|
 |
- Search
|
|
||
Abstract
Objective
Endoscopic spine surgery (ESS) is a minimally invasive approach with reduced tissue trauma, shorter hospital stays, and faster recovery times. It employs advanced endoscopic instruments and imaging technologies to address a wide range of spinal pathologies with minimal disruption to surrounding tissues. As ESS continues to evolve, this article aims to gather insights into the opinions and perspectives of the key stakeholders involved, and highlight strategies to improve implementation.
Methods
A cross-sectional survey was distributed to collect data on Australian spine surgeons’ perspectives of ESS. The survey questionnaire was distributed electronically to a diverse group of spine surgeons who are members of the Spine Society of Australia.
Results
Of responders, 46.8% were already integrating ESS into practice, or had the sufficient training to commence ESS. A further 29.8% were contemplating introduction of ESS techniques, while just under one quarter of respondents (23.4%) were not interested in implementing minimally invasive techniques. Primary motivators for implementation included skill development and improved patient outcomes. Primary barriers included lack of training opportunities, length of time to develop competency and lack of current supporting evidence.
Conclusion
The study contributes to the existing body of knowledge on ESS by providing a comprehensive analysis of surgeon opinions and experiences. The results highlight the growing interest in endoscopic techniques, while recognizing the challenges that need to be addressed to make this more widely utilised and available. The findings can guide future research, training programs, clinical practice and ultimately improve health and financial outcomes to patients and the wider health system.
Endoscopic spine surgery (ESS) has emerged as a minimally invasive alternative to traditional open spine surgery, offering potential benefits such as reduced tissue trauma, shorter hospital stays, and faster recovery times [1]. This innovative surgical technique employs endoscopic instruments and imaging technologies to address a wide range of spinal pathologies with minimal disruption to surrounding tissues. As the field of ESS continues to evolve it is crucial to gain insights into the opinions and perspectives of the key stakeholders involved, particularly the surgeons who perform these procedures. In doing so, we can be better prepared to implement strategies that assist in education and adoption of ESS.
Endoscopic approaches in Australia for Spinal pathologies have been documented in the literature over the last 20 years [2-5]. However, uptake of these various techniques has been slow. A survey was conducted to evaluate and discuss potential barriers.
This article aims to delve into the opinions of surgeons on ESS, shedding light on their experiences, challenges faced, and overall satisfaction with this minimally invasive approach. By exploring the attitudes of surgeons towards ESS, we can identify areas of success, ongoing concerns, and potential areas for improvement within this specialized field.
To accomplish this objective, a survey was designed and distributed to a diverse group of orthopaedic and neurosurgical spine surgeons. The questionnaire focused on various aspects of ESS, including indications for its use, approaches with use, technical challenges encountered, and overall likelihood to include this technique in future practice (Table 1).
Additionally, this paper will review existing literature on ESS, analysing relevant studies, clinical trials, and case reports to provide a comprehensive overview of the current state of knowledge. By combining the survey data with existing literature, we aim to present a comprehensive analysis of the collective opinions and experiences of surgeons regarding ESS.
