|
 |
- Search
|
|
||
Abstract
Objective
To assess the effect of transitioning to remote working during the coronavirus disease 2019 pandemic in a population of adults affected by chronic low back pain (cLBP).
Methods
An online questionnaire was sent by email to teleworkers affected by cLBP. Demographic data, remote working features and tasks, and LBP burden were analyzed. The psychological burden of remote working was evaluated with the World Health Organization Five Well-Being Index and the Patient Health Questionnaire-2. LBP severity was evaluated using a visual analogue scale. LBP-related disability was assessed using the Oswestry Disability Index. The effect of LBP on working capacity was examined with the Occupational Role Questionnaire. Independent risk factors related to LBP worsening were identified using a multivariate logistic regression model.
Results
During remote working, LBP severity was significantly higher compared to previous in-person working (p < 0.0001), as well as average weekly work hours (p < 0.001). Furthermore, the risk of LBP worsening was associated with higher depression scores (odds ratio [OR], 1.38; 95% confidence interval [CI], 1.00â1.91; p = 0.048), increased stress levels (OR: 3.00, 95% CI: 1.04â8.65; p = 0.042), and being divorced (OR: 4.28, 95% CI: 1.27â14.47; p = 0.019). Conversely, living with others (OR: 0.24, 95% CI: 0.07â0.81; p = 0.021), and reporting unchanged stress levels (OR: 0.22, 95% CI: 0.08â0.65; p = 0.006) were associated with a lower risk of LBP worsening.
Since December 2019, the pandemic outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused an unprecedented global health issue, with > 574,000,000 cases and approximately 6,500,000 deaths worldwide [1]. Due to the high transmissibility of the coronavirus disease 2019 (COVID-19), personal-contact activities and short-distance interactions have been minimized to reduce viral dissemination during social and clinical encounters [2]. At the socioeconomic level, this has prompted a profound reorganization of the working world with an increasing number of individuals working remotely from home [3]. In a matter of months, several companies and employers shifted to âremote workingâ (also known as âtelework,â âsmart working,â âhome working,â etc.), consisting in carrying out a job outside the workplace on a regular basis with the use of information technology [4]. Yet, while preserving productivity and the prosecution of both public and private services, prolonged remote working has demonstrated to negatively impact on workersâ physical and mental wellbeing [5]. Indeed, decreased physical activity and the sedentary lifestyle associated with social confinement and working from home have been related to a higher risk of several systemic and musculoskeletal disorders (MSDs) [6], including chronic low back pain (cLBP) [7].
Low back pain (LBP) is the main cause of disability worldwide, resulting in a huge medical burden and economic costs for the healthcare systems and society [8]. Indeed, studies in European countries indicate that total costs associated with LBP vary between 0.1%â2% of the gross domestic product [9], with over 80% consisting in indirect costs due to the loss of productivity and disability payments [10]. The main risk factors for LBP include aging, smoking, obesity, sedentary occupations, physical inactivity, and depression [11-13]. Considering the impossibility to participate in leisure activities, increased time spent home and prolonged sitting during remote working, the prevalence and severity of LBP has significantly increased during the pandemic [7]. However, it is still unclear how remote working impacts on individuals affected by LBP and how transitioning to this new work modality has influenced both work- and health-related outcomes.
The aim of this cross-sectional study was to investigate the effect of transitioning to remote working in an adult population affected by cLBP. We hypothesized that diverse working conditions, home office equipment as well as perceived advantages, disadvantages and impact on job satisfaction, productivity, well-being and stress may differentially influence the severity of LBP in this subset of workers.
