 |
 |
- Search
|
|
||
Abstract
Objective
Methods
Results
Conclusion
NOTES
Funding/Support
This work was sponsored by Army Medical University Outstanding Talent Pool Key Support Object Personalized Training Project (No. 2019rcpy05) and Chongqing Talent Program: CQYC202105037.
Author Contribution
Conceptualization: FL, JZX, ZRZ, ZHZ; Data curation: HL, YSY, JHZ, YG, HC, FL; Formal analysis: HL, YSY, ZHZ; Funding acquisition: ZRZ, ZHZ; Methodology: JZX; Project administration: FL, JZX, ZRZ, ZHZ; Visualization: JZX, ZRZ, ZHZ; Writing - original draft: HL; Writing - review & editing: JZX, ZRZ, ZHZ.
ACKNOWLEDGEMENTS
Fig. 1.

Fig. 2.
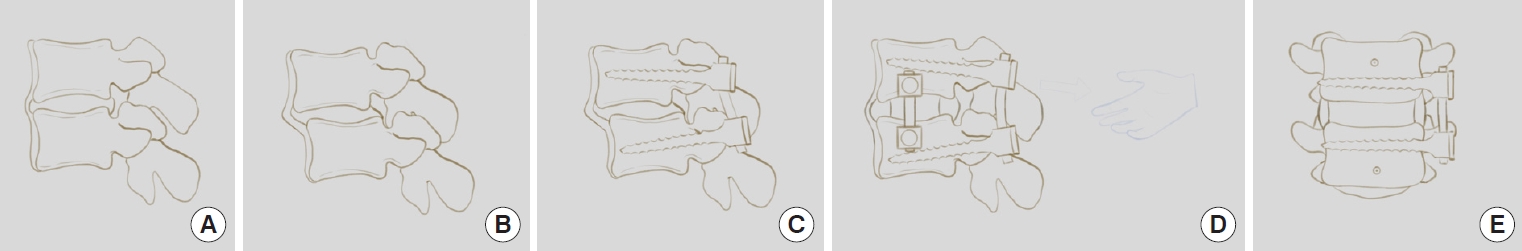
Fig. 3.
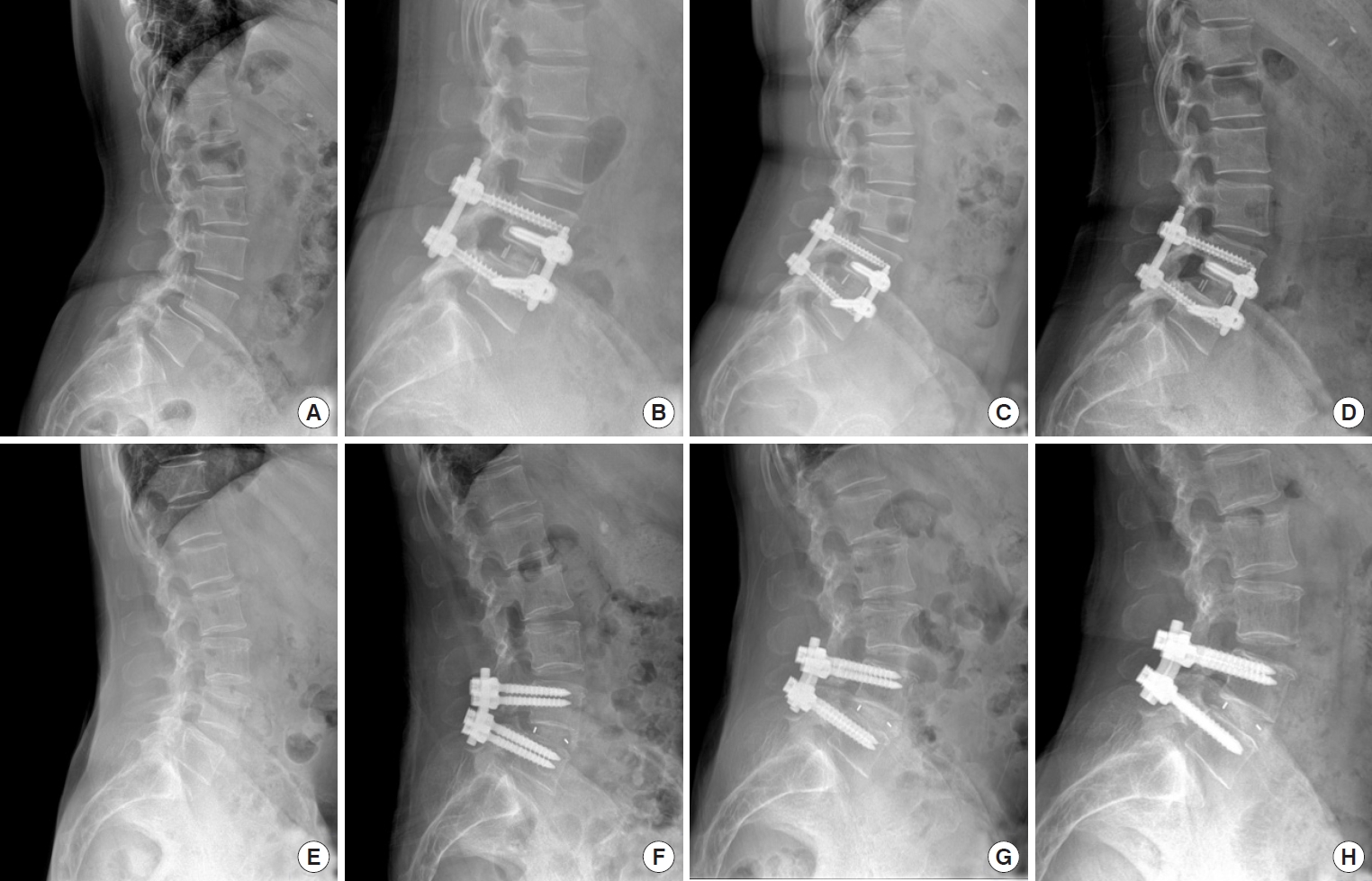
Table 1.
Values are presented as mean±standard deviation or number (%).
MIS-TLIF-BPS, minimally invasive transforaminal lumbar interbody fusion with bilateral pedicle screw; LLIF-LSUP, lateral lumbar interbody fusion combined lateral single screw-rod and unilateral percutaneous pedicle screw fixation; BMI, body mass index; BMD, bone mineral density.