The findings from this study will potentially have important implications for the future development and advancement of ESS in Australia.
In conclusion, this scientific paper seeks to contribute to the existing body of knowledge on ESS by providing an in-depth analysis of surgeon opinions and experiences. By elucidating the current attitudes towards this innovative technique, we hope to foster a deeper understanding of its strengths, limitations, and potential areas for growth. Ultimately, this research aims to enhance patient care and facilitate evidence-based decision-making for surgeons and healthcare providers involved in the management of spinal disorders.
This study employed a cross-sectional survey design to collect data on the opinions and perspectives of surgeons regarding ESS. The survey questionnaire was distributed electronically to members of the Spine Society of Australia (SSA).
Contact was made with the SSA and agreement that the questionnaire would be promulgated via email format to all members. There are currently 138 members of the SSA that the email and survey was circulated to.
A survey questionnaire was designed to capture information on various aspects and opinions of ESS. The questionnaire was developed based on a review of existing literature, expert opinions, and input from experienced endoscopic spine surgeons. The survey included both closed-ended and open-ended questions to allow for quantitative and qualitative data collection.
The survey questionnaire was distributed electronically using a secure online survey platform. Participants were provided with a unique survey link and were given a defined period to complete the questionnaire. Reminders were sent to non-respondents to maximize participation rates.
This study adhered to ethical guidelines from the South-Eastern Sydney Local Health District human research ethics committee. Participants were assured of confidentiality and informed consent was obtained prior to survey participation. Information collated was stored in a secure database.
It is important to acknowledge the potential limitations of this study. The survey-based design may introduce response biases, and the findings may not be generalizable to all surgeons and is likely to favour those already involved in or looking to implement ESS. Additionally, the study relied on self-reported data, which may be subject to recall bias.
A total of 48 spine surgeons participated in the study. The surgeons were geographically diverse, representing various regions throughout Australia. The total response rate was 48 of 138, 35% of the spine surgeons involved in SSA.
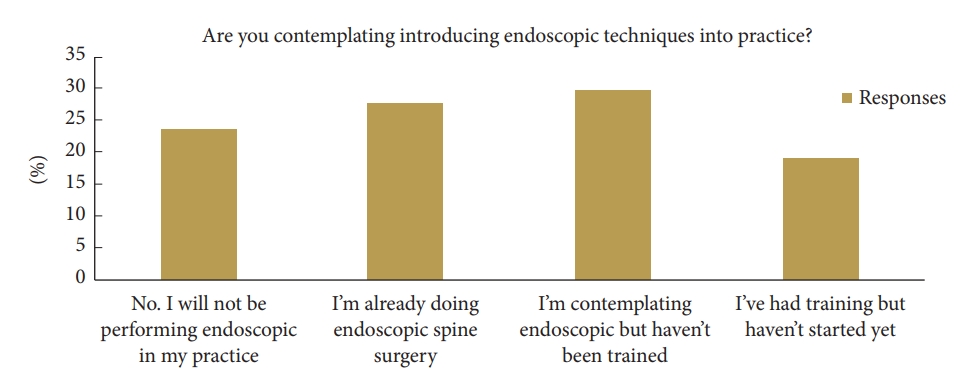
The participants reported a range of experience with ESS. Of the responders, 46.8% were either had the sufficient training to commence ESS or already integrating ESS into practice. A further 29.8% were contemplating introduction of ESS techniques, while just under one quarter of respondents (23.4%) were not interested in introducing minimally invasive techniques into practice (Fig. 1).
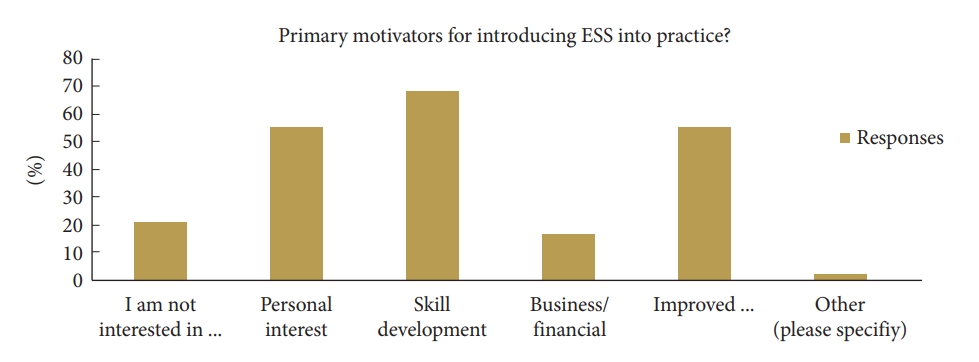
Primary motivators for introduction of ESS into surgical practice included wider skill development (68.1%), personal interest (55.3%), and improve patient recovery time and reduced length of stay (55.3%). Nearly one-fifth of responders noted business or financial means as a motivation to introduce minimally invasive techniques into practice (Fig. 2).
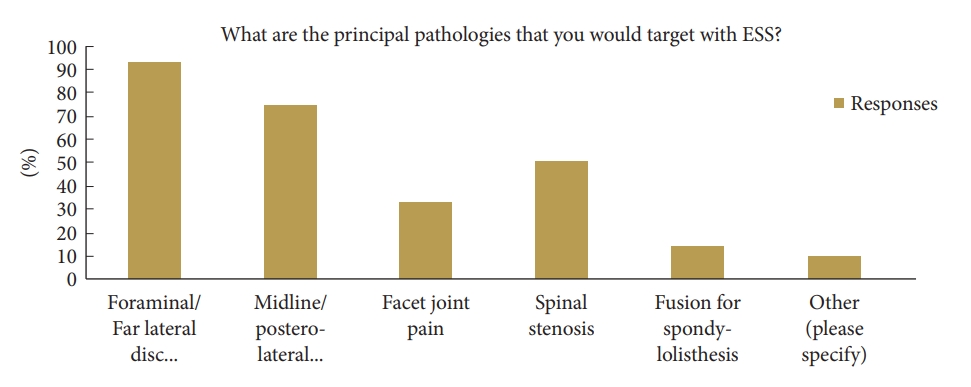