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Campus Bio-Medico University of Rome (approval number: 76/19 OSS ComEt CBM). Informed consent was obtained from all study subjects upon recruitment. The study was reported according to STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines (Supplementary Material 1) [14].
A cross-sectional study was performed at Campus Bio-Medico University of Rome (Rome, Italy) through an online questionnaire. The target population consisted of working-age adults diagnosed with cLBP due to degenerative disc disease after attending the Spine Clinic of Campus Bio-Medico University Hospital Foundation (Rome, Italy). All patients underwent thorough history-taking and physical examination, as well as lumbar spine imaging evaluation to confirm the diagnosis (isolated axial LBP lasting â„ 12 weeks associated with radiographic or magnetic resonance imaging evidence of intervertebral disc degeneration). Participants were recruited if they reported a history of cLBP and worked remotely from home in the previous 18 months. Eligible subjects were reached by phone and recruited after a thorough explanation of the study aims and methods and signature of the informed consent. Upon acceptance, a web-based questionnaire built with Google Forms (Google Inc., Mountain View, CA, USA) was sent by email to each participant. The questionnaire could be interrupted at any time, and the consent could be withdrawn by closing the browser. After 1 month, a reminder was sent to increase participantsâ responsiveness. Data were collected from September 2021 to June 2022.
The questionnaire was evaluated by a panel of experts belonging to different professional categories (3 orthopaedic surgeons, 1 occupational psychologist, 1 occupational doctor, and 2 remote workers who met the eligibility criteria for this study) who assessed its content, completeness, and level of comprehension. The questionnaire included 3 sections: (1) demographic and occupational information; (2) remote working features and tasks; (3) LBP burden.
In the first section, retrieved information included age, gender, civil status, highest qualification held, current field of work, specific job title, length of service, professional category, number of cohabitants, and number of minor children.
The second section investigated whether transitioning to remote working caused any changes in terms of tasks, work hours and salary compared to in-person working. In addition, information regarding workplace equipment (type of chair, desk, and devices), hours spent in standing and sitting position as well as perceived productivity, job satisfaction, stress level, and mental wellbeing during remote working were collected. More specifically, participants were asked about their perceived productivity, job satisfaction and stress level during remote working compared to in-person working and answers were evaluated using a 3-point Likert scale (âincreased,â âunchanged,â âdecreasedâ). The psychological burden of remote working was evaluated with 2 validated scores: the World Health Organization Five Well-Being Index (WHO-5) measuring the level of illness [15] and the Patient Health Questionnaire-2 (PHQ-2) measuring the frequency of depressed mood and anhedonia over the past 2 weeks [16]. Eventually, advantages and disadvantages of remote working were evaluated.
The third section was focused on LBP severity and related disability, as well as its relationship with occupational tasks. More specifically, subjects were asked if their LBP worsened after transitioning to remote working, to what extent LBP caused work absence and how it affected their working activities. LBP severity was evaluated using a visual analogue scale (VAS). LBP-related disability was assessed using the Oswestry Disability Index (ODI) [17]. The effect of LBP on working capacity was examined with the Occupational Role Questionnaire (ORQ) [18]. The Italian version of the questionnaire was sent over and the English translated version is reported (Supplementary Material 2).
In order to achieve a homogeneous sample and avoid participants with self-diagnosed LBP, only patients with LBP due to intervertebral disc degeneration certified by an orthopaedic surgeon were included and personally contacted by the authors, thus reducing selection bias.
