 |
 |
- Search
|
|
||
Abstract
Objective
To compare the radiological outcomes in Lenke 5C type patients whose lowest instrumented vertebra (LIV) was L3 or L4 in a case-match study.
Methods
We conducted a retrospective case-match study and included 82 patients in the study. Radiological results before surgery, after surgery, and at last follow-up were recorded and analyzed in the L3 and L4 groups.
Results
After matching the age, RisserŌĆÖs sign, sex, and main Cobb, 41 pairs of patients were enrolled in our study. The total fusion segments in the L3 group (median [interquartile range]: 5.0 [6.0ŌĆō5.0]) were shorter than those in the L4 group (6.0 [6.5ŌĆō6.0]). The main curve was significantly corrected after surgery in both groups, and was comparable at the last follow-up between groups. In addition, according to the results of Fisher precision probability test, there was no significant difference of coronal or sagittal imbalance between the 2 groups at the 2-year follow-up.
Conclusion
The correction in coronal and sagittal planes in L3 group and L4 group remains similar. On account of more motion segments, L3 could be an ideal choice as LIV in moderate Lenke 5C type AIS. Long-term follow-up is needed to evaluate the effect of larger compensatory lumbar-sacral curve when stopping at L3.
The Lenke 5 type adolescent idiopathic scoliosis (AIS) refers to scoliosis with main curve in thoracolumbar/lumbar segments [1], which has evoked widely controversy especially about the choice of lowest instrumented vertebra (LIV). Balancing stability and mobility are of the utmost importance, since longer segments involved impair mobility [2], while shorter segments induce instability to the alignments and may cause an adding-on phenomenon after surgery [3]. Previous literature has reported multiple selection criteria for LIV in posterior lumbar fusion in these patients [4-7], taking variable measurements of LIV into consideration.
L3 and L4 are the 2 most common selections as the LIV. Many studies recommend L3 as the LIV over L4, citing benefits such as longer fusions below L3 that might lead to severe impairment of lumbar motion function [8], and the patientsŌĆÖ coronal trunks adjusting themselves to balance positions as long as there were more than 2 motion segments left below the fused section [9]. In addition, on account of increasing intradiscal pressure near the LIV, Auerbach et al. [10] urged that the longer segments preserved below LIV, the better long-term prognosis could be achieved. However, some studies discouraged the widespread selection of L3 as LIV because of possibility of distal adding-on and distal junctional kyphosis (DJK) [11], although the specific rate of distal adding-on phenomenon and DJK has sparsely discussed. Therefore, it is still mandatory to explore the radiological outcomes of LIV at L3 or L4 in Lenke 5C type AIS to assist the choice of LIV.
The implications of LIV was variable among different authors, as the degree of rotation and the stable vertebra are of highly concerned in selection of LIV [12]. However, the selection of LIV varies among surgeons even the baseline factors are similar. Therefore, in order to state the adequacy of L3 with little rotation degree as LIV in Lenke 5C type AIS, we conducted a case-match study of 82 patients to compare the incidence of postoperational adding-on phenomenon and DJK, with a minimum 2-year follow-up. We hypothesized that L3 may be an effective choice for LIV in Lenke 5C type AIS.
