1. Glassman SD, Berven S, Bridwell K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 2005;30:682-8.


3. Schwab F, Patel A, Ungar B, et al. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 2010;35:2224-31.

4. Bess S, Schwab F, Lafage V, et al. Classifications for adult spinal deformity and use of the Scoliosis Research Society-Schwab Adult Spinal Deformity Classification. Neurosurg Clin N Am 2013;24:185-93.


5. Terran J, Schwab F, Shaffrey CI, et al. The SRS-Schwab adult spinal deformity classification: assessment and clinical correlations based on a prospective operative and nonoperative cohort. Neurosurgery 2013;73:559-68.

6. Lee CS, Park JS, Nam Y, et al. Long-term benefits of appropriately corrected sagittal alignment in reconstructive surgery for adult spinal deformity: evaluation of clinical outcomes and mechanical failures. J Neurosurg Spine 2020;34:390-8.


9. Park SJ, Lee CS, Park JS, et al. Should thoracolumbar junction be always avoided as upper instrumented vertebra in long instrumented fusion for adult spinal deformity?: risk factor analysis for proximal junctional failure. Spine (Phila Pa 1976) 2020;45:686-93.

10. Lafage R, Schwab F, Challier V, et al. Defining spino-pelvic alignment thresholds: should operative goals in adult spinal deformity surgery account for age? Spine (Phila Pa 1976) 2016;41:62-8.

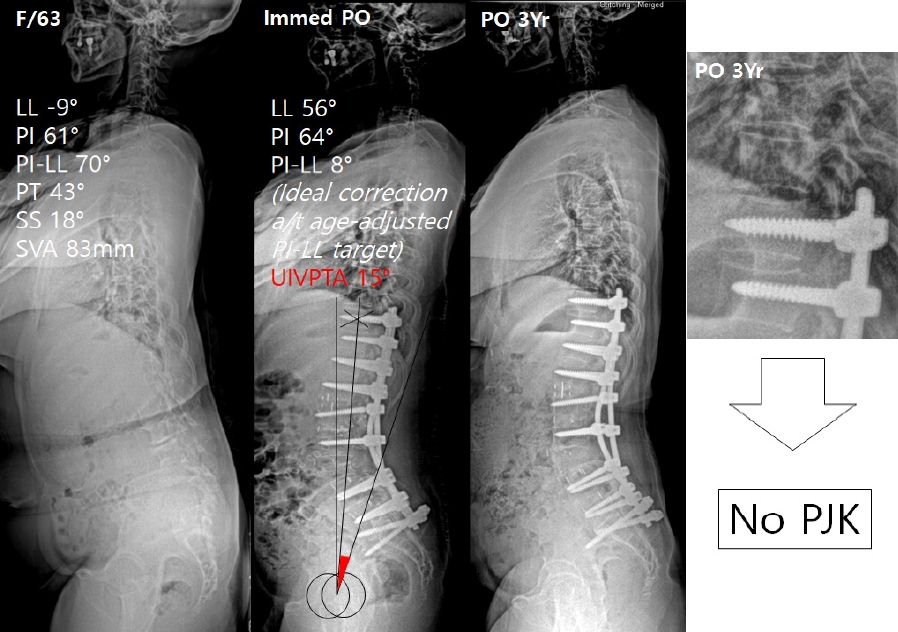
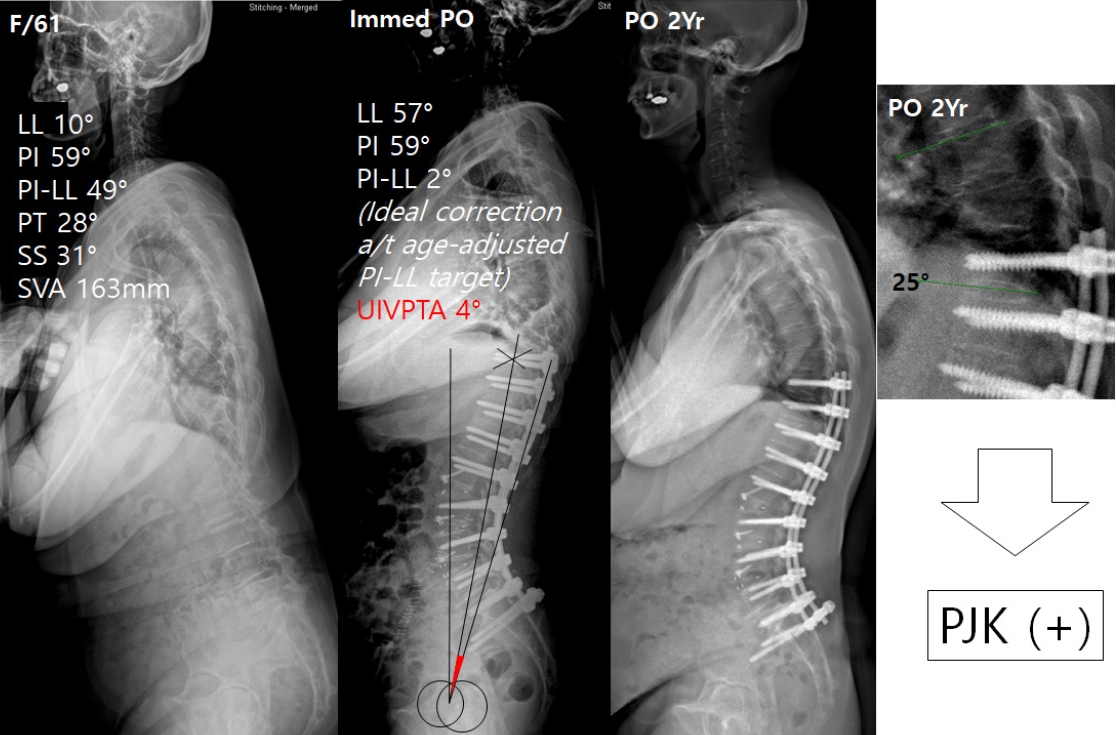
11. Byun CW, Cho JH, Lee CS, et al. Effect of overcorrection on proximal junctional kyphosis in adult spinal deformity: analysis by age-adjusted ideal sagittal alignment. Spine J 2022;22:635-45.


