INTRODUCTION
Ependymomas are the most common intramedullary tumor in adults, and they account for 60% of intramedullary spinal cord tumors14). Intramedullary spinal cord ependymomas arises from the ependymal cells lining the central canal6). Intramedullary ependymomas are most commonly observed in the cervical and cervico-thoracic regions. Spinal cord ependymomas are usually benign and curable with complete surgical resection or in combination with radiotherapy2,11). However the anaplastic ependymomas frequently recur and metastasize and therefore adjuvant radiotherapy should be considered even after complete surgical resection13).
Administration of postoperative adjuvant radiotherapy may result in life-threatening or serious neurologic deficits8), and those occurring in the cervicomedullary junction are particularly severe.
We report herein a case of an anaplastic ependymoma located in the cervicomedullary junction, who experienced recurrent disease after initial partial resection and underwent repeat surgery to achieve complete resection, and who showed good clinical outcome without adjuvant radio-therapy.
CASE REPORT
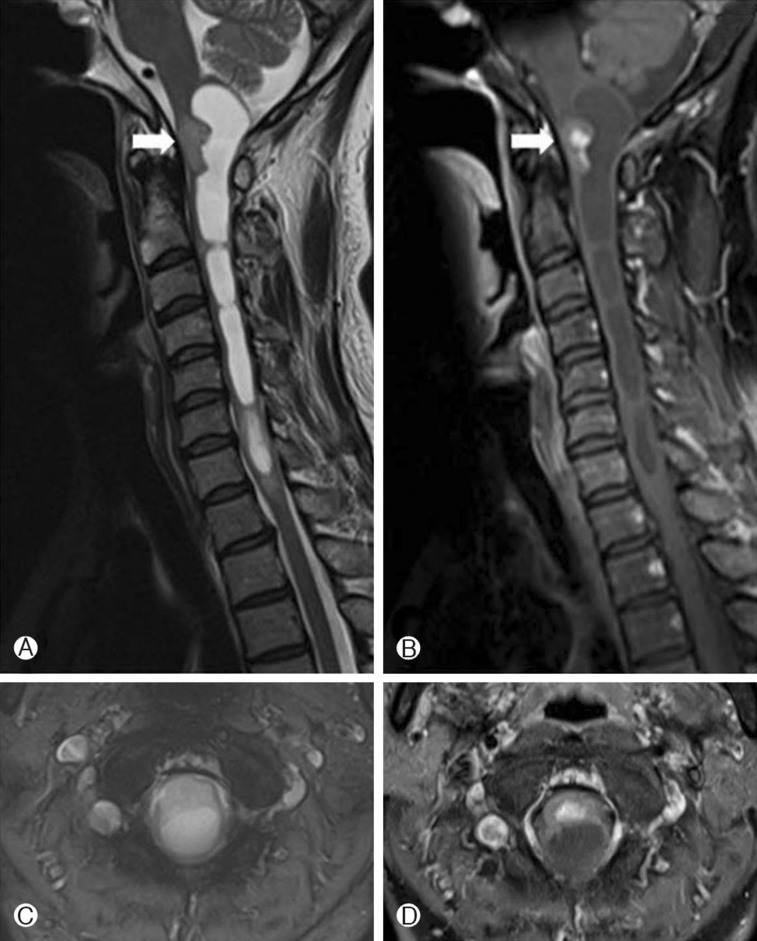
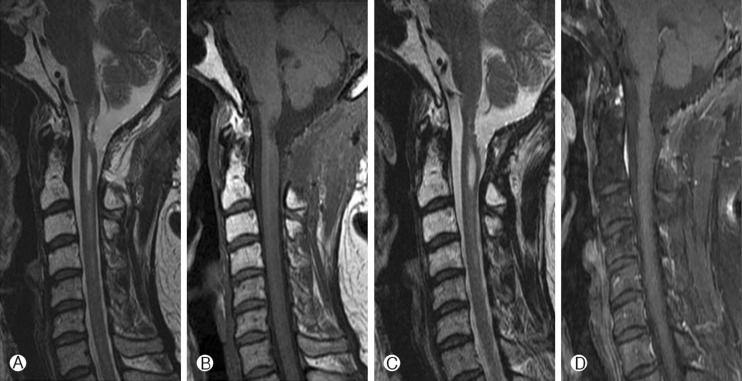
A 45-year-old woman developed right arm pain which radiated down to all 5 finger tips for several months initially. The past medical history was unremarkable. She had visited a local hospital and the magnetic resonance imaging (MRI) demonstrated a solid intramedullary tumor with syrinx at the cervicomedullary junction which was well enhanced by gadolinium contrast media (Fig. 1). The well-enhanced tumor was located at the ventral portion of the cord and the linear syrinx was located from the cervicomedullary junction to C7. For tumor removal, a suboccipital decompression and removal of the tumor was performed at the local hospital. The pathologic finding was an ependymoma at that time. After the first surgery, she suffered from pain and tingling sensation of her right arm which gradually worsened. The follow-up MRI 6 months later after the first surgery revealed an enlarged enhancing tumor and syrinx compared with initial MRI (Fig. 2). The patient was referred to our institution and the initial neurologic examination demonstrated that she had grade 4 motor weakness of her right arm with tingling sensations. Revision surgery was performed. The tumor was seen to be originating from the medulla oblongata to the C1 spinal cord with a huge sized syrinx. The scar tissue was intermingled with neural tissue on the upper, lower and dorsal portions of the tumor. But the ventral portion of the tumor showed a clear demarcation between the tumor and normal neural tissue. Gross total resection of tumor was achieved, despite the previous surgery. The pathological diagnosis was an anaplastic ependymoma (Fig. 3) and the MIB-1 index was increased mildly. Immediate after the surgery, the patient showed mild hemipaparesis of her right side. In consideration of the detrimental effects of radiotherapy on the twice-surgery area we opted for short-term follow-up rather than adjuvant radiotherapy. On the follow-up MRI at 3 months and 7 months after the surgery, no residual or recurrent tumor was observed (Fig. 4). The right side hemiparesis which occurred immediately after surgery improved such that normal everyday activity was almost normal 1 month after the surgery, and at post operative 8 months the neurologic evaluation in the follow-up period did not reveal any new or residual deficits.
