- Search
|
|
||
Abstract
Objective
Spine surgery rates are increasing in the elderly population due to social aging, and it is known that prognoses related to surgery are worse for the elderly compared to younger individuals. However, minimally invasive surgery, such as full endoscopic surgery, is considered safe with low complication rates due to minimal damage to surrounding tissues. In this study, we compared outcomes of transforaminal endoscopic lumbar discectomy (TELD) in elderly and younger patients with disc herniation in the lumbosacral region.
Methods
We retrospectively analyzed the data of 249 patients who underwent TELD at a single center between January 2016 to December 2019, with a minimum follow-up of 3 years. Patients were allocated to 2 groups: a young group aged ≤ 65 years (n = 202) or an elderly group aged > 65 years (n = 47). We evaluated baseline characteristics, clinical outcomes, surgery-related outcomes, radiological outcomes, perioperative complications, and adverse events during the 3-year follow-up period.
Results
Baseline characteristics, including age, general condition based on American Society of Anesthesiologist physical status classification grade, age-Charlson Comorbidity Index, and disc degeneration, were worse in elderly group (p < 0.001). However, except for leg pain at 4 weeks after surgery, overall outcomes, including pain improvement, radiological change, operation time, blood loss, and hospital stay, were not different between the 2 groups. Furthermore, the rates of perioperative complications (9 patients [4.46%] in the young group and 3 patients [6.38%] in the elderly group, p = 0.578) and adverse events over the 3-year follow-up period (32 patients [15.84%] in the young group and 9 patients [19.15%] in the elderly group, p = 0.582) were comparable in the 2 groups.
As the population ages, there is an increasing number of patients with spinal diseases and a corresponding need for spinal surgery [1]. In particular, degenerative lumbar spine diseases are on the rise, leading to a significant increase in the economic burden [2,3]. This trend is the inevitable result of a growing elderly population and the gradual accumulation of age-related degenerative changes in the spine.
In elderly patients, biological age, frailty, and other risk factors identified by prognostic prediction models negatively impact the outcome after surgery [4-6]. The incidence of complications, which exceed 30% in some studies, and recovery time after spinal surgery are worse in the elderly compared to younger individuals [7]. Therefore, physicians should prudently consider the risks and benefits before performing spinal surgery in elderly patients [8].
The comparative clinical outcomes after full endoscopic spine surgery in elderly and younger patients are controversial. Several recent studies have suggested that minimally invasive spine surgery (MISS) reduces postoperative complications and hospital stays compared to conventional surgery, and that MISS may be particularly effective in the elderly [9-12]. In particular, full endoscopic spine surgery, which is performed under local anesthesia or epidural anesthesia, is considered relatively safe as it minimizes damage to surrounding tissues [13,14]. On the other hand, some authors have reported that advanced age is a risk factor for recurrence and reoperation after full endoscopic spine surgery [15-17]. However, there are few direct comparative studies that have examined the efficacy and safety of full endoscopic spine surgery in the elderly and younger adults [13].
To address this controversy, we compared the outcomes of transforaminal endoscopic lumbar discectomy (TELD), a water-based uniportal endoscopic procedure, between elderly and young patients with herniated disc in the lumbosacral region, focusing on complications and adverse events [18]. The criteria used to define the elderly range from 60 to 80 years of age, but 65 is commonly used based on socioeconomic and physical activity considerations [19]. In this study, we used 65 years as the age criterion because it is socially acceptable and in line with recent literature [7,15,20].
The study was approved by the Institutional Review Board of Gachon University Gil Medical Center (GBIRB2023-028), which waived the requirement for informed consent due to the retrospective design of the study and the anonymized nature of the data used.
All patients who underwent surgery were diagnosed with lumbar disc herniation causing leg pain by lumbar magnetic resonance imaging (MRI). The indications for TELD were as follows: (1) persistent back pain and leg pain despite conservative treatment, including medication and/or nerve block, for a minimum of 6 weeks; or (2) extreme pain, making daily life impossible or (3) motor weakness of grade ≤ 3 regardless of conservative treatment duration.
The data of patients that underwent TELD by one of 2 surgeons (SS, AY) at a single institute between January 2016 and December 2019. One surgeon had more than 15 years of experience (>1,000 cases), and the other surgeon had 3 years of experience (>100 cases) [21].