Considering the change of LBP severity as the primary outcome for sample size calculation, the minimal clinically important difference (MCID) for LBP on VAS was determined based on previous data [19]. Assuming a power of 90% and an alpha of 0.05, a sample size of 50 individuals was calculated. To adjust for possible invalid questionnaire responses, considering a rate of 20%, the final sample size consisted of 60 subjects. After reaching the calculated sample size, additional eligible participants were included to increase the external validity of the study population.
Descriptive statistics were applied to analyze the characteristics of the sample. Continuous variables were reported as mean ±standard deviation, whereas categorical variables were reported as absolute and percentage frequencies (n, n%). The normality of data distribution has been assessed upon confirmation of the central limit theorem and determined with the Wilk-Shapiro text. Continuous variable differences between timepoints (before and during remote working) in the same individuals was evaluated using the paired t-test. The individual association of each variable on worsening of LBP (determined as an increase on VAS> 2 following the start of remote working, corresponding to the MCID [19]) was assessed with a logistic regression model. The independent variables considered were age, sex, civil status, number of cohabitants, number of minor children, work hours, % remote working, type of chair, type of desk, hours sitting, hours standing, productivity, stress, job satisfaction, WHO-5, PHQ-2, ODI, ORQ, and work. Odds ratio (OR) and 95% confidence intervals (CI) were estimated for each reference category. Formal analysis was conducted using the Stata 17.0 (StataCorp LLC, College Station, TX, USA). A p-value of < 0.05 was considered statistically significant.
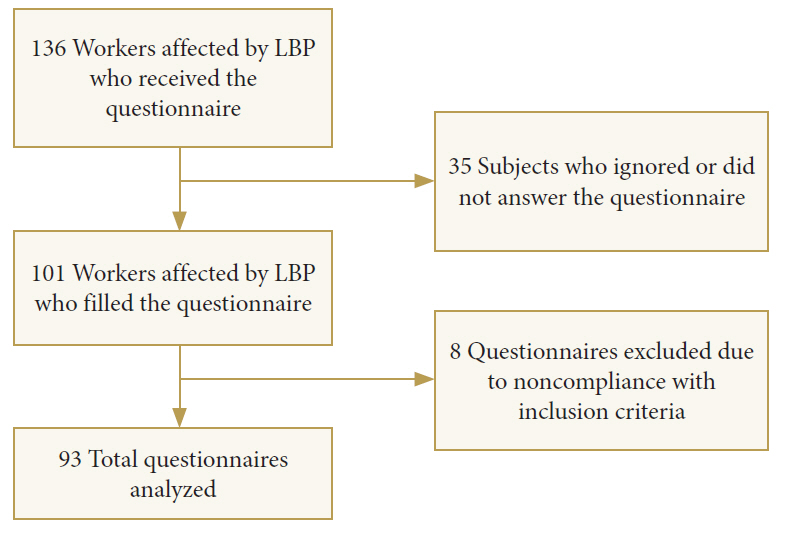
The questionnaire was delivered to 136 participants and a total of 101 responses were received (response rate: 74.26%). Out of the filled questionnaires received, 8 were excluded because participants did not meet one of the inclusion criteria. Eventually, 93 questionnaires were included in the study (Fig. 1). Participantsâ characteristics are reported in Table 1.
After transitioning to remote working, 68 subjects (73.1%) retained the same tasks, 4 (4.3%) were assigned to new tasks, and 27 (29%) changed their working time. Indeed, a statistically significant increase of average weekly work hours during remote working (38.09 ± 13.26) was reported compared to previous in-person working (34.98 ± 12.46, p < 0.001) (Fig. 2). A more detailed summary on the influence of remote working on working time is depicted in Table 2.
Most study participants (38, 40.9%) worked exclusively from home, while 18 (19.4%) worked > 50% of the time remotely and 37 (39.8%) worked < 50% of the time from home. With regard to the home office setup, 65 (69.9%) declared to have a dedicated workstation, 6 (6.5%) shared their workstation with others, while 22 (23.7%) did not have a fixed workstation. In terms of workstation equipment, 22 participants (23.7%) had a chair with fixed feet not adjustable in height and inclination, 4 (4.3%) had a rolling chair not adjustable in height and inclination, 17 (18.3%) had a rolling chair adjustable in height but not in inclination, 20 (21.5%) had a rolling chair adjustable in height and inclination and 12 (12.9%) possessed an ergonomic chair. Most subjects (69, 74.2%) owned a fixed desk, 5 (5.4%) had a height-adjustable desk and 19 (20.4%) declared not to have a specific workstation but to work anywhere without preferences. In terms of digital devices, 80 (86%) utilized a laptop, 11 (11.8%) a desktop and only 2 (2.2%) a tablet. Sixty-five participants (69.9%) considered these devices to be adequate for their working tasks, while the remainder (28, 30.1%) affirmed they were insufficient for their activities. The latter lamented about limited connectivity (4, 12.1%), inadequateness of digital devices (9, 27.3%), deficient sharing software and tools (5, 15.2%) and, most of all, insufficient ergonomic supports (25, 75.8%). As for the role of the employers in supplying the workers with their home office equipment, 45 (48.4%) were provided with digital devices but not with other items (i.e., chair, desk etc.), 10 (10.8%) were provided with both digital devices and furniture, while the remainder (38, 40.8%) declared to have equipped their home office in total autonomy without the support of their employer.
