 |
 |
- Search
|
|
||
Abstract
Objective
To illustrate a simultaneous single-position oblique lateral interbody fusion (SP-OLIF) combined with unilateral percutaneous pedicle screw fixation in treating single-level lumbar tuberculosis, compared with posterior-only approach in clinical and radiographic evaluations.
Methods
Consecutive patients who had undergone surgeries for single-level lumbar tuberculosis from January 2018 to December 2020 were retrospectively reviewed. The patients included were divided into SP-OLIF and posterior-only groups according to surgical methods applied, with follow-up for at least 36 months. Outcomes included estimated blood loss, operative time, and complications for safety evaluation; visual analogue scale (VAS), Oswestry Disability Index (ODI) for efficacy evaluation; erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) for evaluating tuberculosis activity; x-ray and computed tomography scan were used for radiographic evaluation.
Results
A total of 136 patients had been enrolled in the study (60 for SP-OLIF and 76 for Posterior-only). The median operative time, blood loss, and hospital stay in SP-OLIF group were significantly less, with a lower complication rate. Meanwhile, the SP-OLIF group showed substantially lower VAS in 1 and 7 days and decreased ODI in the first month postoperatively, without significant difference afterward. Similarly, the median CRP and ESR in SP-OLIF group were significantly lower in 3 and 7 days postoperatively. All indicators had reduced to normal after 3 months. No recurrence had been reported throughout the whole follow-up.
Lumbar tuberculosis had been challenging due to progressive bony destruction and abscesses formation refractory to chemotherapy, leading to segmental instability and deformity along with intolerable symptoms [1,2]. Surgical management had been debated for decades on how to achieve efficient debridement and rigid fixation whereas the optimal protocol remained controversial [3]. Traditional anterior approach had once been the standard protocol due to excellent ability in debridement and reconstruction, whereas large incisions with unignorable vascular or visceral morbidities had raised increasing concerns. As an alternative, posterior-only approach was increasingly popularized with advantages in effective alignment reconstruction and instrumentation [4,5]. However, excessive soft tissue dissection with inconvenient surgical routine and obstructed visualization had prevented the technique from becoming an optimal protocol complying with minimal invasiveness principle.
Fortunately, the last decade had witnessed impressive advance of minimally invasive lateral retroperitoneal approach in treating lumbar spondylopathies, especially oblique lateral interbody fusion (OLIF) applied in management of disc degeneration diseases with the goal of minimizing intraoperative blood loss, decreasing postoperative pain, facilitating early ambulation and discharge from hospital [6-9]. Meanwhile, the technique had also been reported to be applied in treating tuberculous spondylitis with satisfactory results confirmed [10]. Nevertheless, classical OLIF surgery involved lateral decubitus position for debridement and reconstruction followed by prone position for posterior instrumentation to achieve rigid fixation, necessitating intraoperative reposition, inevitably prolonging operative time and triggering risk of position-oriented morbidities, which had been considered an apparent deficiency in treating lumbar tuberculosis.
Against the background, the study aimed to (1) illustrate a simultaneous single-position OLIF technique combining lateral fixation with unilateral percutaneous pedicle screw fixation; (2) compare the present technique with traditional posterior-only approach in treating single-level lumbar tuberculosis based on clinical and radiographic evaluation; (3) provide an innovative minimally invasive protocol with enhanced efficacy and convenience for treating single-level lumbar tuberculosis.
Surgery indications included (1) significant abscesses and bony destruction; (2) segmental instability or deformity; (3) neurological dysfunction by compression; (4) unbearable back pain refractory to standardized antituberculosis chemotherapy.
The research was approved by the ethics committee of the First Affiliated Hospital of Army Medical University (approval No. (B)KY2023009). Informed consent was obtained from all individual participants included in the study.
The retrospective study was performed in line with STROBE (strengthening the reporting of observational studies in epidemiology) criteria [11]. During a 3-year period from January 2018 to December 2020, consecutive patients who had been diagnosed single-level lumbar tuberculosis and undergone surgeries were retrospectively reviewed. Inclusion criteria included (1) single-level cases with lesions in the anterior-middle column without neurological compression, ensuring the feasibility for both SP-OLIF and posterior surgery; (2) having undergone SP-OLIF or posterior-only surgeries (all patients had been provided alternatives to determine their surgery method preoperatively on their own after being fully informed of the characteristics of both surgeries); (3) affected-vertebra fixation without extension; (4) follow-up for at least 36 months. Exclusion criteria included (1) multilevel fixation; (2) spinal deformity warranting correction; (3) severe radiculopathy or cauda equina injury necessitating posterior circumferential decompression; (4) prior intra-abdominal or retroperitoneal surgery or other conditions unsuitable for lateral approach. Consequently, a total of 136 patients were enrolled in this study, including 60 cases in SP-OLIF group and 76 cases in posterior-only group.
Posterior unilateral percutaneous fixation: Patients after general anesthesia were placed in lateral decubitus position on the side dependent on lesion location. Except for cases with lesion located mainly on the right, right lateral decubitus position (Fig. 1A) was preferred to avoid inferior vena cava. Unilateral percutaneous fixation was performed under the guidance of fluoroscopy without repositioning to prone position (Fig. 1B, C). As a rule, affected-vertebra fixation was encouraged if only sufficient screw purchase could be confirmed during screw placement. In cases with severe bony defect or osteoporosis, the fixed range should extend 1 or 2 levels above or below according to individualized condition.