The study exclusion criteria used were as follows: (1) transforaminal endoscopic lumbar foraminotomy or extraforaminal endoscopic lumbar discectomy cases for foraminal stenosis or far lateral disc rupture, (2) history of previous surgery at the same level, (3) insufficient follow-up during the prescribed 3-year period, or (4) inadequate medical or imaging records.
During the study period, 345 patients underwent TELD by the 2 surgeons, and after excluding 96 patients, the remaining 249 were enrolled. These patients were then allocated to a young group (≤ 65 years of age, n = 202) or an elderly group (> 65 years of age, n = 47) (Fig. 1).
All surgical procedures were carried out in the prone position on a Jackson spine table to reduce abdominal pressure. All patients were lightly sedated by an intravenous injection of midazolam, with dosage varying case to case, while vital signs were monitored. After local anesthesia with lidocaine, a skin incision of 0.5 to 0.7 cm in length was made at the surgical level, which was 10 to 15 cm from the midline. The entry points were determined based on anatomical variations and surgical targets.
A discogram was obtained using indigo carmine after inserting a discogram needle into the surgical level under fluoroscopic guidance. The discogram needle was then replaced with a guide wire, and a dilator, an obturator, and a working cannula were sequentially inserted. A Vertebris system (Richard Wolf, Knittlingen, Germany) or a Joimax system (Joimax, Irvine, CA, USA) was used. Foraminoplasty to facilitate cannula approach, removal of ruptured disc, evacuation of the disc space, and annuloplasty/coagulation using radiofrequency were performed on a case-by-case basis under water-based endoscopic view. Finally, the wound was closed with 1−2 stitches of subcutaneous suture and skin tape without drainage [11,22].
Demographic data and baseline characteristics, such as age, sex, body mass index, occupation, smoking status, alcohol intake, surgical level, dominant symptom side, preoperative symptom duration, previous history of nerve block, trauma history, and presence of motor weakness, were analyzed. In addition, general patient conditions were assessed using American Society of Anesthesiologist (ASA) physical status (PS) classification grades and age-Charlson Comorbidity Index (age-CCI) [23,24].
Clinical outcomes were assessed using visual analogue scale (VAS) scores for low back pain and leg pain. Clinical data were collected preoperatively and at each follow-up visit (4 weeks ± 1 week, 1 year ± 1 month, and 3 years ± 3 months after surgery). Patient satisfaction was estimated using Odom criteria at each follow-up visit [25].
Radiological outcomes were obtained from MRI and simple radiography. Lumbar MRI was performed before and immediately after surgery in all patients to confirm nerve root decompression and determine remnant ruptured disc volumes. Plain and dynamic radiographs were performed preoperatively and at 3 years postoperatively to evaluate changes in disc height and lumbar alignment.
Baseline Pfirrmann grade, which represents disc degeneration, and the type of disc rupture (migrated or subligamentous) were evaluated using preoperative MRI [26]. The estimated extruded disc volume was determined using the formula transverse diameter × depth × height of herniated disc 2
Calibrated disc height was measured by averaging the anterior, middle, and posterior disc heights. Then, the disc height ratio to anteroposterior diameter of the L5 vertebral body was determined, considering variations in x-ray magnification, using the formula anterior disc height + middle disc hegith + posterior disc height ( mm ) 3 anteroposterior diameter of L 5 body ( mm ) × 100 %
Surgery-related outcomes were evaluated using the total operation time, blood loss during surgery as assessed by changes in hemoglobin levels post-surgery, and recovery time based on hospital stays. The total operation time was calculated by adding preparation time (time for positioning the patient and preparing the surgical site) and operation time from skin incision to wound closure. Hemoglobin levels were checked prior to the surgery and on the day after to assess changes.
Perioperative complications and adverse events during the 3-year study period were thoroughly investigated. Perioperative complications included surgery-related complications (e.g., exiting root irritation/injury, durotomy, nerve damage, and surgical site infection), non–surgery-related complications (e.g., cardiopulmonary complications, deep vein thrombosis, and urinary retention), and surgical failure and conversion to another surgical method. Adverse events during follow-up included additional admission for care, additional nerve block for pain control, remnant lesion detected postoperative MRI requiring additional treatment, recurrence in the same lesion site, revision surgery for the same lesion, and revision surgery for another lesion.
