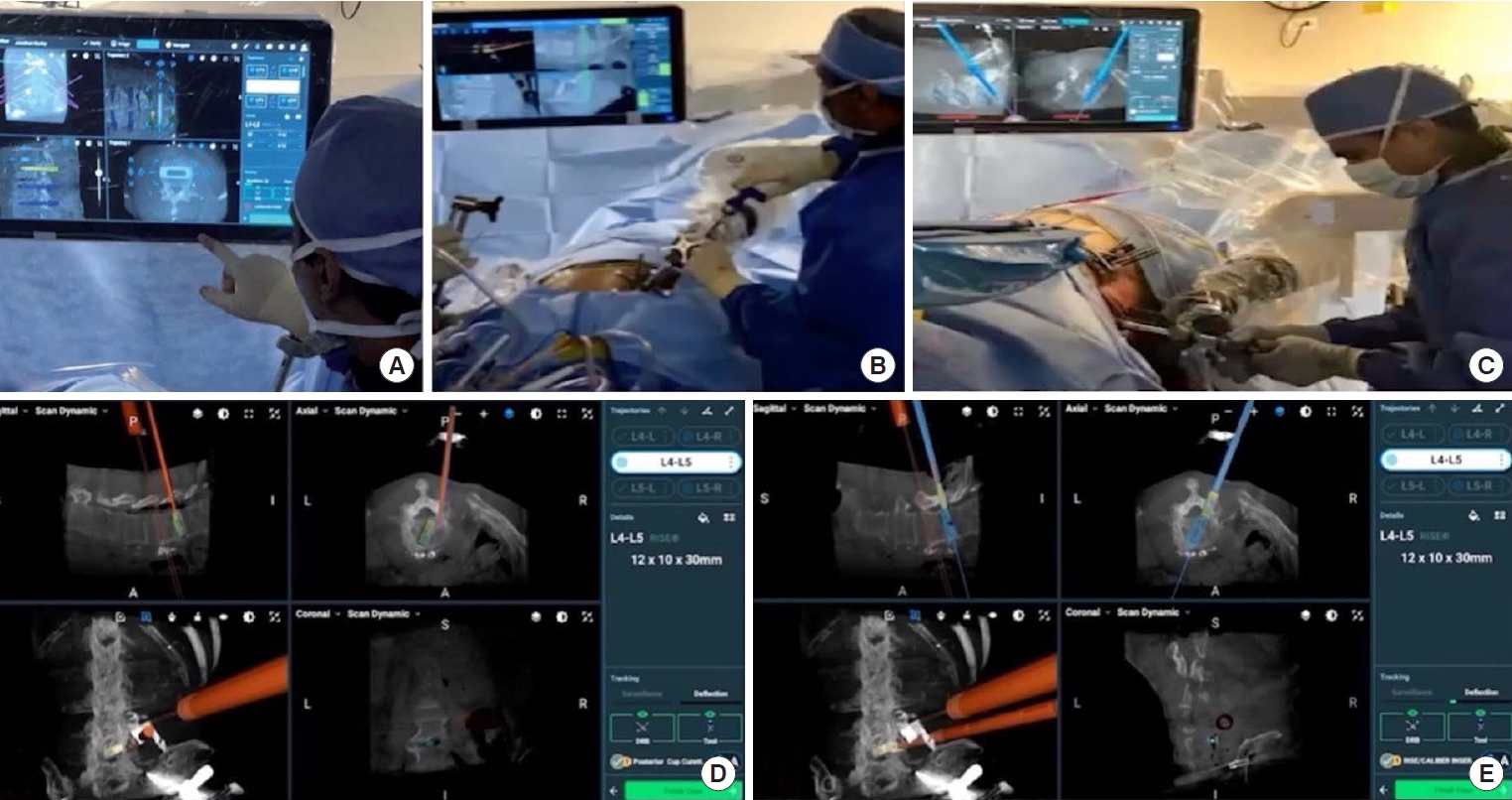
Fig.┬Ā1.
(A) Intraoperative planning of pedicle screws (trajectory, diameter, and length) and interbody placement. Pedicle screw placement through the rigid robotic arm with the patient in prone (B) or lateral (C) position. Disc preparation (D) and interbody placement (E) using robotic navigation.
Table┬Ā1.
Demographic and surgical data (n=229)
Table┬Ā2.
Assessment of pedicle screw placement in prone and lateral positions using robotics
Table┬Ā3.
Assessment of pedicle screw placement in primary and revision surgeries using robotics
Table┬Ā4.
Pedicle screw diameter and length
Table┬Ā5.
Studies conducted on ExcelsiusGPS-assisted spine surgery and their findings
| Study | Surgery type | No. of patients/pedicle screws | Pedicle screw accuracy | Screw-related complications | Robot abandonment |
|---|---|---|---|---|---|
| Jiang et al. [28] (2018) | Posterolateral fusion | 2/8 | 100% (8/8) | None | None |
| Jain et al. [29] (2019) | TLIF, ALIF, LLIF | 106/636 | 100% (66/66) | None | 5 |
| Wallace et al. [30] (2019) | Not specified | 106/600 | 98.2% (589/600) | None | 5 |
| Elswick et al. [31] (2019) | Not specified | 28/127 | 97.6% (122/125) | None | Not reported |
| Godzik et al. [32] (2019) | MI-TLIF, ALIF, LLIF | 28/116 | 96.6% (112/116) | None | 3 |
| Benech et al. [33] (2019) | Posterolateral fusion | 54/292 | 98.3% (287/292) | None | 1 |
| Huntsman et al. [34] (2020) | Single-position LLIF | 55/328 | Not studied | None | Not reported |
| Fayed et al. [35] (2020) | MI-TLIF, LLIF, ALIF | 20/103 | 98.1% (101/103) | None | 1 |
| Maalouly et al. [36] (2021) | Interbody fusion | 50/250 | 98% (245/250) | None | 2 |
| Current study | MI-TLIF, LLIF, ALIF, combination | 229/1050 | 96.4% (406/419) | 1 | 2 |
REFERENCES
1. Huang M, Tetreault TA, Vaishnav A, et al. The current state of navigation in robotic spine surgery. Ann Transl Med 2021;9:86.