DISCUSSION
Ependymoma is the most common intraspinal tumor14). Ependymomas arise from ependymal cells that line the ventricles and central canal of the spinal cord13,14). It comprises 15% of spinal cord tumors and up to 60% of spinal cord gliomas2). A previous study reported the incidence as four regions were localized in the thoracic region (19%), 7 in the lumbar region (34%), 4 in the cervical region (19%), 3 in the cervicothoracic region (14%), and 3 in the conus medullaris (14%)14). In the same study, pathological examinations revealed that 7 (34%) lumbar region cases were identified as myxopapillary ependymomas stemming from the filum terminale, and 14 (66%) other cases were intramedullary ependymomas. There were no malignant ependymoma cases14).
Several cases of clear cell ependymoma of the medulla oblongata has been reported and also a case of cervicomedullary junction tanycytic ependymoma3,8). In general, ependymomas includes anaplastic (malignant) ependymomas, and myxopapillary ependymomas, cellular, papillary, clear cell, and tanycytic subtypes1,5,7,10,13). Almost all spinal cord ependymomas are histologically benign tumors2,13) and curable with complete surgical resection or in combination with radiotherapy16). Maximal resection of the tumor while protecting neurological function is the golden rule in surgical treatment of spinal ependymomas5). Also, anaplastic ependymomas are less common and has worse prognosis5,14,16).
In our present case, tumor originated from the medulla oblongata to the C1 spinal cord with a huge sized syrinx. Gross total removal (GTR) of the tumor was successfully achieved in spite of the previous surgical treatment and location of cervicomedullary junction. The pathology was confirmed as anaplastic ependymoma.
Careful manipulation of the tumor results in reducing the postoperative neurologic deficit and a significant favorable clinical outcome. As anaplastic ependymomas frequently recur and is accompanied with a poor prognosis, it is important that they are totally removed grossly in order to achieve a good outcome5,12). In the operation field, clear demarcation was observed between the tumor and neural tissue, and therefore complete resection could be achieved. After the complete resection, we determined that conservative management without adjuvant radiotherapy would be the best therapeutic plan for the patient.
The complete resection alone in spinal cord "ependymoma" without local radiotherapy can achieve excellent tumor control and survival5). Since a residual tumor or "malignant ependymoma" has a poor prognosis, postoperative radiotherapy is recommended in the past literature review.10,11,15). The majority of reports propose that radiotherapy in those who have a "anaplastic ependymoma" should be added to the surgical resection13).
The ependymoma of this patient was located at the cervicomedullary junction and therefore consideration of the possibility of the radiotherapy induced central nervous system injury should be taken into account. In addition, information pertaining to the scope and effect of radiation therapy is lacking and remains under debate8). The radiation therapy may result in the gliosis, fibrosis and hardening of ependymoma4). The radiation therapy can also predispose the patient radiation induced myelopathy and result in the severe neurologic damage4). As the mild motor weakness that was observed in the immediate post-operation period was expected to improve with rehabilitative therapy, and because of the possibility of neurologic deficit and delayed recovery, radiotherapy was not included in the postoperative treatment plans. During the follow-up period, no new neurologic symptoms appeared, the neurologic deficit improved, and the MRI demonstrated that there was no residual or recurrent tumor.
We agree that adjuvant radiotherapy is necessary in patient with anaplastic ependymomas. However, in the group of patients in whom radiotherapy is envisaged to consequently result in severe neurological deficits, complete resection and short-term follow up may be a valid alternative.
CONCLUSION
Anaplastic ependymoma arising from the cervicomedullary junction is uncommon. Surgical resection should be considered as an initial treatment for residual or recurred anaplastic ependymomas, followed by postoperative radiotherapy. Adjuvant radiotherapy in patients with complete resected anaplastic ependymoma may not always be necessary. In patients who received the surgical resection at the cervicomedullary junction, complete resection alone might be a strategic recommendation.