From the sampled participants, the primary pathologies thought to be favourable for ESS included foraminal and posterolateral/midline disc herniation (92.9% and 73.8% respectively). Other pathologies include facet joint pain, spinal stenosis, foraminotomy and fusion. Majority of respondents felt the most appropriate approaches to introduce to practice would be transforaminal and interlaminar. The majority felt they would utilise either uniportal or biportal endoscopic approaches (Fig. 3).
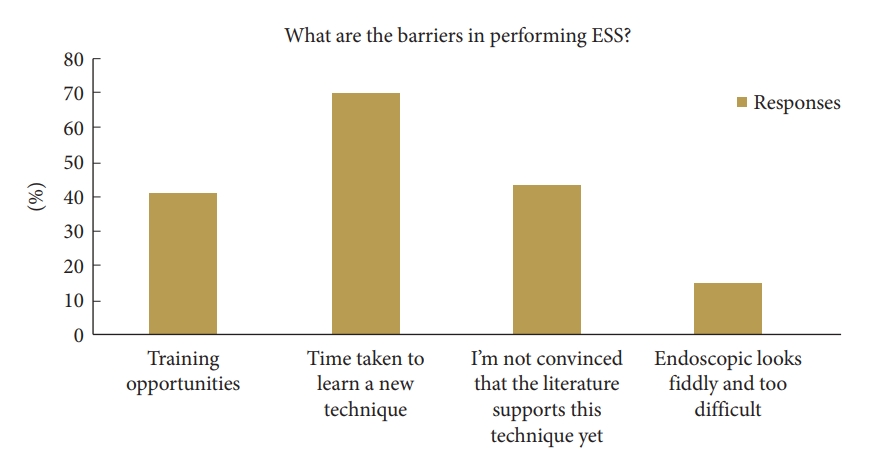
The primary barrier to implementation of ESS for most respondents was the perceived time taken to learn and master another surgical approach (69.6%) and the lack of training opportunities (41.3%). Other deterrents included lack of supporting evidence in medical literature and procedural difficulty with visualization and manoeuvrability (Fig. 4).
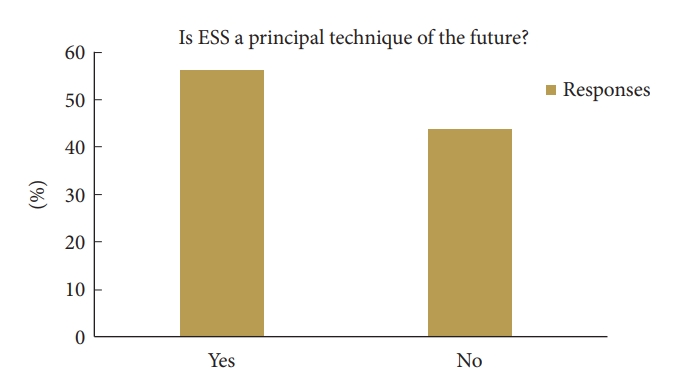
Overall, when questioned asked about the future of ESS, 56.3% of surgeons believed that the technique would continue to advance and become a standard procedure in spine surgery (Fig. 5).
The results of this study indicate that surgeons have positive opinions and experiences with ESS. It appears to be perceived as an effective and minimally invasive approach for treating certain spinal pathologies. However, challenges such as surgical technique with limited visualization and a challenging learning curve exist, highlighting the importance of formalised training and skill development. The results show promise for the future of ESS, envisioning further advancements and broader applications in the field of spine surgery.
This study provides valuable insights into the opinions and current familiarity of Australian surgeons regarding ESS as a practice for the future. The findings reveal that spinal surgeons perceive ESS as an effective and minimally invasive technique for the treatment a wide range of pathology.
Medical literature shows the first attempts of endoscopic lumbar spine surgery can be dated back as early as the 1980s [6], however it is only within the last decade that this approach is growing in prevalence, as a higher volume of spine surgeons become more familiar and experienced with the various techniques. This willingness to learn and master new techniques is a trait that is exhibited within the survey distributed and should further drive the development and availability of further training opportunities.
Developing techniques and research in ESS has been reviewed in the previous years as the technique is more widely explored and adopted. Research and early technique implementation are particularly concentrated within a small group of countries and authors. A bibliometric analysis highlighted that the vast majority of research into endoscopic spine techniques (over 50%) of these are published in and originated in China and South Korea [7].
The regions identified that demonstrated larger interest and publications within the field of endoscopic spine techniques also had noticeably higher rates of native surgeon training in ESS, as they go on to utilise and implement this in practice [8]. There were statistically significant differences in spinal endoscopy between Asian vs. non-Asian surgeons, further highlighting the willingness to learn and implement more progressive techniques. A beneficial notion identified within the article by Kim et al. [16] is that a formalised training program with an accredited curriculum or mentorship program, such as those seen in Asian regions, may lead to higher uptake, skill development and implementation of ESS in Australia.