Following Institutional Review Board approval of Peking Union Medical College Hospital (I-23PJ961) regarding human subjects, 2 groups of Lenke 5C AIS patients who underwent posterior spinal fusion surgeries were retrospectively analyzed. The L3 group refers to patients whose LIV located at L3, and the L4 group involves patients with LIV at L4. Inclusion criteria were as follows: (1) patients diagnosed with Lenke 5C type AIS; (2) patients who underwent selective posterior thoracolumbar/lumbar fusion surgery at Peking Union Medical College Hospital from 2015ŌĆō2020; (3) LIV was L3 or L4; (4) acquired informed patient consent; (5) with a minimum of 2-year follow-up. Patients with incomplete clinical data were excluded. Our LIV selection criteria were as follows [4]: (1) the most cephalad vertebrae touched by central sacrum vertical line (CSVL); (2) the Nash-Moe rotation is grade II or less on the standing anteroposterior (AP) radiograph [13]; (3) the CSVL crosses between the 2 pedicles of LIV on concave bending film; (4) the vertebrae which is not at the kyphosis apex. All 4 criteria must be met for a vertebra to be considered as the LIV. One thing should be noted is that the CSVL in our criteria is different from that in the SRS definition [14], which is the plumb line through the sacrum center. Our CSVL follows the King classification definition [15], which is perpendicular to the crest line.
The detailed procedure of the surgery is as follows [4]: patients were placed in the prone position on a radiolucent table. After making a standard midline incision, we made a subperiosteal dissection of the posterior soft tissues to the tips of the transverse processes. We placed uniplanar pedicle screws bilaterally at every segment in all patients with a free-hand technique. For rigid curves or ones with the lower instrumented vertebra barely touched by the coronal spinal vertical line on the preoperative AP view, multiple-level Ponte osteotomies were performed. After inserting contoured cobalt-chromium-molybdenum alloy rods, bilateral rod rotation and segmental derotation technique was used to correct the deformity. If necessary, compression, distraction, and in situ bending maneuvers were added under fluoroscopic control. The alignment of the disc below lower instrumented vertebra was evaluated again with fluoroscopy. The lamina and transverse processes were thoroughly decorticated, and allograft bone material was used for fusion. During the whole procedure, neurophysiological monitoring was done with motor-evoked potentials, somatosensory-evoked potential, and electromyography.
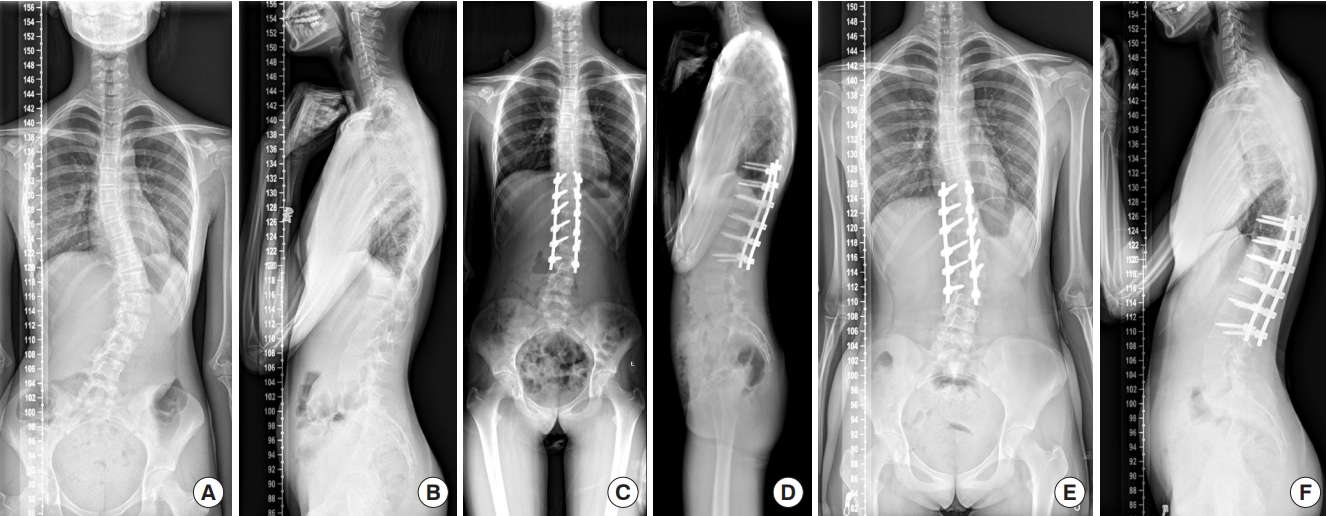
The function of case-control matching in IBM SPSS Statistics ver. 23.0 (IBM Co., Armonk, NY, USA) was used in this study. We applied 1:1 case-control matching for cases from 2 groups by RisserŌĆÖs sign (┬▒ 0), sex (┬▒ 0), lowest end vertebra (LEV) (┬▒ 0), age (┬▒ 2), and main Cobb angle (┬▒ 5). Finally, 41 pairs of patients were included in this study. The analytic results were assessed by comparing the radiographic outcomes between the 2 groups. The scheme of AP and lateral X-rays before surgery, after surgery and at the last follow-up is shown in Fig. 1.
At the time of surgery, baseline data including age, sex, Risser grade, height, weight, body mass index, and follow-up time were collected. The number of total fusion levels and thoracic fusion levels were collected after the surgery. To assess the stability of the spine postsurgery, the following subjects were recorded before surgery, after surgery and at the last follow-up: (1) coronal lumbar Cobb angle; (2) coronal thoracic Cobb angle; (3) ΔHshoulders: the height difference between 2 shoulders, which is defined as positive when left shoulder is higher while negative at the opposite; (4) trunk shift: evaluated by the distance between C7 plumb line and CSVL. The negative value indicated the leftward trunk shift, while positive value indicated the rightward trunk shift; (5) coronal balance/coronal imbalance (CIB): represents the number of patients without or with coronal imbalance. If the trunk shift