Data management and statistical analysis were conducted using IBM SPSS Statistics ver. 27.0 (IBM Co., Armonk, NY, USA). Pearson chi-square test, Fisher exact test, the nonparametric Mann-Whitney U-test, the nonparametric Friedman test, the independent t-test, the paired t-test, or Kaplan-Meier survival analysis were used according to the characteristic of the values. Results are presented as means ± standard deviations, means with 95% confidence intervals (CIs), or medians and interquartile ranges (IQR) depending on whether data were normally distributed. Statistical significance was determined at a p-value of less than 0.05.
The mean age of overall population was 51.72 ± 15.87 years with normal distribution. The median ages in the young and elderly groups were 49 (IQR, 37.00−58.00) and 72.00 (IQR, 67.25−79.75), respectively (p < 0.001, nonparametric Mann-Whitney U-test) (Fig. 2).
The ASA PS classification grade and age-CCI were significantly higher in the elderly group (p < 0.001, by Pearson chi-square test and the nonparametric Mann-Whitney U-test, respectively). The occupational distribution among the patients revealed a significant proportion of retired individuals in the elderly group, which was different from the distribution in the young group (p < 0.001, Pearson chi-square test). Notably, the elderly group had a relatively high proportion of patients above the L4−5 level of surgery, which was also significantly different from the young group (p < 0.001, Pearson chi-square test).
Other factors, including sex ratio, smoking, alcohol intake, duration of symptoms, dominant symptom side, trauma history, and presence of paresis, were not different between the 2 groups. Additionally, body mass index was not significantly different between the 2 groups, although height and weight were greater in the young group (Table 1).
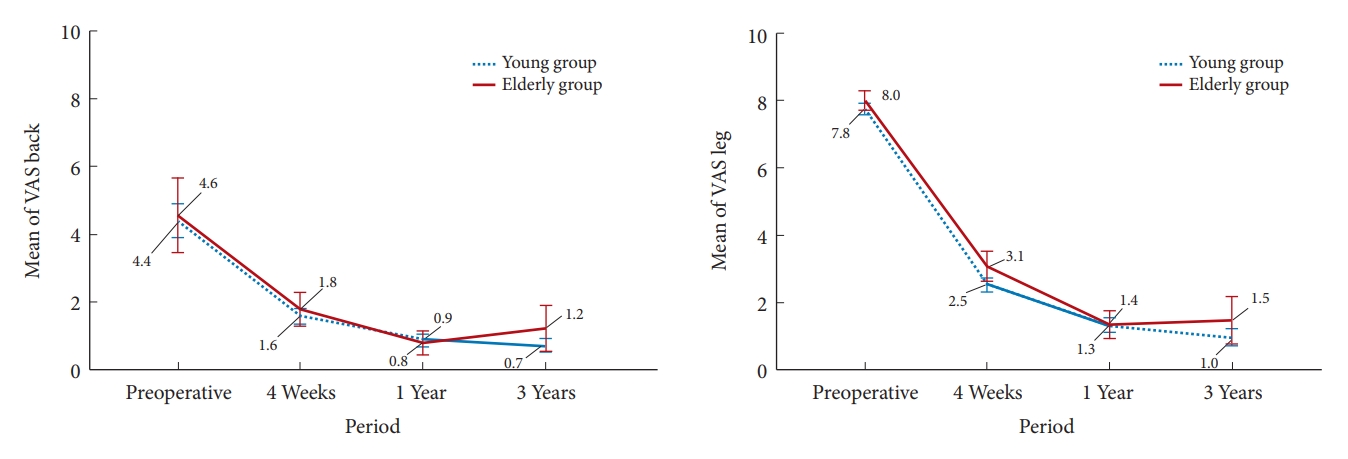
Longitudinal analysis of both groups showed that the VAS scores for back and leg pain significantly improved after surgery, and that pain reduced progressively during the 3-year follow-up (p < 0.001, nonparametric Friedman test) (Fig. 3).
Comparative analysis revealed that median VAS scores for back pain were similar in the 2 groups across all survey periods, and that median VAS scores for leg pain were not different between the 2 groups before surgery and at 1- and 3-year follow-up visits. However, at 4 weeks after surgery, the young group showed greater improvement in VAS scores for leg pain than the elderly group (median [IQR]: 2.0 [2.0–3.0] vs. 3.0 [2.0–4.0], p = 0.012, nonparametric Mann-Whitney U-test) (Table 2).
According to Odom criteria, both groups showed favorable satisfaction, with success rates above 90%, and no intergroup difference was evident at any follow-up visit (Table 2).
The degree of preoperative disc degeneration at the surgical level, as determined by Pfirrmann grade, was more severe in the elderly group (p = 0.013, Pearson chi-square test). However, types of disc extrusion were similar as determined by preoperative MRI. Additionally, the reduction ratio of the extruded disc was not significantly different between the 2 groups (median [IQR], 73.92% [56.72%−86.69%] in the young group and 69.34% [58.39%−80.18%] in the elderly group, p = 0.301, nonparametric Mann-Whitney U-test) (Table 3).
Longitudinal analysis of simple radiographs showed that disc height ratio to vertebral body was significantly smaller in both groups at 3 years after surgery compared to preoperative values (from 27.46% ± 8.93% to 26.84% ± 9.91% in the young group and from 27.22% ± 6.15% to 26.07% ± 6.08% in the elderly group, p < 0.001, paired t-test). Lumbar lordosis also significantly increased in both groups at 3 years after surgery (from 38.91° ± 14.65° to 43.20° ± 11.05° in the young group and from 40.00° ± 12.53° to 43.70° ± 12.16° in the elderly group, p < 0.001 and p = 0.011 respectively, paired t-test). However, comparative analysis showed that preoperative and 3-year postoperative changes were not significantly different (Table 3).
In terms of the surgical procedure, there was no difference in the rate of performing bone work, such as foraminoplasty, partial pediculectomy, or partial endplate drilling, between the 2 groups. In addition, the total operation time, including preparation and operation time, was not different between the 2 groups (median [IQR], 75.0 minutes [65.0−85.0 minutes] in the young group and median 75.0 minutes [65.0−80.0 minutes] in the elderly group, p = 0.738, nonparametric Mann-Whitney U-test) (Table 4).
The reduction in hemoglobin level, indicating intraoperative blood loss, was not different between the 2 groups (median [IQR], 0.60 [0.30−1.00] in the young group and median 0.70 [0.30−0.90] in the elderly group, p = 0.596, nonparametric Mann-Whitney U-test), although pre- and postoperative hemoglobin levels were significantly lower in the elderly group (Table 4).
Hospital stay was also not significantly different between the 2 groups (median [IQR], 4.0 days [3.0−6.0 days] in both groups, p = 0.927, nonparametric Mann-Whitney U-test) (Table 4).