2. Virk S, Qureshi S. Navigation in minimally invasive spine surgery. J Spine Surg 2019;5(Suppl 1):S25-30.



3. Shahi P, Vaishnav A, Araghi K, et al. Robotics reduces radiation exposure in minimally invasive lumbar fusion compared with navigation. Spine (Phila Pa 1976) 2022;47:1279-86.


4. Vaishnav AS, Othman YA, Virk SS, et al. Current state of minimally invasive spine surgery. J Spine Surg 2019;5(Suppl 1):S2-10.



5. Qureshi S, Lu Y, McAnany S, et al. Three-dimensional intraoperative imaging modalities in orthopaedic surgery: a narrative review. J Am Acad Orthop Surg 2014;22:800-9.

6. Vaishnav AS, Gang CH, Qureshi SA. Time-demand, radiation exposure and outcomes of minimally invasive spine surgery with the use of skin-anchored intraoperative navigation: the effect of the learning curve. Clin Spine Surg 2022;35:E111-20.

7. Tian W, Fan M, Zeng C, et al. Telerobotic spinal surgery based on 5G network: the first 12 cases. Neurospine 2020;17:114-20.




8. Avrumova F, Sivaganesan A, Alluri RK, et al. Workflow and efficiency of robotic-assisted navigation in spine surgery. HSS J 2021;17:302-7.




9. Good CR, Orosz LD, Lehman RA, et al. Minimally invasive posterior facet decortication and fusion using navigated robotic guidance: feasibility and workflow optimization. Neurospine 2022;19:773-9.




10. Alluri RK, Sivaganesan A, Vaishnav AS, et al. Robotic guided minimally invasive spine surgery. Perez-Cruet MMinimally invasive spine surgery - advances and innovations. London: IntechOpen; 2021.
11. Zhang Q, Han XG, Xu YF, et al. Robotic navigation during spine surgery. Expert Rev Med Devices 2020;17:27-32.


12. Louie PK, Vaishnav AS, Gang CH, et al. Development and initial internal validation of a novel classification system for perioperative expectations following minimally invasive degenerative lumbar spine surgery. Clin Spine Surg 2021;34:E537-44.