exceeds 2 cm, it is defined with coronal imbalance; (6) sagittal vertebral axis (SVA): evaluated by the horizontal distance between a plumb line drawn from center of C7 and posterior superior sacral end plate; (7) sagittal balance/sagittal imbalance (SIB): represents the number of patients without or with sagittal balance. SIB is defined with SVA exceeding 4 cm; (8) distal junctional angle (DJA): sagittal Cobb angle of the intervertebral disc below the LIV, while negative value stands for lordosis; (9) DJK: defined with DJA larger than 10°; (10) lumbar-sacral compensational curve: Cobb angle between inferior endplate of the LEV and the superior endplate of the S1; (11) sacral slanting: defined with the angle between the horizontal line and the upper end plate of the sacrum on the AP radiology larger than 5°; (12) LIV rotation: the degree of rotation of LIV, evaluated by Nash-Moe classification [16]; (13) LIV tilt: the angle of the inferior endplate of the LIV from the horizontal plane; (14) LIV translation: the distance between the center of LIV and CSVL; (15) touched vertebra: the lowest barely touched vertebra refers to the most cephalad vertebra touch by CSVL, while the lowest substantial touched vertebra refers to the most cephalad vertebra whose pedicle is touched by CSVL. According to different definition of CSVL by King et al. [15] and SRS [14], there are 2 set of touched vertebra listed in the table; (16) adding-on phenomenon [17]: defined as the extension of the involved vertebrae within the distal curve between the first erect radiograph and the latest one, with either an increase larger than 5 mm in the deviation of the first vertebra below the LIV or an increase of more than 5° in the angulation of the first disc below the LIV. All data were collected by 2 individual experienced orthopedists with crosschecking, when the data were no consistent, a third confirmation by another orthopedist was made.
We used IBM SPSS Statistics ver. 23.0 to analyze the data collected above. Categorical variables were summarized as frequencies, and continuous variables as median (interquartile range). Mann-Whitney U-test and Wilcoxon test were used in significant tests for continuous variables, while chi-square test was used in significant test for categorical variables, and the chosen level of significance was 0.05. To evaluate the prevalence of CIB, SIB, adding-on phenomenon and DJK, we calculated the odds ratio (OR) between the 2 groups and the 2-sided exact significant value through Fisher precision probability test.
Table 1 lists the baseline information of the patients included in this study. After case-matching, there were 1 male and 40 females in each group. There was a significant difference in total fusion segments between both groups. The total fusion segments in the L3 group (median [interquartile range]: 5.0 [6.0ŌĆō5.0]) were shorter than those in the L4 group (6.0 [6.5ŌĆō6.0]), while the thoracic fusion segments in the L3 group (2.0 [3.0ŌĆō2.0]) were similar with those in L4 group (2.0 [2.5ŌĆō2.0]).
There was no significant difference of lumbar and thoracic Cobb angle at any time-spot, indicating comparable deformity correction effect of the main curve between the 2 groups. Furthermore, to evaluate the alignment balance, the comparisons of ΔHshoulders, trunk shift, SVA, and lumbar-sacral compensational curve were carried out in Table 2. As a result, apart from the DJA and lumbar-sacral compensational curve, there was no significance of alignment balance between the 2 groups. As for the DJA, the more negative value in L4 group indicated the larger lordosis reconstructed by the LIV at L4 (p<0.001). Lumbar-sacral compensational curve was significantly lower in L4 group than that in the L3 group after surgery (p = 0.006) and at the last follow-up (p < 0.001). There was no significance of sacral slanting between both groups in the follow-up.