The incidence of perioperative complications was not significantly different between the 2 groups (9 patients [4.46%] in young group versus 3 patients [6.38%] in elderly group, p = 0.578, Pearson chi-square test). In the young group, 8 patients (3.96%) experienced surgery-related complications, including 4 cases of transient exiting root irritation, 2 cases of iatrogenic durotomy, 1 case of surgical site infection with discitis, and 1 case of new disc herniation in the foramen along the endoscope trajectory. In the elderly group, 2 patients (4.26%) experienced surgery-related complications, including 1 case of iatrogenic durotomy and 1 case of surgical site infection with discitis. In terms of nonsurgery-related complications, there was one patient in the elderly group who was newly diagnosed with arterial insufficiency after surgery. Additionally, there was one case of conversion to open surgery in the young group because of intradural disc rupture (Table 5).
The number of patients who experienced an adverse event during follow-up was similar between the 2 groups (32 patients [15.84%] in the young group vs. 9 patients [19.15%] in the elderly group, p = 0.582, Pearson chi-square test). Significant residual extruded discs requiring further treatment occurred in 2 patients (1.00%) in the young group and 1 patient (2.13%) in the elderly group (p = 0.468, Fisher exact test). Recurrent disc herniation with symptom aggravation occurred in 14 patients (6.93%) in the young group and 5 patients (10.64%) in the elderly group (p = 0.394, Pearson chi-square test). Revision surgery for the previously treated lesion was performed in 17 patients (8.42%) in the young group (5 cases of revisional TELD for recurrence, 4 cases of revisional microscopic discectomy for recurrence, 3 cases of fusion surgery for recurrence, 3 cases of microscopic discectomy for remnant lesion, 1 case of fusion for iatrogenic durotomy, and 1 case of revisional TELD for discitis) and 7 patients (14.89%) in the elderly group (3 cases of revisional microscopic discectomy for recurrence, 1 case of revisional TELD for recurrence, 1 case of revisional TELD for remnant lesion, 1 case of fusion surgery for recurrence, and 1 case of fusion surgery for discitis) (p=0.175, Pearson chi-square test). In addition, surgery for another lesion was performed in 3 patients (1.49%) in the young group (1 case of disc herniation in the contralateral side at 1 month after surgery, and 2 cases of disc herniation at an adjacent cranial level at 2 and 3 months after surgery, whereas no surgery for another lesion was performed in the elderly group) (p = 1.000, Fisher exact test) (Table 5).
No overall significant intergroup difference was observed for any complication or adverse event (37 patients [18.32%] in the young group versus 10 patients [21.28%] in the elderly group, p = 0.640, Pearson chi-square test). According to Kaplan-Meier survival analysis of all perioperative complications and adverse events during the 3-year follow-up period, the mean time to occurrence of an event was similar between the 2 groups (908.3 days [95% CI, 853.1−963.4] in the young group and 911.7 days [95% CI, 800.2−1,023.3] in the elderly group, p = 0.682, log-rank test) (Fig. 4).
On the other hand, regarding age as a risk factor for recurrence after TELD, the mean age of the recurrence group (n = 19) was higher compared to the nonrecurrence group (n = 230), but the difference was not statistically significant (mean age of 51.30 ± 16.09 years in the nonrecurrence group and 56.84 ± 12.18 years in the recurrence group, p = 0.144, independent t-test). There was also no difference between the event-occurred group (n = 202) and non–event-occurred group (n = 47) in terms of age as a risk factor for overall complications and adverse events (mean age of 51.71 ± 15.77 years in the event-occurred group and 51.74 ± 16.46 years in the non–event-occurred group, p = 0.990, independent t-test).
According to the results of this study, overall outcomes, including clinical and radiological outcomes, perioperative complications, and adverse events, were comparable in both the elderly group (age > 65 years) and the young group. As expected, several baseline characteristics, such as baseline general condition (based on ASA PS classification grade and age-CCI), basic physique (based on height and weight), hemoglobin level, and degenerative disc changes, were significantly worse in the elderly group. Baseline general condition and age are known to be associated with postoperative prognosis [28,29], and disc degeneration has known to be associated with recurrence [30,31]. However, clinical and radiological outcomes were not significantly different between the 2 groups, except for VAS leg pain at 4 weeks after surgery. Additionally, both groups showed similar outcomes in terms of recovery rates, based on the length of hospital stay and incidences of perioperative complications and adverse events during the 3-year follow-up period.