During an average remote working day, participants spent 7.37 ± 2.16 hours sitting and 1.97 ± 1.6 hours standing. Compared to in-person working, participants considered their productivity to be increased (50, 53.8%), decreased (8, 8.6%), or unchanged (35, 37.6%). Similarly, their stress level was increased (32, 34.4%), decreased (32, 34.4%), or unchanged (29, 31.2%). Furthermore, 29 subjects (31.2%) affirmed that their work satisfaction increased, while it decreased in 26 (28%) and remained unchanged in 38 (40.9%).
In terms of advantages of remote working, the most renowned benefit was reduced commuting time (84, 90.4%), followed by higher organizational flexibility (61, 65.6%), increased family time (52, 55.9%), higher autonomy (43, 46.2%), and higher focus while working (32, 34.4%). On the contrary, the main disadvantages were lack of social interactions with colleagues (70, 75.3%), difficulty in separating work and family environments (47, 50.5%), higher distractions within the domestic environment (33, 35.5%), lower involvement in organizational and administrative changes at work (26, 28%), technical issues with digital devices (27, 29%), lower support and interaction with superiors (17, 18.3%), communication problems (18, 19.4%), and activity planning issues (11, 11.8%). The average WHO-5 score was 13.31/25, which is indicative of a nearly poor wellbeing [15], while the average PHQ-2 score was 1.85/6. Additional outcome measures of the psychosocial burden of remote working are summarized in Table 3. When asked if willing to continue with remote working after the pandemic, 48 participants (51.6%) answered âyes, as much as possible,â 31 (33%) âoccasionallyâ and the remainder answered ânoâ due to organizational difficulties (3, 3.2%), increased costs (1, 1.1%), lack of social interaction (5, 5.4%), increased distractions (2, 2.2%) and higher workload (3, 3.2%).
After having started remote working, 54 participants (58.1%) reported a worsening of their LBP and 24 (25.8%) that LBP was unchanged; only 15 (16.1%) affirmed that their LBP improved compared to in-person working. Indeed, LBP severity was significantly higher (5.29 ±2.16) compared to previous in-person working (3.21 ±2.19, p < 0.0001) (Fig. 3) after transitioning to remote working, with an average ORQ of 30.4/100 and an ODI of 22.55/100. While LBP did not cause work absence in 37 subjects (39.8%), 38 (40.9%) were absent for less than 10 days, 15 (16.1%) between 10 and 24 days and 3 (3.2%) between 25 and 99 days.
A multivariate logistic regression model was built to examine the association between worsening of LBP after starting remote working and several independent variables (Table 4). Interestingly, participants who were married/cohabitees (OR, 0.24; 95% CI, 0.07â0.81; p = 0.021) or reported an unchanged job satisfaction (OR, 0.22; 95% CI, 0.08â0.65; p = 0.006) showed a significantly lower risk of LBP deterioration. On the other hand, higher depression scores (OR, 1.38; 95% CI, 1.00â1.91; p = 0.048), an increased stress levels (OR, 3.00; 95% CI, 1.04â8.65; p = 0.042), and being divorced (OR, 4.28; 95% CI, 1.27â14.47; p = 0.019) were associated with a significantly higher risk of LBP worsening.
The COVID-19 pandemic has profoundly reshaped the daily routines of workers throughout the world. To reduce the risk of disease transmission, remote working has been implemented on a global scale across nearly all industry sectors, including governments, educational and information services, business companies and several more [20]. While promoting safety and guaranteeing the continuity of production activities, working from home has also raised significant concerns regarding workersâ performance, health and wellbeing [21]. These aspects may be related to several factors, such as inadequate environmental conditions within the home workspace (lighting, noise, comfort, etc.) [22], decreased concentration due to poor proxemics, lack of social interactions, and several more [23]. In addition, the sedentary lifestyle and physical inactivity imposed by remote working also importantly increase the risk of non-communicable diseases [24] and MSDs, including cLBP [7].