The LIV rotation was large in L3 group than L4 group at preoperative (p = 0.005), and decreased to 0┬░ at the last follow-up in both groups. L4 group had larger LIV tilt than L3 group at the last follow-up (p = 0.036). The LIV translation and LIV Cobb were comparable at preoperative, postoperative and the latest follow-up in both group (p Ōēź 0.05) (Table 3).
To assess the contribution of LIV at L3 to postoperational alignment imbalance, we introduced the OR to evaluate whether LIV at L3 was risk factor or protective factor, results were shown in Table 4. As a result, LIV at L3 turned out to be protective factors for coronal and sagittal balance after the surgery. For the adding-on phenomenon, LIV at L4 might be minor protective factors in the long term. The sacral slanting of both groups remained similar before the operation, after the operation and at the last follow-up. According to the results of Fisher precision probability test, there was no significant difference of postoperational alignment imbalance between the 2 groups.
The selection of LIV for Lenke type 5C has been a controversial topic. The main concerns for the decision lie in the main Cobb angle and last ended vertebra [5,6,18]. Wang et al. [19] developed a formula to assist the selection of LIV in Lenke type 5C AIS from a 2-year follow-up study, with which the postoperative distance between thoracic/lumbar apical vertebra and CSVL could be predicted by the preoperative distance between LIV and CSVL. Furthermore, Erdem et al. [20] found out that the application of preoperative traction x-rays under general anesthesia is able to assess the proper LIV more accurately than standing AP and lateral x-rays. No matter what assessments are applied by different surgeons, balancing the stability and range of motion (ROM) of instrumented spine is the key to acquiring the satisfactory correction, as extending the instrumented segments might advance better stability but impair the ROM of whole alignments. Although there are tremendous selection criteria for LIV, most of them chose L3 or L4 as the LIV. In order to compare the efficacy of the 2 most selected choices, we presented a case-match study by dividing the LIV to L3 or L4.
As the arguments of the selection of LIV concentrate on the balance of stability and mobility, the fused segment was highly concerned in our study. As the results showed, the overall fused segments in the L3 group (5.0 [6.0ŌĆō5.0]) are significantly (p<0.001) shorter than those in L4 group (6.0 [6.5ŌĆō6.0]), while the fused segments in thoracic segments in the L3 group (2.0 [3.0ŌĆō2.0]) are similar with those in the L4 group (2.0 [2.5ŌĆō2.0]). The thoracic spine is considered to have a restricted ROM during flexion and extension compared with that of cervical and lumbar spine, because of the existence of the rib cage. Therefore, with more reserved motion segments in L3 group, the ROM in L3 group was probably higher than that in L4 group.
The deformity correction is crucial for Lenke 5C type AIS. Banno et al. [21] retrospectively reported a cohort of 49 AIS patients with Lenke type 5C curves whose LIV was at L3 or L4. The results indicated that the thoracic/lumbar curve was reduced to a similar degree (p = 0.925, p = 0.082). Ozkunt et al. [22] analyzed the correction effect of 42 patients with Lenke type 5 AIS, the Cobb angle was reduced to 7.68┬░ and 7.98┬░ in L3 group and L4 group, without significant difference between the 2 groups. Consistent with the reported articles, the thoracic/lumbar curve in our cohort was reduced to a similar degree with mild residual Cobb angle in both groups, indicating both L3 and L4 are both adequate selections to achieve satisfying curve correction. Both