These findings of the present study are not consistent with previous suggestions that the elderly have a higher probability of experiencing adverse events after undergoing full endoscopic surgery. A previous study based on a nationwide database suggested that the cutoff age for endoscopic surgery was 57 years because the risk of reoperation after this age increased more than that of open surgery [14,15]. In addition, others have suggested that patients with a mean age between 52.1 to 68.5 years have higher rates of recurrence, reoperation, or readmission after endoscopic surgery compared to younger patients [16,32].
We postulate several hypotheses for the discrepancy of results between this study and previous reports. First, the difference of statistical methods can affect the conclusion. We directly compared the young and elderly groups, whereas previous studies compared the event-occurred group and non–event-occurred group. However, in this study, comparison between the recurrence group and the nonrecurrence group also showed no statistical difference in terms of age, although there was a trend that the recurrence group had an older age compared to the nonrecurrence group. Secondly, fundamental difference in collected data, such as surgical approach or follow-up period, can affect the overall results of the analysis. To validate our results, large-scaled studies or prospective studies are necessary.
Full endoscopic surgery has several advantages over conventional spine surgery, which includes local anesthesia, a smaller incision, less blood loss, and a shorter recovery time [33]. MISS techniques have rapidly improved over the past 2 decades, and one of the most advanced MISS techniques for patients with lumbar disc herniation is TELD [12]. TELD minimizes damage to surrounding structures and does not require general anesthesia [12,34]. Several authors have reported that TELD is superior to conventional surgery, including microscopic discectomy, in terms of outcomes and complication rates [34,35]. Based on this concept, many authors have suggested that MISS might be more beneficial than conventional surgery in the elderly, and full endoscopic surgery could be applied safely in elderly patients [7,34,36,37]. Previous studies have shown that the overall results of full endoscopic surgery in patients aged over 70 were favorable [13].
Despite the several advantages of TELD, its application in the elderly has several limitations. For example, the surgical approach is more challenging in elderly patients, and greater surgical proficiency is often required because of degenerative changes such as facet joint hypertrophy or reduced disc height [38]. The indications for TELD in elderly patients are also more restrictive because of advanced pathologic conditions, such as severe central stenosis, calcified discs, spondylolisthesis, or sagittal imbalance [39]. Nevertheless, based on our findings, there was no difference in baseline disc height, although the preoperative disc degeneration was different. This phenomenon could be caused by the patient selection process for TELD. As a result, TELD could be an excellent option in elderly patients, given sufficient surgical proficiency and proper patient selection.
The present study has several limitations that need to be considered. Firstly, the retrospective design of the study did not allow for objective comparisons between the 2 study groups. However, the study included a relatively large number of patients with a minimum 3-year follow-up period, which provided statistical reliability. Secondly, surgeries were performed by different surgeons, and the analysis was not controlled for confounders. However, we attempted to minimize selection bias by adopting strict exclusion criteria. Nonetheless, this study is the first to compare the outcomes of TELD for young and elderly patients to the best of our knowledge.
The overall outcomes, including occurrence of complication/adverse events, were not significantly different between young and elderly groups. These findings indicate that the clinical efficacy and safety of TELD in elderly patients (> 65 years) are comparable to younger patients. Additionally, full endoscopic spine surgery has relatively good risk-benefits compared to conventional surgeries requiring general anesthesia. We hope that this study will serve as a reference for surgeons considering TELD in the elderly population.
NOTES
Fig. 1.
The patient selection process. TELD, transforaminal endoscopic lumbar discectomy; EELD, extraforaminal endoscopic lumbar discectomy; TELF, transforaminal endoscopic lumbar foraminotomy.
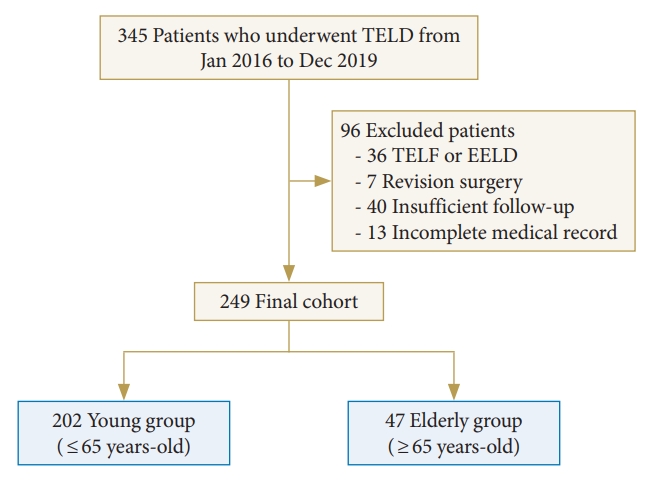
Fig. 4.
Kaplan-Meier survival analysis for perioperative complications and adverse events during the 3-year follow-up period in the 2 groups.
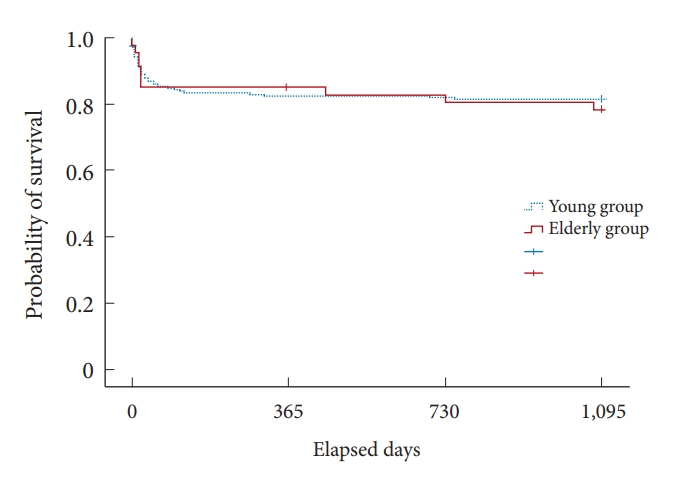
Table 1.
Baseline characteristics
| Characteristic | Young (n = 202) | Elderly (n = 47) | p-value |
|---|---|---|---|
| Age (yr) | 49.00 (37.00−58.00) | 72.00 (67.25−79.75) | < 0.001† |
| Sex, male:female | 107:95 | 25:22 | 0.978‡ |
| Height (cm) | 167.62 ± 9.38 | 161.01 ± 9.76 | < 0.001§ |
| Weight (kg) | 66.00 (59.55–75.00) | 60.70 (53.15–70.25) | 0.003† |