Table 2.
| Variable | MIS-TLIF- BPS (n = 36) | LLIF-LSUP (n = 26) | p-value | t/χ2 |
|---|---|---|---|---|
| Operative duration (min) | 140.3 ± 27.6 | 100.5 ± 13.3 | 0.000* | 6.799 |
| Blood loss (mL) | 244.7 ± 101.1 | 68.8 ± 18.6 | 0.000* | 8.748 |
| Length of hospital stay (day) | 9.2 ± 2.1 | 6.1 ± 1.9 | 0.000* | 5.997 |
| VAS | ||||
| Pre | 6.8 ± 1.5 | 6.5 ± 1.2 | 0.629 | 0.486 |
| 3 Months | 2.5 ± 0.8 | 1.8 ± 0.6 | 0.000* | 3.606 |
| 6 Months | 2.0 ± 0.6 | 1.6 ± 0.5 | 0.001* | 3.426 |
| 9 Months | 1.8 ± 0.4 | 1.6 ± 0.4 | 0.101 | 1.667 |
| 12 Months | 1.7 ± 0.5 | 1.5 ± 0.5 | 0.193 | 1.318 |
| ODI | ||||
| Pre | 47.2 ± 10.0 | 46.9 ± 9.9 | 0.904 | 0.121 |
| 3 Months | 26.7 ± 8.1 | 22.2 ± 6.5 | 0.022* | 2.357 |
| 6 Months | 18.5 ± 5.1 | 15.8 ± 4.4 | 0.033* | 2.183 |
| 9 Months | 13.2 ± 2.5 | 12.0 ± 3.2 | 0.118 | 1.587 |
| 12 Months | 11.4 ± 1.7 | 10.8 ± 2.2 | 0.203 | 1.287 |
Values are presented as mean±standard deviation.