LBP is a multifaceted condition affecting nearly every worker at least once in their life [25,26]. According to the biopsychosocial model, cLBP is determined by the complex interplay between biological factors (intervertebral disc degeneration associated with aging, obesity, overload, etc.) and psychosocial factors, including depression, social isolation, catastrophizing, and misperceptions about the relationship between pain, health, work, and societal obstacles [27].
In this cross-sectional study, we performed a multidimensional evaluation of the interaction between demographic and work-related factors with cLBP in an adult population working from home. We found that the severity of LBP significantly increased after beginning remote working compared to in-person working and was accompanied by an ODI score corresponding to a degree of moderate disability [17], with more than half of participants reporting sick leaves due to LBP. More interestingly, we found that the risk LBP worsening was significantly associated with several factors, including being divorced, depression, and having reported increased stress levels with remote working. Conversely, living with others or reporting unchanged job satisfaction seemed to protect against the risk of LBP deterioration. Thence, the increased severity of LBP in this specific population may be explained by several reasons. Indeed, it is widely accepted that cLBP is more prevalent among office workers and that prolonged sitting (> 7 hours) is directly associated with a higher risk of developing LBP [28]. Due to its sedentary nature and the lack of adequate workplace conditions, remote workers are often affected by LBP [29]. In a study by Matsugaki et al. [30], a positive correlation between telework hours and the risk of LBP was described in workers reporting a poor work environment. Indeed, as per ours and other reports [21,31], home offices often lack good illumination, noise isolation, appropriately sized screens and ergonomically friendly chairs and desks, with a substantial amount of individuals not having a dedicated workstation or even working at shared desks or from their beds.32 The use of adjustable chairs and desks allows to work in a comfortable position and is recommended to reduce the overload on the cervical and lumbar spine, thus reducing the risk of neck pain and LBP [33]. Likewise, having a dedicated workspace that is not intended for other uses reduces the probability of being interrupted by distractions, therefore increasing work productivity and reducing stress [21]. This is particularly important for workers living with others and having young children, which are often required to pause their tasks due to family duties [34]. Therefore, it is not surprising that we found a statistically significant increase of approximately 3 weekly work hours during remote working compared to in-person working in our population. This is in line with the study of Awada et al. [21], who reported a daily increment of approximately 90 minutes per day while working from home. In this report, longer hours were mainly reported by individuals with school age children and that adjusted their work hours to fit their family routine. Remote working is often aggravated by a drastic reduction of social interactions as well, which has been claimed by most participants in this and other studies [21,31]. Indeed, reduced communication with both coworkers and employers has been shown to negatively impact on work productivity, job satisfaction, and stress [21]. Furthermore, the prolonged stay at home may contribute to depressed and anxious feelings [35], with sentiments of loneliness and failure of work expectations, especially in subjects living alone. Notably, these psychosocial traits are widely known to increase the risk of cLBP [36], which may partially explain the increased risk of LBP worsening in divorced workers and in individuals with higher WHO-5 and PHQ-2 scores in our study. On the other hand, remote working is characterized by several advantages that have been advocated by most participants, including reduced commuting time, higher organizational flexibility, increased family time and higher