| Body mass index (kg/m2) | 23.57 (21.63–26.00) | 23.34 (21.46–26.25) | 0.504† |
| Occupation | |||
| White collar:blue collar:others | 86:46:70 | 10:6:31 | < 0.001‡ |
| Smoking | |||
| Yes:no | 28:174 | 4:43 | 0.324‡ |
| Alcohol | |||
| Yes:no | 71:131 | 17:30 | 0.895‡ |
| Surgery level | |||
| L2–3:L3–4:L4–5:L5–S1 | 0:10:147:45 | 1:13:26:7 | < 0.001‡ |
| Dominant symptom side | |||
| Right:left:equivocal | 89:107:6 | 17:30:0 | 0.241‡ |
| Symptom duration (wk) | 8.57 (3.00–25.71) | 12.86 (3.32–51.43) | 0.428† |
| Previous nerve block | |||
| Yes:no | 128 (63.4):74 | 28 (59.6):19 | 0.663‡ |
| Trauma | |||
| Yes:no | 15 (7.4):187 | 2 (4.3):45 | 0.433‡ |
| Weakness | |||
| Yes:no | 31 (15.4):171 | 8 (17.0):39 | 0.776‡ |
| ASA PS classification grade | |||
| I:II:III:IV | 102:82:18:0 | 2:30:15:0 | < 0.001‡ |
| Age-CCI | 1.0 (0.0–3.0) | 4.0 (3.0–5.0) | < 0.001† |
| Surgeon | |||
| A:B | 140:62 | 38:9 | 0.114‡ |
Table 2.
Clinical outcomes
| Variable | Young (n = 202) | Elderly (n = 47) | p-value |
|---|---|---|---|
| VAS back | |||
| Preoperative | 6.0 (0.0−8.0) | 6.5 (0.0−8.0) | 0.670† |
| 4 Weeks | 2.0 (0.0−2.0) | 2.0 (0.0−2.75) | 0.468† |
| 1 Year | 0.0 (0.0−1.0) | 0.0 (0.0−1.0) | 0.791† |
| 3 Years | 0.0 (0.0−1.0) | 0.0 (0.0−1.75)§ | 0.762† |
| VAS leg | |||
| Preoperative | 8.0 (7.0−9.0) | 8.0 (7.0−9.0) | 0.253† |
| 4 Weeks | 2.0 (2.0–3.0) | 3.0 (2.0–4.0) | 0.012† |
| 1 Year | 1.0 (0.0−2.0) | 1.0 (0.0−2.0) | 0.925† |
| 3 Years | 0.0 (0.0−1.0)§ | 1.0 (0.0−2.0)§ | 0.292† |
| Odom’s criteria: excellent:good:faire:poor | |||
| 4 Weeks with success rate | 91:100:10:1 (94.6) | 13:31:3:0 (93.6) | 0.175‡ |
| 1 Year with success rate | 160:32:9:1 (95.0) | 33:13:1:0 (93.9) | 0.172‡ |
| 3 Years with success rate | 154:37:10:1 (94.6) | 30:13:3:1 (91.5) | 0.206‡ |
Table 3.
Radiological outcomes
| Variable | Young (n = 202) | Elderly (n = 47) | p-value |
|---|---|---|---|
| Pfirrmann grade | 0.013† | ||
| III:IV:V | 70:126:6 | 5:41:1 | |
| Type of ruptured disc | 0.875† | ||
| Migrated:subligamentous | 146:56 | 35:12 | |
| Ruptured disc volume | |||
| Preoperative (mm3) | 1,595.58 (926.49−2,476.69) | 1,278.43 (882.20−2,125.31) | 0.135‡ |
| Postoperative (mm3) | 361.73 (227.72−526.68) | 439.50 (192.82−548.56) | 0.504‡ |
| Reduction ratio (%) | 73.92 (56.72−86.69) | 69.34 (58.39−80.18) | 0.301‡ |
| Disc height ratio to vertebral body (%) | |||
| Preoperative | 27.46 ± 8.93 | 27.22 ± 6.15 | 0.891§ |
| 3 Years | 26.84 ± 9.91 | 26.07 ± 6.08 | 0.431§ |
| Segmental angle of surgery level (°) | |||
| Preoperative | 13.61 ± 7.75 | 14.83 ± 6.55 | 0.417§ |
| 3 Years | 14.70 ± 6.26 | 16.14 ± 6.53 | 0.273§ |
| Range of motion of surgery level (°) | |||
| Preoperative | 3.82 ± 1.67 | 4.49 ± 1.91 | 0.473§ |
| 3 Years | 3.99 ± 1.57 | 3.58 ± 1.74 | 0.664§ |
| Lumbar lordosis (°) | |||
| Preoperative | 38.91 ± 14.65 | 40.00 ± 12.53 | 0.704§ |
| 3 Years | 43.20 ± 11.05 | 43.70 ± 12.16 | 0.833§ |
| Range of motion of lumbar spine (°) | |||
| Preoperative | 19.63 ± 5.66 | 21.75 ± 5.79 | 0.382§ |
| 3 Years | 21.27 ± 5.91 | 22.10 ± 6.03 | 0.125§ |
Table 4.
Surgery-related outcomes
| Variable | Young (n = 202) | Elderly (n = 47) | p-value |
|---|---|---|---|
| Bone work during surgery | |||
| Yes:no | 36 (17.8):166 | 7 (14.9):40 | 0.632† |
| Operation time (min) | |||
| Preparation time | 20.0 (15.0−25.0) | 20.0 (15.0−20.0) | 0.651‡ |
| Operation time | 55.0 (45.0−60.0) | 55.0 (50.0−60.0) | 0.352‡ |
| Total operation time | 75.0 (65.0−85.0) | 75.0 (65.0−80.0) | 0.738‡ |
| Hemoglobin (g/dL) | |||
| Preoperative hemoglobin | 14.22 ± 1.58 | 13.27 ± 1.60 | < 0.001§ |
| Postoperative hemoglobin | 13.52 ± 1.55 | 12.63 ± 1.56 | < 0.001§ |
| Decrease of hemoglobin | 0.60 (0.30−1.00) | 0.70 (0.30−0.90) | 0.596‡ |
| Hospital stay (day) | 4.0 (3.0−6.0) | 4.0 (3.0−6.0) | 0.927‡ |
Table 5.
Perioperative complication and adverse event during follow-up
| Variable | Young (n = 202) | Elderly (n = 47) | p-value |
|---|---|---|---|
| Perioperative complication | |||
| Surgery-related | 8 (3.96) | 2 (4.26) | 0.926† |
| Nonsurgery-related | 0 (0) | 1 (2.13) | 0.189‡ |
| Conversion to open surgery | 1 (0.50) | 0 (0) | 1.000‡ |
| No. of patients who experienced any complication | 9 (4.46) | 3 (6.38) | 0.578† |
| Adverse events | |||
| Additional admission and conservative treatment | 3 (1.49) | 1 (2.13) | 0.569‡ |
| Additional nerve block | 10 (4.95) | 2 (4.26) | 0.841‡ |
| Remnant lesion | 3 (1.49) | 1 (2.13) | 0.468‡ |
| Recurrence | 14 (6.93) | 5 (10.64) | 0.394† |
| Revision surgery of previous lesion | 17 (8.42) | 7 (14.89) | 0.175† |
| Revision surgery of another lesion | 3 (1.49) | 0 (0) | 1.000‡ |
| Number of patients who experienced any adverse event | 32 (15.84) | 9 (19.15) | 0.582† |
| Sum of patients with any complication or adverse event | 37 (18.32) | 10 (21.28) | 0.640† |
REFERENCES
1. Morris K, Nami M, Bolanos JF, et al. Neuroscience20 (BRAIN20, SPINE20, and MENTAL20) Health Initiative: a global consortium addressing the human and economic burden of brain, spine, and mental disorders through neurotech innovations and policies. J Alzheimers Dis 2021;83:1563-601.