MIS-TLIF-BPS, minimally invasive transforaminal lumbar interbody fusion with bilateral pedicle screw; LLIF-LSUP, lateral lumbar interbody fusion combined lateral single screw-rod and unilateral percutaneous pedicle screw fixation; VAS, visual analogue scale; ODI, Oswestry Disability Index.
Table 3.
Table 4.
| Variable | MIS-TLIF-BPS (n = 36) | LLIF-LSUP (n = 26) | p-value | t/χ2 |
|---|---|---|---|---|
| DH | ||||
| Pre | 7.6 ± 1.3 | 7.3 ± 1.7 | 0.425 | 0.804 |
| 3 Days | 9.7 ± 1.2 | 11.6 ± 1.4 | 0.000* | 5.774 |
| 12 Months | 8.7 ± 1.2 | 10.3 ± 1.2 | 0.000* | 4.969 |
| FH | ||||
| Pre | 16.2 ± 2.1 | 15.7 ± 2.6 | 0.409 | 0.832 |
| 3 Days | 18.4 ± 2.3 | 20.3 ± 2.9 | 0.007* | 2.783 |
| 12 Months | 17.6 ± 2.1 | 19.2 ± 2.4 | 0.003* | 3.028 |
| LLA | ||||
| Pre | 34.5 ± 9.8 | 35.1 ± 9.2 | 0.809 | 0.242 |
| 3 Days | 37.1 ± 6.4 | 40.8 ± 7.2 | 0.037* | 2.131 |
| 12 Months | 36.7 ± 6.3 | 40.1 ± 6.9 | 0.484 | 2.015 |
| SLA | ||||
| Pre | 8.1 ± 2.3 | 8.4 ± 2.1 | 0.601 | 0.525 |
| 3 Days | 10.9 ± 3.1 | 13.2 ± 2.9 | 0.004* | 2.961 |
| 12 Months | 10.5 ± 2.8 | 12.7 ± 2.8 | 0.003* | 3.053 |
| SP | ||||
| Pre | 22.4 ± 10.1 | 21.6 ± 7.9 | 0.738 | 0.336 |
| 3 Days | 2.5 ± 1.0 | 2.1 ± 0.7 | 0.085 | 1.751 |
| 12 Months | 2.8 ± 1.1 | 2.3 ± 0.8 | 0.054 | 1.970 |
| CSA | ||||
| Pre | 80.3 ± 13.2 | 84.5 ± 7.7 | 0.152 | 1.452 |
| 3 Days | 124.8 ± 16.7 | 105.4 ± 8.7 | 0.000* | 5.409 |
| 12 Months | 122.4 ± 16.1 | 113.2 ± 9.6 | 0.012* | 2.600 |
| Fusion rate | ||||
| 3 Months | 13 (36.1) | 15 (57.7) | 0.045* | 4.029 |
| 6 Months | 21 (58.3) | 19 (73.1) | 0.231 | 1.434 |
| 9 Months | 27 (75) | 22 (84.6) | 0.359 | 0.842 |
| 12 Months | 31 (86.1) | 24 (92.3) | 0.723 | 0.125 |
Values are presented as mean±standard deviation.
MIS-TLIF-BPS, minimally invasive transforaminal lumbar interbody fusion with bilateral pedicle screw; LLIF-LSUP, lateral lumbar interbody fusion combined lateral single screw-rod and unilateral percutaneous pedicle screw fixation; DH, disc height; FH, foraminal height; LLA, lumbar lordosis angle; SLA, segmental lordosis angle; SP, slipping percentage; CSA, cross-sectional areas.
REFERENCES

- TOOLS
- Related articles in NS
-
Journal Impact Factor 3.2



