13. Lafage R, Schwab F, Glassman S, et al. Age-adjusted alignment goals have the potential to reduce PJK. Spine (Phila Pa 1976) 2017;42:1275-82.


14. Park SJ, Lee CS, Kang BJ, et al. Validation of age-adjusted ideal sagittal alignment in terms of proximal junctional failure and clinical outcomes in adult spinal deformity. Spine (Phila Pa 1976) 2022;47:1737-45.


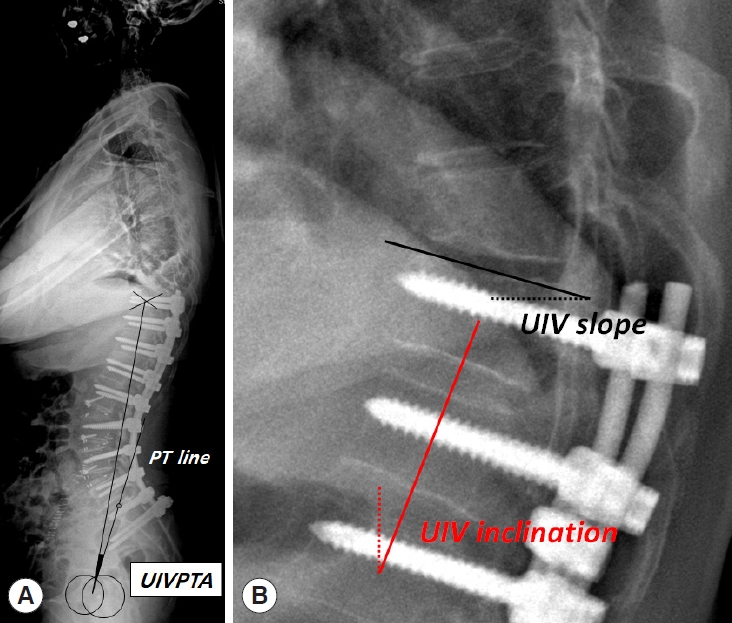
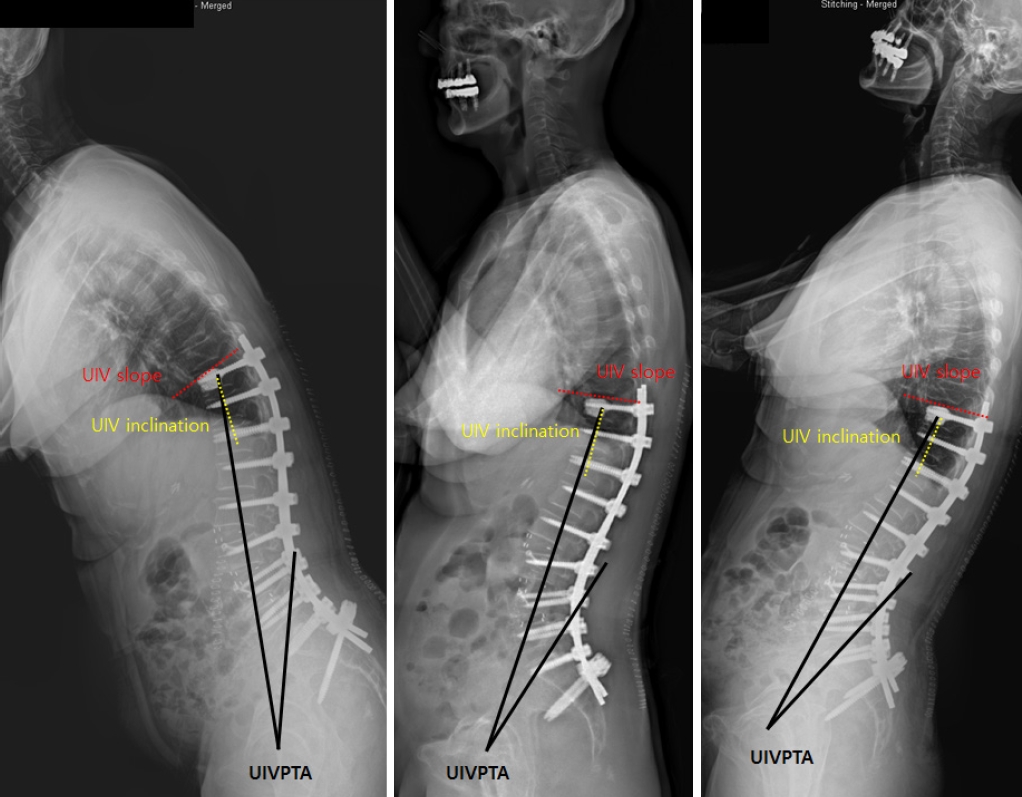
16. Lafage R, Line BG, Gupta S, et al. Orientation of the uppermost instrumented segment influences proximal junctional disease following adult spinal deformity surgery. Spine (Phila Pa 1976) 2017;42:1570-7.