autonomy. Indeed, even if all these factors have not shown a direct link with LBP, they have been associated with reduced stress, increased mental health and wellbeing and, in turn, higher job satisfaction [37]. Collectively, these aspects may support the desire to continue with remote working after the pandemic expressed by > 80% of the study participants. As remote working is increasingly heard to be âhere to stay,â several implementations should be considered to promote remote workersâ mental and physical wellbeing. With regards to workstation equipment, it is mandatory to sensitize employers about the relevance of guaranteeing an appropriate work environment at home by directly supplying workers with the ergonomic supports needed [21], as they usually need to arrange themselves their home office without any logistic or economic support. Daily routines and schedules should be created in order to optimize work hours, dedicate time to physical activity and avoid family-work conflicts [33]. Interactions with coworkers and reports to employers should be encouraged to increase job satisfaction, productivity and engagement [38]. Nevertheless, as also highlighted by our findings, more efforts at the policy level are required to coordinate workplace interventions, measures, and actions within organizations to prevent MSDs with a multidimensional approach [39,40].
This study has some limitations. Firstly, caution should be used in generalizing the results of this study. As the study population is entirely from Italy, it might not be representative of the working population of other countries, despite the homogenous distribution of age, sex, and field of work. Furthermore, while internal validity and compliance with inclusion criteria was guaranteed by direct recruitment of participants by the research team, biases may have been introduced by convenience sampling and the cross-sectional design of the study. Indeed, the lack of determination of causal relationship between variables over different timepoints may further decrease the generalizability of our results.
The COVID-19 pandemic has significantly changed the world of work with a radical shift towards remote tasks without the need to perform in-person workplace activities. However, the sedentary lifestyle, reduced physical activity, poorer workspace conditions and decreased social interactions associated with remote working may also increase the severity of LBP in individuals working from home. In this study, we reported that workers affected by LBP significantly worsened and had increased work hours after starting remote working. Furthermore, the risk of LBP deterioration was associated with being divorced or living with others, higher ill-ness and depression scores, and having reported an unchanged or decreased job satisfaction as well as increased stress levels. Considering the likely integration of remote working in everyday life in the next future, it is essential to plan specific interventions to promote physical and mental wellbeing of remote workers.
Supplementary Material
Supplementary Materials 1 and 2 can be found via https://doi.org/10.14245/ns.2346510.255.
NOTES
Fig. 2.
Study participants reported an increase of average weekly work hours during remote working compared to previous in-person working. ***p<0.001.
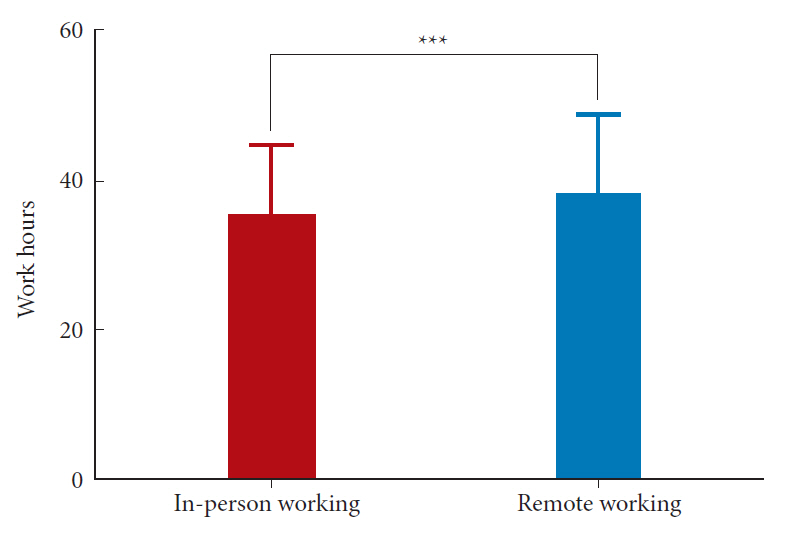
Fig. 3.
Study participants reported an increase of low back pain severity during remote working compared to previous in-person working. VAS, visual analogue scale. ****p<0.0001.
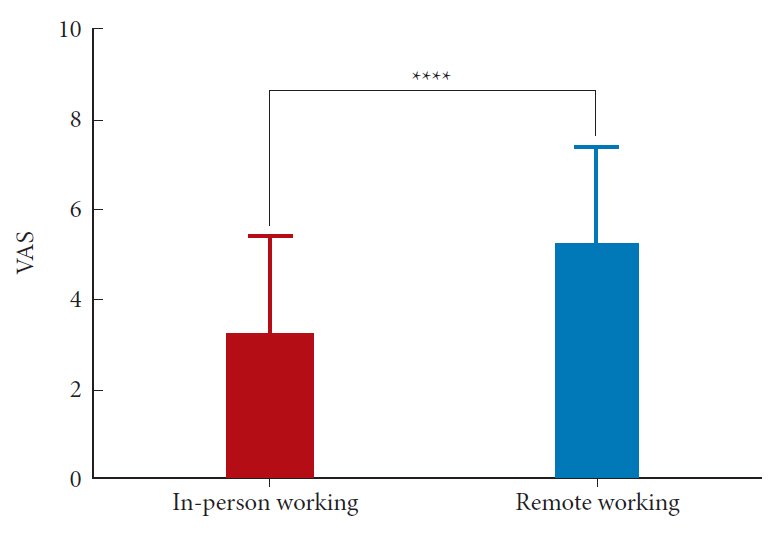
Table 1.
Study population characteristics
Table 2.
Changes of working time during remote working compared to in-person working
Table 3.
Changes of working time during remote working compared to in-person working
Table 4.
Statistically significant associations between low back pain worsening and study variables
REFERENCES
1. World Health Organization. COVID-19 weekly epidemiological update, edition 103, 3 August 2022. Geneva (Switzerland), World Health Organization. 2022;[cited 2022 Aug 10]. Available from: https://apps.who.int/iris/handle/10665/361286.
2. Ambrosio L, VadalĂ G, Russo F, et al. The role of the orthopaedic surgeon in the COVID-19 era: cautions and perspectives. J Exp Orthop 2020;7:35.