13. Alluri RK, Avrumova F, Sivaganesan A, et al. Overview of robotic technology in spine surgery. HSS J 2021;17:308-16.




14. Shahi P, Vaishnav AS, Mai E, et al. Practical answers to frequently asked questions in minimally invasive lumbar spine surgery. Spine J 2022 Jul 15:S1529-9430(22)00788-4. doi: 10.1016/j.spinee.2022.07.087. [Epub].

15. Shahi P, Vaishnav AS, Melissaridou D, et al. Factors causing delay in discharge in patients eligible for ambulatory lumbar fusion surgery. Spine (Phila Pa 1976) 2022;47:1137-44.


16. Shahi P, Dalal S, Shinn D, et al. Improvement following minimally invasive transforaminal lumbar interbody fusion in patients aged 70 years or older compared with younger age groups. Neurosurg Focus 2023;54:E4.

17. Fourman M, Alluri RK, Sarmiento JM, et al. Female sex and supine proximal lumbar lordosis are associated with the size of the LLIF safe zone at L4-5. Spine (Phila Pa 1976) 2022 Nov 14. doi: 10.1097/BRS.0000000000004541. [Epub].

18. Subramanian T, Araghi K, Sivaganesan A, et al. Ambulatory lumbar fusion: a systematic review of perioperative protocols, patient selection criteria, and outcomes. Spine (Phila Pa 1976) 2023 Feb 15;48(4):278-287. doi: 10.1097/BRS.0000000000004519. [Epub].
19. Shahi P, Shinn D, Singh N, et al. ODI <25 denotes patient acceptable symptom state after minimally invasive lumbar spine surgery. Spine (Phila Pa 1976) 2023;48:196-202.


20. Shinn D, Mok JK, Vaishnav AS, et al. Recovery kinetics after commonly performed minimally invasive spine surgery procedures. Spine (Phila Pa 1976) 2022 Jul 15. doi: 10.1097/BRS.0000000000004399. [Epub].

21. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377-81.


22. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 2019;95:103208.



23. Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine (Phila pa 1976) 1990;15:11-4.


24. Devito DP, Kaplan L, Dietl R, et al. Clinical acceptance and accuracy assessment of spinal implants guided with SpineAssist surgical robot: retrospective study. Spine (Phila pa 1976) 2010;35:2109-15.

25. van Dijk JD, van den Ende RP, Stramigioli S, et al. Clinical pedicle screw accuracy and deviation from planning in robot-guided spine surgery: robot-guided pedicle screw accuracy. Spine (Phila Pa 1976) 2015;40:E986-91.

26. Cong T, Sivaganesan A, Mikhail CM, et al. Facet violation with percutaneous pedicle screw placement: impact of 3D navigation and facet orientation. HSS J 2021;17:281-8.




27. Shafi KA, Pompeu YA, Vaishnav AS, et al. Does robot-assisted navigation influence pedicle screw selection and accuracy in minimally invasive spine surgery? Neurosurg Focus 2022;52:E4.

28. Jiang B, Karim Ahmed A, Zygourakis CC, et al. Pedicle screw accuracy assessment in ExcelsiusGPS® robotic spine surgery: evaluation of deviation from pre-planned trajectory. Chin Neurosurg J 2018;4:23.




29. Jain D, Manning J, Lord E, et al. Initial single-institution experience with a novel robotic-navigation system for thoracolumbar pedicle screw and pelvic screw placement with 643 screws. Int J Spine Surg 2019;13:459-63.



30. Wallace DJ, Vardiman AB, Booher GA, et al. Navigated robotic assistance improves pedicle screw accuracy in minimally invasive surgery of the lumbosacral spine: 600 pedicle screws in a single institution. Int J Med Robotics Comput Assist Surg 2020;16:e2054.


31. Elswick CM, Strong MJ, Joseph JR, et al. Robotic-assisted spinal surgery: current generation instrumentation and new applications. Neurosurg Clin N Am 2020;31:103-10.

32. Godzik J, Walker CT, Hartman C, et al. A quantitative assessment of the accuracy and reliability of robotically guided percutaneous pedicle screw placement: technique and application accuracy. Oper Neurosurg (Hagerstown) 2019;17:389-95.


33. Benech CA, Perez R, Benech F, et al. Navigated robotic assistance results in improved screw accuracy and positive clinical outcomes: an evaluation of the first 54 cases. J Robot Surg 2020;14:431-7.