Key areas of focus for endoscopic surgeons were identified in review of the literature, including patient selection, technical challenges, and postoperative outcomes [9,10]. Surgeons considered various factors when selecting patients for ESS, emphasizing the importance of appropriate case selection based on age, symptom severity, and imaging findings. Technical challenges such as limited visualization and instrument manoeuvrability were recognized, highlighting the need for ongoing training and skill development in endoscopic techniques. Complications encountered during ESS can be difficult to manage, given lack of exposure and visualization. This further emphasizes the importance of adequate training and skillset, in addition to the importance of understanding the advantages and disadvantages of ESS and ensuring to utilise the most appropriate approach for each individual presentation.
Based on the literature to date, positive postoperative outcomes reported by surgeons, including significant pain relief and improved functional outcomes, are encouraging [10]. Patient satisfaction rates were high, indicating the potential benefits of ESS in enhancing patient well-being and quality of life. Complication rates in experienced and well-trained endoscopic spine surgeons appear to be comparable to traditional discectomy and decompression procedures [11-14] within retrospective analyses, however the medical literature currently lacks high powered studies to further this.
The study participants expressed a positive outlook for the future of ESS, foreseeing continued advancements and broader applications in the field. This reflects the potential of endoscopic techniques to become routine in spine surgery, offering patients a less invasive alternative to traditional open surgery that produces less tissue trauma, minimal disruption of healthy soft tissues and shorter hospital stays with comparable adverse outcomes [15,16].
It is important to acknowledge the limitations of this study, including the potential for response bias and the reliance on self-reported data. Additionally, the findings may not be generalizable to all surgeons performing ESS due to the specific sample characteristics. In addition, the authors accept that the true rate of uptake of ESS in this cohort is likely significantly lower than reported in this study as surgeons who have contemplated, or performing ESS, are more likely to respond to the study questionnaire rather than surgeons disinterested in ESS. Despite this, the overall trend in addition to the progressive implementation of techniques within the wider spinal surgery community is promising and worth highlighting.
The review contributes to the existing body of knowledge on ESS by providing a comprehensive analysis of Australian spine surgeons opinions and experiences, in addition to highlighting the development of endoscopic techniques on a global scale. The article demonstrates the strengths of endoscopic techniques in terms of patient outcomes and surgeon perspectives, while also highlighting the challenges that need to be addressed before this practice can become more commonplace. The findings can guide future research, training programs, and clinical practice, ultimately leading to improved patient care and outcomes in the field of ESS. As surgical techniques become less invasive and surgeons become more proficient with endoscopic spine approaches, it is possible the future of spinal decompression and discectomy could be performed on a day-surgery basis; leading to improved patient satisfaction, reduced surgical wait times, reduced bed pressures and overall reduction in costs to the healthcare systems [17].
NOTES
Table 1.
Summary of survey and results
REFERENCES
1. Hasan S, Härtl R, Hofstetter CP. The benefit zone of full-endoscopic spine surgery. J Spine Surg 2019;5(Suppl 1):S41-56.