3. Park M, Cook AR, Lim JT, et al. A systematic review of COVID-19 epidemiology based on current evidence. J Clin Med 2020;9:967.



4. Eurofound. Telework [Internet]. Dublin (Ireland), Eurofound. 2021;[cited 2022 Aug 10]. Available from: https://www.eurofound.europa.eu/observatories/eurwork/industrial-relations-dictionary/telework.
5. Charalampous M, Grant CA, Tramontano C, et al. Systematically reviewing remote e-workersâ well-being at work: a multidimensional approach. Eur J Work Organ Psychol 2018;28:51-73.

6. Lee IM, Shiroma EJ, Lobelo F, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012;380:219-29.



7. Papalia GF, Petrucci G, Russo F, et al. COVID-19 pandemic increases the impact of low back pain: a systematic review and metanalysis. Int J Environ Res Public Health 2022;19:4599.



9. Olafsson G, Jonsson E, Fritzell P, et al. Cost of low back pain: results from a national register study in Sweden. Eur Spine J 2018;27:2875-81.



10. Russo F, De Salvatore S, Ambrosio L, et al. Does workers' compensation status affect outcomes after lumbar spine surgery? A systematic review and meta-analysis. Int J Environ Res Public Health 2021;18:6165.



11. Cannata F, VadalĂ G, Ambrosio L, et al. Intervertebral disc degeneration: a focus on obesity and type 2 diabetes. Diabetes Metab Res Rev 2020;36:e3224.



12. Vadalaâ G, Russo F, Ambrosio L, et al. Biotechnologies and biomaterials in spine surgery. J Biol Regul Homeost Agents 2015;29(4 Suppl):137-47.
13. VadalĂ G, Russo F, Ambrosio L, et al. Mesenchymal stem cells for intervertebral disc regeneration. J Biol Regul Homeost Agents 2016;30(4 Suppl 1):173-9.
14. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007;370:1453-7.


15. Topp CW, Ăstergaard SD, SĂžndergaard S, et al. The WHO-5 Well-Being Index: a systematic review of the literature. Psychother Psychosom 2015;84:167-76.



16. Li C, Friedman B, Conwell Y, et al. Validity of the Patient Health Questionnaire 2 (PHQ-2) in identifying major depression in older people. J Am Geriatr Soc 2007;55:596-602.