2. Deng H, Yue JK, Ordaz A, et al. Elective lumbar fusion in the United States: national trends in inpatient complications and cost from 2002-2014. J Neurosurg Sci 2021;65:503-12.


3. Lee CH, Chung CK, Kim CH, et al. Health care burden of spinal diseases in the Republic of Korea: analysis of a nationwide database from 2012 through 2016. Neurospine 2018;15:66-76.




4. Makary MA, Segev DL, Pronovost PJ, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg 2010;210:901-8.


5. Tan JY, Kaliya-Perumal AK, Oh JY. Is spinal surgery safe for elderly patients aged 80 and above? Predictors of mortality and morbidity in an asian population. Neurospine 2019;16:764-9.




6. Jang HJ, Chin DK, Park JY, et al. Influence of frailty on life expectancy in octogenarians after lumbar spine surgery. Neurospine 2021;18:303-10.




8. Umekawa M, Takai K, Taniguchi M. Complications of spine surgery in elderly Japanese patients: implications for future of world population aging. Neurospine 2019;16:780-8.




9. Goh GS, Tay YWA, Liow MHL, et al. Elderly patients undergoing minimally invasive transforaminal lumbar interbody fusion may have similar clinical outcomes, perioperative complications, and fusion rates as their younger counterparts. Clin Orthop Relat Res 2020;478:822-32.



10. Liu G, Liu S, Zuo YZ, et al. Recent advances in technique and clinical outcomes of minimally invasive spine surgery in adult scoliosis. Chin Med J (Engl) 2017;130:2608-15.



11. Song SK, Son S, Choi SW, et al. Comparison of the outcomes of percutaneous endoscopic interlaminar lumbar discectomy and open lumbar microdiscectomy at the L5-S1 level. Pain Physician 2021;24:E467-75.