2. Mobbs RJ, Nakaji P, Szkandera BJ, et al. Endoscopic assisted posterior decompression for spinal neoplasms. J Clin Neurosci 2002;9:437-9.


4. Phan K, Xu J, Schultz K, et al. Full-endoscopic versus microendoscopic and open discectomy: a systematic review and meta-analysis of outcomes and complications. Clin Neurol Neurosurg 2017;154:1-12.


5. Rao PJ, Thayaparan GK, Fairhall JM, et al. Minimally invasive percutaneous fixation techniques for metastatic spinal disease. Orthop Surg 2014;6:187-95.



6. Mayer HM. A history of endoscopic lumbar spine surgery: what have we learnt? Biomed Res Int 2019;2019:4583943.




7. Lin GX, Zhu MT, Kotheeranurak V, et al. Current status and research hotspots in the field of full endoscopic spine surgery: a bibliometric analysis. Front Surg 2022;9:989513.



8. Kim JS, Yeung A, Lokanath YK, et al. Is Asia truly a hotspot of contemporary minimally invasive and endoscopic spinal surgery? J Spine Surg 2020;6(Suppl 1):S224-36.



9. Dowling Á, Lewandrowski KU, da Silva FHP, et al. Patient selection protocols for endoscopic transforaminal, interlaminar, and translaminar decompression of lumbar spinal stenosis. J Spine Surg 2020;6(Suppl 1):S120-32.



10. Wu C, Lee CY, Chen SC, et al. Functional outcomes of full-endoscopic spine surgery for high-grade migrated lumbar disc herniation: a prospective registry-based cohort study with more than 5years of follow-up. BMC Musculoskelet Disord 2021;22:58.




11. Silva JDS, Carelli LE, de Oliveira JAA, et al. Full-endoscopic discectomy for thoracic disc herniations: a single-arm meta-analysis of safety and efficacy outcomes. Eur Spine J 2023;32:1254-64.



12. Zhou C, Zhang G, Panchal RR, et al. Unique complications of percutaneous endoscopic lumbar discectomy and percutaneous endoscopic interlaminar discectomy. Pain Physician 2018;21:E105-12.

13. Tu Z, Li YW, Wang B, et al. Clinical outcome of full-endoscopic interlaminar discectomy for single-level lumbar disc herniation: a minimum of 5-year follow-up. Pain Physician 2017;20:E425-30.

14. Ruetten S, Komp M, Merk H, et al. Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: a prospective, randomized, controlled study. J Neurosurg Spine 2009;10:476-85.


15. Qin R, Liu B, Hao J, et al. Percutaneous endoscopic lumbar discectomy versus posterior open lumbar microdiscectomy for the treatment of symptomatic lumbar disc herniation: a systemic review and meta-analysis. World Neurosurg 2018;120:352-62.