17. Fairbank JC, Pynsent PB. The oswestry disability index. Spine (Phila Pa 1976) 2000;25:2940-52. discussion 2952.


18. Kopec JA, Esdaile JM. Occupational role performance in persons with back pain. Disabil Rehabil 1998;20:373-9.


19. Ostelo RW, de Vet HC. Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol 2005;19:593-607.


20. Gostin LO, Wiley LF. Governmental public health powers during the COVID-19 pandemic: stay-at-home orders, business closures, and travel restrictions. JAMA 2020;323:2137-8.


21. Awada M, Lucas G, Becerik-Gerber B, et al. Working from home during the COVID-19 pandemic: impact on office worker productivity and work experience. Work 2021;69:1171-89.


22. Kang S, Ou D, Mak CM. The impact of indoor environmental quality on work productivity in university open-plan research offices. Build Environ 2017;124:78-89.

23. Kim J, de Dear R. Workspace satisfaction: the privacy-communication trade-off in open-plan offices. J Environ Psychol 2013;36:18-26.

25. Russo F, Di Tecco C, Fontana L, et al. Prevalence of work related musculoskeletal disorders in Italian workers: is there an underestimation of the related occupational risk factors? BMC Musculoskelet Disord 2020;21:738.




26. Russo F, Papalia GF, VadalĂ G, et al. The effects of workplace interventions on low back pain in workers: a systematic review and meta-analysis. Int J Environ Res Public Health 2021;18:12614.



28. Bontrup C, Taylor WR, Fliesser M, et al. Low back pain and its relationship with sitting behaviour among sedentary office workers. Appl Ergon 2019;81:102894.


29. Moretti A, Menna F, Aulicino M, et al. Characterization of home working population during COVID-19 emergency: a cross-sectional analysis. Int J Environ Res Public Health 2020;17:6284.



30. Matsugaki R, Ishimaru T, Hino A, et al. Low back pain and telecommuting in Japan: influence of work environment quality. J Occup Health 2022;64:e12329.



31. Xiao Y, Becerik-Gerber B, Lucas G, et al. Impacts of working from home during COVID-19 pandemic on physical and mental well-being of office workstation users. J Occup Environ Med 2021;63:181-90.


32. van der Lippe T, Lippényi Z. Co-workers working from home and individual and team performance. New Technol Work Employ 2020;35:60-79.



33. Lopez-Leon S, Forero DA, Ruiz-DĂaz P. Recommendations for working from home during the COVID-19 pandemic (and beyond). Work 2020;66:371-5.


34. Toniolo-Barrios M, Pitt L. Mindfulness and the challenges of working from home in times of crisis. Bus Horiz 2021;64:189-97.


35. Wang Y, Kala MP, Jafar TH. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: a systematic review and meta-analysis. PLoS One 2020;15:e0244630.



36. Petrucci G, Papalia GF, Russo F, et al. Psychological approaches for the integrative care of chronic low back pain: a systematic review and metanalysis. Int J Environ Res Public Health 2021;19:60.



37. Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry 2020;7:883-92.



38. Waizenegger L, McKenna B, Cai W, et al. An affordance perspective of team collaboration and enforced working from home during COVID-19. Eur J Inf Sys 2020;29:429-42.

39. Di Tecco C, Ronchetti M, Russo S, et al. Implementing smart working in public administration: a follow up study. Med Lav 2021;112:141-52.


40. Di Tecco C, Ronchetti M, Russo S, et al. Prevention of musculoskeletal disorders and psychosocial risks in the workplace: EU strategies and future challenges [Internet]. Bilbao (Spain), European Agency for Safety and Health at Work. 2022;[cited 2022 Aug 22]. Available from: https://osha.europa.eu/en/publications/prevention-musculoskeletal-disorders-and-psychosocial-risks-workplace-eu-strategies-and-future-challenges.

- TOOLS
- Related articles in NS
-
Journal Impact Factor 3.2