18. Lee CS, Lee CK, Kim YT, et al. Dynamic sagittal imbalance of the spine in degenerative flat back: significance of pelvic tilt in surgical treatment. Spine (Phila Pa 1976) 2001;26:2029-35.

19. Takemitsu Y, Harada Y, Iwahara T, et al. Lumbar degenerative kyphosis. Clinical, radiological and epidemiological studies. Spine (Phila Pa 1976) 1988;13:1317-26.

20. Park JS, Lee CS, Choi YT, et al. Usefulness of anterior column release for segmental lordosis restoration in degenerative lumbar kyphosis. J Neurosurg Spine 2021;36:422-8.


21. Glattes RC, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adult spinal deformity following long instrumented posterior spinal fusion: incidence, outcomes, and risk factor analysis. Spine (Phila Pa 1976) 2005;30:1643-9.

22. Yilgor C, Sogunmez N, Boissiere L, et al. Global alignment and proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am 2017;99:1661-72.


24. Schwab F, Ungar B, Blondel B, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976) 2012;37:1077-82.

25. Jacobs E, van Royen BJ, van Kuijk SMJ, et al. Prediction of mechanical complications in adult spinal deformity surgery-the GAP score versus the Schwab classification. Spine J 2019;19:781-8.


30. Scheer JK, Lafage R, Schwab FJ, et al. Under correction of sagittal deformities based on age-adjusted alignment thresholds leads to worse health-related quality of life whereas over correction provides no additional benefit. Spine (Phila Pa 1976) 2018;43:388-93.


31. Yamato Y, Hasegawa T, Togawa D, et al. Rigorous correction of sagittal vertical axis is correlated with better ODI outcomes after extensive corrective fusion in elderly or extremely elderly patients with spinal deformity. Spine Deform 2019;7:610-8.


32. Pahys JM. T1 pelvic angle (TPA): another acronym to add to the pile, or the missing link for assessing sagittal plane alignment in adult spinal deformity? J Bone Joint Surg Am 2014;96:e172.


33. Fujimori T, Inoue S, Le H, et al. Long fusion from sacrum to thoracic spine for adult spinal deformity with sagittal imbalance: upper versus lower thoracic spine as site of upper instrumented vertebra. Neurosurg Focus 2014;36:E9.

34. Yagi M, Rahm M, Gaines R, et al. Characterization and surgical outcomes of proximal junctional failure in surgically treated patients with adult spinal deformity. Spine (Phila Pa 1976) 2014;39:E607-14.


35. Park SJ, Park JS, Nam YJ, et al. The long-term fate of asymptomatic proximal junctional kyphosis following long instrumented fusion in elderly patients with sagittal imbalance. Spine (Phila Pa 1976) 2021;46:E1097-104.


36. Park SJ, Park JS, Nam Y, et al. Who will require revision surgery among neurologically intact patients with proximal junctional failure after surgical correction of adult spinal deformity? Spine (Phila Pa 1976) 2021;46:520-9.


37. Raj A, Lee CS, Park JS, et al. Characteristics of patients undergoing revision surgery for proximal junctional failure after adult spinal deformity surgery: revalidation of the Hart-International Spine Study Group proximal junctional kyphosis severity scale. J Neurosurg Spine 2022 Mar 25:1-8. doi: 10.3171/2022.2.SPINE211387. [Epub].