34. Huntsman KT, Ahrendtsen LA, Riggleman JR, et al. Robotic-assisted navigated minimally invasive pedicle screw placement in the first 100 cases at a single institution. J Robotic Surg 2020;14:199-203.


35. Fayed I, Tai A, Triano M, et al. Robot-assisted percutaneous pedicle screw placement: evaluation of accuracy of the first 100 screws and comparison with cohort of fluoroscopy-guided screws. World Neurosurg 2020;143:e492-502.


36. Maalouly J, Sarkar M, Choi J. Retrospective study assessing the learning curve and the accuracy of minimally invasive robot-assisted pedicle screw placement during the first 41 robot-assisted spinal fusion surgeries. Mini-invasive Surg 2021;5:35.

37. Korkmaz M, Sariyilmaz K, Ozkunt O, et al. Quantitative comparison of a laterally misplaced pedicle screw with a redirected screw. How much pull-out strength is lost? Acta Orthop Traumatol Turcica 2018;52:459-63.

38. Gautschi OP, Schatlo B, Schaller K, et al. Clinically relevant complications related to pedicle screw placement in thoracolumbar surgery and their management: a literature review of 35,630 pedicle screws. Neurosurg Focus 2011;31:E8.

39. Baird EO, McAnany SJ, Overley S, et al. Accuracy of percutaneous pedicle screw placement: does training level matter? Clin Spine Surg 2017;30:E748-53.

40. Fan Y, Du JP, Liu JJ, et al. Accuracy of pedicle screw placement comparing robot-assisted technology and the free-hand with fluoroscopy-guided method in spine surgery: an updated meta-analysis. Medicine 2018;97:e10970.


41. Li HM, Zhang RJ, Shen CL. Accuracy of pedicle screw placement and clinical outcomes of robot-assisted technique versus conventional freehand technique in spine surgery from nine randomized controlled trials: a meta-analysis. Spine (Phila Pa 1976) 2020;45:E111-9.

42. Roser F, Tatagiba M, Maier G. Spinal robotics: current applications and future perspectives. Neurosurgery 2013;72 Suppl 1:12-8.

43. Sarmiento JM, Shahi P, Melissaridou D, et al. Step-by-step guide to robotic-guided minimally invasive transforaminal lumbar interbody fusion (MI-TLIF). Ann Transl Med 2023;11:221.


44. Dupont M, Shahi P, Qureshi S. Use of robotics in lateral surgery. Contemp Spine Surg 2022;23:1-5.

45. Pham MH, Diaz-Aguilar LD, Shah V, et al. Simultaneous robotic single position oblique lumbar interbody fusion with bilateral sacropelvic fixation in lateral decubitus. Neurospine 2021;18:406-12.




46. Ando K, Ishikawa Y, Kanemura T, et al. Accuracy of pedicle screw reinsertion in revision spine surgery. Clin Surg 2021;6:3230.
47. Bederman SS, Jain N, Woolwine S, et al. Accuracy of pedicle screw placement in revision spine surgery using robotic guidance. Global Spine J 2015;5(1_suppl):s-0035-1554210-s-0035-1554210.


48. Bagheri SR, Alimohammadi E, Froushani AZ, et al. Adjacent segment disease after posterior lumbar instrumentation surgery for degenerative disease: Incidence and risk factors. J Orthop Surg (Hong Kong) 2019;27:2309499019842378.



49. Wang H, Ma L, Yang D, et al. Incidence and risk factors of adjacent segment disease following posterior decompression and instrumented fusion for degenerative lumbar disorders. Medicine (Baltimore) 2017;96:E6032.



50. Sakaura H, Miwa T, Yamashita T, et al. Cortical bone trajectory screw fixation versus traditional pedicle screw fixation for 2-level posterior lumbar interbody fusion: comparison of surgical outcomes for 2-level degenerative lumbar spondylolisthesis. J Neurosurg Spine 2018;28:57-62.


51. Zhang Q, Xu YF, Tian W, et al. Comparison of superior-level facet joint violations between robot-assisted percutaneous pedicle screw placement and conventional open fluoroscopic-guided pedicle screw placement. Orthop Surg 2019;11:850-6.





- TOOLS
- Related articles in NS
-
Journal Impact Factor 3.2



