groups achieved good radiologic outcomes according to LIV parameters, which confirmed the selection criteria of LIV of Lenke 5C AIS patients according to our center could be coopted. Given the similar results of shouldersŌĆÖ height and trunk shift, it is showed that the coronal alignment balance was satisfactorily reconstructed by LIV at L3 or L4. As for the sagittal alignment, once the satisfactory postoperational balance was achieved, sagittal trunk imbalance seems not to be an important issue, which differs from that in Lenke 1C type AIS. In our research, similar SVA between both groups during the whole follow-up time proved the validity of L3 and L4 as LIV to reconstruct the sagittal balance.
It is important to note that selecting the wrong LIV can result in complications and deformity progression. Unsatisfactory clinical outcome after surgery, as defined by Chang et al. [23], includes adding-on phenomenon, LIV tilt > 10┬░, or coronal balance > 2 cm. Distal adding-on phenomenon refers to progressive correction loss of distal segments, caused by lumbar vertebral deviation or LIV disc angulation [24]. DJA is defined as the sagittal Cobb angle of intervertebral disc inferior to the LIV, which predicts the occurrence of DJK once it is higher than 10┬░. As shown in previous study, inappropriate selection of LIV, larger LIV translation, and skeletal immaturity rise the risk for postoperational distal adding-on effect, especially in Lenke 1A and 2A AIS [25,26]. Moreover, it has been reported [23] that there is higher risk of unsatisfactory clinical outcomes in the L3 group than in the L4 group. In addition, Hyun et al. [27] reported that adding-on phenomenon and DJK is more likely prevalent after anterior spinal fusion than after posterior spinal fusion, even if the LIV in both groups were L3. As for posterior spinal fusion, the prevalence of DJK or adding-on phenomenon at the last follow-up was reported as 13.1% [11]. To prevent DJK, Yang et al. [28] advised that choosing the LIV at or below stable sagittal vertebra can reduce the risk of DJK. However, in our study, LIV at L3 seemed to be a protective factor from coronal/SIB and adding-on phenomenon, although without any significant difference. In addition, there were no reports of DJA in both the L3 and L4 group, indicating similar corrective effect whether the LIV locate at L3 or L4. Furthermore, Enercan et al. [29] demonstrated similar rates of disc degeneration and facet joint degeneration between groups of LIV at L3 and L4. Koller et al. [30] reported similar lumbar-sacral compensational curve with LIV at L3 or L4 in patients with Lenke 3, 4, and 6 AIS. On the contrary, our results showed there was a larger compensational curve in the L3 group than that in the L4 group, although the angles in both groups remained in a low range. However, as Koller et al. [30] pointed out, lumbar-sacral curve might compensate the postoperational residual curve, which would be impeded by longer fusion. Longer follow-up is needed to clarify whether larger compensational curve would accelerate the disc degeneration and joint facet degeneration or compensate the residual curve. Furthermore, sacral slanting might be a way for scoliotic spine to compensate itself, and should be a critical consideration in selecting LIV. As Lee et al. [31] reported, postoperational sacral slanting could negate the bending force when the directions of sacral slanting and L4 tilt were the same, which diminished the rate of adding-on phenomenon. In our study, the incidence of coronal imbalance and adding-on phenomenon was low. Therefore, a larger prospective cohort study is needed for further exploration of the importance of sacral slanting in Lenke 5C AIS.