12. Son S, Yoo BR, Lee SG, et al. Full-endoscopic versus minimally invasive lumbar interbody fusion for lumbar degenerative diseases: a systematic review and meta-analysis. J Korean Neurosurg Soc 2022;65:539-48.




13. Kim JH, Kim HS, Kapoor A, et al. Feasibility of full endoscopic spine surgery in patients over the age of 70 years with degenerative lumbar spine disease. Neurospine 2018;15:131-7.




14. Casper DS, Rihn JA. Preoperative risk stratification: who needs medical consultation? Spine (Phila Pa 1976) 2020;45:860-1.

15. Kim CH, Chung CK, Choi Y, et al. The selection of open or percutaneous endoscopic lumbar discectomy according to an age cut-off point: nationwide cohort study. Spine (Phila Pa 1976) 2015;40:E1063-70.

16. Wang A, Si F, Wang T, et al. Early readmission and reoperation after percutaneous transforaminal endoscopic decompression for degenerative lumbar spinal stenosis: incidence and risk factors. Risk Manag Healthc Policy 2022;15:2233-42.




17. Yin S, Du H, Yang W, et al. Prevalence of recurrent herniation following percutaneous endoscopic lumbar discectomy: a meta-analysis. Pain Physician 2018;21:337-50.

18. Hofstetter CP, Ahn Y, Choi G, et al. AOSpine consensus paper on nomenclature for working-channel endoscopic spinal procedures. Global Spine J 2020;10(2 Suppl):111S-121S.




19. Wichmann F, Pischke CR, Jürgens D, et al. Requirements for (web-based) physical activity interventions targeting adults above the age of 65years - qualitative results regarding acceptance and needs of participants and non-participants. BMC Public Health 2020;20:907.




20. Singh S, Bajorek B. Defining 'elderly' in clinical practice guidelines for pharmacotherapy. Pharm Pract (Granada) 2014;12:489.



21. Ahn Y, Lee S, Son S, et al. Learning curve for interlaminar endoscopic lumbar discectomy: a systematic review. World Neurosurg 2021;150:93-100.


22. Son S, Ahn Y, Lee SG, et al. Learning curve of percutaneous endoscopic transforaminal lumbar discectomy by a single surgeon. Medicine (Baltimore) 2021;100:e24346.



23. Mayhew D, Mendonca V, Murthy BVS. A review of ASA physical status - historical perspectives and modern developments. Anaesthesia 2019;74:373-9.



24. Charlson ME, Carrozzino D, Guidi J, et al. Charlson comorbidity index: a critical review of clinimetric properties. Psychother Psychosom 2022;91:8-35.



25. Broekema AEH, Molenberg R, Kuijlen JMA, et al. The Odom criteria: validated at last: a clinimetric evaluation in cervical spine surgery. J Bone Joint Surg Am 2019;101:1301-8.

26. Pfirrmann CW, Metzdorf A, Zanetti M, et al. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976) 2001;26:1873-8.


27. Son S, Lee SG, Kim WK, et al. Disc height discrepancy between supine and standing positions as a screening metric for discogenic back pain in patients with disc degeneration. Spine J 2021;21:71-9.


28. Shin JI, Kothari P, Phan K, et al. Frailty index as a predictor of adverse postoperative outcomes in patients undergoing cervical spinal fusion. Spine (Phila Pa 1976) 2017;42:304-10.


29. Flexman AM, Charest-Morin R, Stobart L, et al. Frailty and postoperative outcomes in patients undergoing surgery for degenerative spine disease. Spine J 2016;16:1315-23.


30. Brooks M, Dower A, Abdul Jalil MF, et al. Radiological predictors of recurrent lumbar disc herniation: a systematic review and meta-analysis. J Neurosurg Spine 2020;34:481-91.


31. Sayin Gülensoy E, Gülensoy B. A 9-year retrospective cohort of patients with lumbar disc herniation: comparison of patient characteristics and recurrence frequency by smoking status. Medicine (Baltimore) 2022;101:e32462.



32. Zhao C, Zhang H, Wang Y, et al. Nomograms for predicting recurrent herniation in PETD with preoperative radiological factors. J Pain Res 2021;14:2095-109.




33. Wei FL, Zhou CP, Zhu KL, et al. Comparison of different operative approaches for lumbar disc herniation: a network meta-analysis and systematic review. Pain Physician 2021;24:E381-92.

34. Xu X, Chen C, Tang Y, et al. Clinical efficacy and safety of percutaneous spinal endoscopy versus traditional open surgery for lumbar disc herniation: systematic review and meta-analysis. J Healthc Eng 2022;2022:6033989.




35. Yang CC, Chen CM, Lin MH, et al. Complications of full-endoscopic lumbar discectomy versus open lumbar microdiscectomy: a systematic review and meta-analysis. World Neurosurg 2022;168:333-48.


36. Perez-Roman RJ, Gaztanaga W, Lu VM, et al. Endoscopic decompression for the treatment of lumbar spinal stenosis: an updated systematic review and meta-analysis. J Neurosurg Spine 2021;36:549-57.


37. Gadjradj PS, Harhangi BS. Full-endoscopic transforaminal discectomy versus open microdiscectomy for sciatica: update of a systematic review and meta-analysis. Spine (Phila Pa 1976) 2022;47:E591-4.