As a result, selection of LIV at L3 results in similar correction outcomes as LIV at L4. However, the lumbar-sacral compensation curve is significantly larger in L3 group than that in L4 group, indicating a higher possibility of emergence of lumbar-sacral compensation whose LIV is L3. Furthermore, the LIV at L3 might be helpful to avoid coronal/SIB after surgery. Therefore, the selection of L3 as LIV might have some merit in maintaining better stability and mobility for the whole alignments.
The advantages of this study are as follows: Firstly, we include a relatively large group of patients with Lenke type 5C AIS, which verified the results of our study. Secondary, all of the surgeries were conducted by a single team of doctors, certifying the consistency of the data in both groups. Thirdly, we match the cases with preconditions to eliminate the differences of preoperational parameters between different groups, in order to compare clinical outcomes objectively.
However, there are still some limitations in our study. First, we only matched the sex, age, RisserŌĆÖs sign, LEV position and preoperational coronal Cobb angle between the 2 groups, leaving other confounding factors. Secondary, this study is retrospective and could not avoid missing data. Therefore, a further random, prospective study with a longer follow-up about the different clinical outcomes of LIV at L3 or L4 should be conducted in the near future.
In conclusion, the clinical outcomes of LIV at L3 and L4 were compared in Lenke type 5C AIS. LIV at L3 could preserve more motion segments for patients with Lenke 5C AIS. The selection of LIV of L3 or L4 may not have negative effect on radiologic complications such as SIB, CIB, PJK, adding-on phenomenon. Therefore, due to the efficiency and safety in moderate Lenke type 5C AIS, L3 could be a competent choice as LIV.
NOTES
Fig.┬Ā1.
The scheme of anteriorposterior and lateral x-rays before surgery (A, B), after surgery (C, D), and at the last follow-up (E, F).
Table┬Ā1.
Demographic information
| Variable | L3 group | L4 group | p-value |
|---|---|---|---|
| Age (yr) | 14.0 (16.0ŌĆō13.0) | 14.0 (16.0ŌĆō13.2) | 0.742 |
| Sex, female:male | 40:1 | ||
| RisserŌĆÖs sign | |||
| ŌĆā0 | 5 (12.2) | ||
| ŌĆā1 | 0 (0) | ||
| ŌĆā2 | 3 (7.3) | ||
| ŌĆā3 | 6 (14.6) | ||
| ŌĆā4 | 25 (61.0) | ||
| ŌĆā5 | 2 (4.9) | ||
| Fused segments | 5.0 (6.0ŌĆō5.0) | 6.0 (6.5ŌĆō6.0) | < 0.001 |
| Fused T segments* | 2.0 (3.0ŌĆō2.0) | 2.0 (2.5ŌĆō2.0) | 0.152 |
| Height (m) | 1.62 (1.66ŌĆō1.56) | 1.61 (1.65ŌĆō1.57) | 0.845 |
| Weight (kg) | 49.0 (52.2ŌĆō45.5) | 49.0 (53.3ŌĆō44.5) | 0.993 |
| BMI (kg/m2) | 19.1 (20.3ŌĆō17.8) | 18.9 (20.6ŌĆō17.3) | 0.795 |
| Follow-up (yr) | 2.0 (4.0ŌĆō2.0) | 2.0 (4.3ŌĆō2.8) | 0.150 |
Table┬Ā2.
Radiologic assessments of alignments in L3 and L4 groups
Table┬Ā3.
The parameters of LIV
Table┬Ā4.
Coronal and sagittal alignment related to different LIV
| Variable | L3 group | L4 group | p-value | L3 OR |
|---|---|---|---|---|
| CB/CIB* | ||||
| ŌĆāPreoperative | 33/7 | 26/15 | 0.080 | 0.37 |
| ŌĆāPostoperative | 36/4 | 35/6 | 0.738 | 0.65 |
| ŌĆāAt last follow-up | 33/2 | 38/0 | 0.226 | |
| SB/SIBŌĆĀ | ||||
| ŌĆāPreoperative | 30/9 | 31/9 | 1.000 | 1.03 |
| ŌĆāPostoperative | 39/2 | 34/7 | 0.155 | 0.25 |
| ŌĆāAt last follow-up | 30/3 | 34/3 | 1.000 | 1.13 |
| Adding-on phenomenonŌĆĪ | ||||
| ŌĆāPostoperative | 2/37 | 1/39 | 0.615 | 2.11 |
| ŌĆāAt last follow-up | 9/25 | 3/33 | 0.059 | 3.96 |
| DJK┬¦ | ||||
| ŌĆāPostoperative | 41/0 | 41/0 | 1.000 | |
| ŌĆāAt last follow-up | 41/0 | 40/1 | 1.000 | |
| Sacral slantingll | ||||
| ŌĆāPreoperative | 15/25 | 19/19 | 0.266 | 0.6 |
| ŌĆāPostoperative | 5/33 | 8/33 | 0.550 | 0.625 |
| ŌĆāAt last follow-up | 9/30 | 16/25 | 0.152 | 0.469 |
REFERENCES
1. Lenke LG. Lenke classification system of adolescent idiopathic scoliosis: treatment recommendations. Instr Course Lect 2005;54:537-42.

2. Barsi J, Caprio B, Garg S, et al. Do Intraoperative LIV-tilt and disk angle remain stable at 2-year follow-up compared with upright radiographs in patients with idiopathic scoliosis?: a retrospective cohort study. J Spinal Disord Tech 2015;28:264-9.

3. OŌĆÖDonnell C, Michael N, Pan X, et al. Anterior spinal fusion and posterior spinal fusion both effectively treat Lenke type 5 curves in adolescent idiopathic scoliosis: a multicenter study. Spine Deform 2018;6:231-40.


4. Zhuang Q, Zhang J, Wang S, et al. How to select the lowest instrumented vertebra in Lenke type 5 adolescent idiopathic scoliosis patients? Spine J 2021;21:141-9.


5. Phillips L, Yaszay B, Bastrom TP, et al. L3 translation predicts when L3 is not distal enough for an ŌĆ£idealŌĆØ result in Lenke 5 curves. Eur Spine J 2019;28:1349-55.



6. Sun Z, Qiu G, Zhao Y, et al. Lowest instrumented vertebrae selection for selective posterior fusion of moderate thoracolumbar/lumbar idiopathic scoliosis: lower-end vertebra or lower-end vertebra+1? Eur Spine J 2014;23:1251-7.



7. Liu Z, Guo J, Zhu Z, et al. Role of the upper and lowest instrumented vertebrae in predicting the postoperative coronal balance in Lenke 5C patients after selective posterior fusion. Eur Spine J 2013;22:2392-8.




8. Ilharreborde B, Ferrero E, Angelliaume A, et al. Selective versus hyperselective posterior fusions in Lenke 5 adolescent idiopathic scoliosis: comparison of radiological and clinical outcomes. Eur Spine J 2017;26:1739-47.



9. Yang X, Hu B, Song Y, et al. Coronal and sagittal balance in Lenke 5 AIS patients following posterior fusion: important role of the lowest instrument vertebrae selection. BMC Musculoskelet Disord 2018;19:212.




10. Auerbach JD, Lonner BS, Errico TJ, et al. Quantification of intradiscal pressures below thoracolumbar spinal fusion constructs: is there evidence to support ŌĆ£saving a levelŌĆØ? Spine (Phila Pa 1976) 2012;37:359-66.

11. Hyun SJ, Lenke LG, Kim Y, et al. Adolescent idiopathic scoliosis treated by posterior spinal segmental instrumented fusion: when is fusion to L3 stable? J Korean Neurosurg Soc 2021;64:776-83.




12. Chang DG, Yang JH, Suk SI, et al. Importance of distal fusion level in major thoracolumbar and lumbar adolescent idiopathic scoliosis treated by rod derotation and direct vertebral rotation following pedicle screw instrumentation. Spine (Phila Pa 1976) 2017;42:E890-8.


13. Shao X, Sui W, Deng Y, et al. How to select the lowest instrumented vertebra in Lenke 5/6 adolescent idiopathic scoliosis patients with derotation technique. Eur Spine J 2022;31:996-1005.



14. Malfair D, Flemming AK, Dvorak MF, et al. Radiographic evaluation of scoliosis: review. AJR Am J Roentgenol 2010;194(3 Suppl):S8-22.


15. King HA, Moe JH, Bradford DS, et al. The selection of fusion levels in thoracic idiopathic scoliosis. JBJS 1983;65:1302-13.

16. Lam GC, Hill DL, Le LH, et al. Vertebral rotation measurement: a summary and comparison of common radiographic and CT methods. Scoliosis 2008;3:16.




17. Ogura Y, Okada E, Fujii T, et al. Midterm surgical outcomes of a short fusion strategy for adolescent idiopathic scoliosis with Lenke 5C curve. Spine J 2020;20:361-8.


18. Ketenci IE, Yanik HS, Ulusoy A, et al. Lowest instrumented vertebrae selection for posterior fusion of Lenke 5C adolescent idiopathic scoliosis: can we stop the fusion one level proximal to lower-end vertebra? Indian J Orthop 2018;52:657-64.




19. Wang Y, B├╝nger CE, Zhang Y, et al. Lowest instrumented vertebra selection for Lenke 5C scoliosis: a minimum 2-year radiographical follow-up. Spine (Phila Pa 1976) 2013;38:E894-900.

20. Erdem MN, Karaca S, Korkmaz MF, et al. Criteria for ending the distal fusion at the L3 vertebra vs. L4 in surgical treatment of adolescent idiopathic scoliosis patients with Lenke Type 3C, 5C, and 6C curves: results after ten years of follow-up. Cureus 2018;10:e2564.



21. Banno T, Yamato Y, Oba H, et al. Should L3 be selected as the lowest instrumented vertebra in patients with Lenke type 5C adolescent idiopathic scoliosis whose lowest end vertebra is L4? J Neurosurg Spine 2021;35:330-9.


22. Ozkunt O, Karademir G, Sariyilmaz K, et al. Analysing the change of sagittal balance in patients with Lenke 5 idiopathic scoliosis. Acta Orthop Traumatol Turc 2017;51:377-80.



23. Chang DG, Suk SI, Song KS, et al. How to avoid distal adding-on phenomenon for rigid curves in major thoracolumbar and lumbar adolescent idiopathic scoliosis? Identifying the incidence of distal adding-on by selection of lowest instrumented vertebra. World Neurosurgery 2019;132:e472-8.


24. Wang Y, Hansen ES, H├Ėy K, et al. Distal adding-on phenomenon in Lenke 1A scoliosis: risk factor identification and treatment strategy comparison. Spine (Phila Pa 1976) 2011;36:1113-22.

25. Li Y, Bai H, Liu C, et al. Distal adding-on phenomenon in Lenke IA and Lenke IIA: risk analysis and selection of the lowest instrumented vertebra. World Neurosurg 2020;136:e171-80.


26. Cho RH, Yaszay B, Bartley CE, et al. Which Lenke 1A curves are at the greatest risk for adding-on... and why? Spine (Phila Pa 1976) 2012;37:1384-90.


27. Hyun SJ, Lenke LG, Kim Y, et al. The incidence of adding-on or distal junctional kyphosis in adolescent idiopathic scoliosis treated by anterior spinal fusion to L3 was significantly higher than by posterior spinal fusion to L3. Neurospine 2021;18:457-63.




28. Yang J, Andras LM, Broom AM, et al. Preventing distal junctional kyphosis by applying the stable sagittal vertebra concept to selective thoracic fusion in adolescent idiopathic scoliosis. Spine Deform 2018;6:38-42.


29. Enercan M, Kahraman S, Yilar S, et al. Does it make a difference to stop fusion at L3 versus L4 in terms of disc and facet joint degeneration: an MRI study with minimum 5 years follow-up. Spine Deform 2016;4:237-44.



- TOOLS
- Related articles in NS
-
Journal Impact Factor 3.2



