Lateral exposure, debridement, reconstruction, and fixation: Fluoroscopy was used to localize the targeted level with the anterior vertebral border marked on the skin before a 4- to 6-cm incision anterior to the middle of the targeted disc was made. The external oblique, internal oblique, and transversus abdominis were bluntly divided along fiber orientation to expose underlying retroperitoneal fat before entering retroperitoneal space. Medial and dorsal palpation with fingers along the transverse process and psoas help confirm the ideal orientation. Further ventral palpation would reach the anatomical space between the psoas and aorta, followed by retractors placed for initial passage establishment (Fig. 1D). The peritoneum and abdominal organs were mobilized ventrally to enlarge the space for further exposure. A guiding pin was utilized for level confirmation by fluoroscopy followed by retractors placed sequentially to create an access corridor which was fixed to a table-mounted arm assembly. Under magnification via loupes, necrotic materials would be visible and accessible during the exposure process above. Various curettes, rongeurs, and scalpels were sequentially utilized to absolutely remove lesion including sequestrum, necrotic disc, pus, and caseous necrosis tissue which was reserved for laboratory test. Adequate irrigation with saline solution, hydrogen peroxide, and iodophor was alternatively performed before the titanium mesh/biocage with autograft particles collected from iliac bone was placed for reconstruction. Generally, allogenic bone cage filled with autograft bone was the common option for cases without excessive defect. Titanium mesh filled with autograft was often used in severe defect which was difficult to reconstruct even with the largest allogenic cage (13 mm in height). Lastly, lateral instrumentation on affected vertebrae was performed under direct vision (Fig. 1E) in the presence of posterior fixation. Notably, the compression procedure on the screws should be performed simultaneously from the lateral and posterior by the surgeon and assistants which was checked by fluoroscopy.
The standardized posterior-only procedure for single-level lumbar tuberculosis was performed according to Wu et al. [12]. In detail, patients were placed in prone position after anesthesia. Extraperiosteal dissection was performed through a middle incision to expose posterior structure of the affected vertebrae including the lamina, articular process, and transverse process. Entry points confirmed, pedicle screws were inserted in the affected vertebrae with freehand technique [13]. Then a rod was applied to provide temporary stability to avoid neurological injury during decompression and focal debridement. Subsequentially, bilateral posterior elements including articular processes and lamina were removed to expose the affected disc, which was resected to expose the underlying lesion around the anterior-middle column through transforaminal approach. Curettes and rongeurs were utilized alternatively to remove the lesion as completely as possible, which was reserved for postoperative laboratory test. Copious irrigation was performed with saline solution, hydrogen peroxide, and iodophor before the titanium mesh/cage with autograft particles was placed for reconstruction. Lastly, another rod was applied, and all the screws were tightened.
All patients had received standardized antituberculosis chemotherapy (isoniazid+rifampicin+pyrazinamide+ethambutol) for at least 4 weeks before surgery, with erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) significantly decreased. It was worth noting that all patients in the study were able to endure the 4-week chemotherapy owing to the absence of neurological compression. As for cases with significant neurological compression which had been excluded from the study, the therapy duration could be reduced to 2 weeks for earlier neurological restoration. After surgery, lesion removed was sent to laboratory immediately for drug susceptibility tests to guide subsequent antituberculosis chemotherapy, which generally lasted for 18 months.
Indicators including estimated blood loss, operative time, complication profile and hospital stay were used for clinical safety evaluation; perioperative visual analogue scale (VAS), Oswestry Disability Index (ODI) for clinical efficacy evaluation; ESR and CRP for evaluating tuberculosis activity and recurrence risk in follow-up.
Standard anteroposterior and lateral view of x-ray was taken perioperatively and in follow-up. Fusion assessment was made in 12 months postoperatively according to Bridwell criteria [14]. Computed tomography (CT) scan was required in all cases postoperatively to assess debridement and screw accuracy. In cases with inaccessible contralateral psoas abscess, additional CT-guided percutaneous drainage catheterization had been performed before discharge from hospital.
All evaluations above were conducted by 2 independent observers blinded to the study and any dispute would be designated to a third senior surgeon for final confirmation.
Data was presented as mean ± standard deviation or median (interquartile range) according to normality analysis for various variation, numbers and percentage for category variation. Statistics evaluation was made with IBM SPSS Statistics ver. 26.0 (IBM Co., Armonk, NY, USA). Student t-test and Mann-Whitney U-test were used for continuous variation and chi-square test for category variation. A p-value of < 0.05 was regarded significant difference.
As shown in Table 1, a total of 136 patients (52 for males and 84 for females) had been enrolled in the study (60 for SP-OLIF and 76 for posterior-only group). The mean age was 47.4 ± 12.1 years (range, 24–78 years) with mean follow-up ranging from 36 to 52 months. The involved range included upper lumbar (L1/2, 40 cases) and lower lumbar (L2–5, 96 cases). Demographic date did not show significant difference between the 2 groups (p > 0.05).
As shown in Table 2 of clinical safety evaluation, the median operation time (160; interquartile range [IQR], 180–150 minutes), blood loss (320; 450–290 mL), hospital stay (8; 8–7 days) in SP-OLIF group were significantly less than posterior-only group (207.5 [230–180] minutes; 500 [600–400] mL; 10 [12–9] days; p < 0.05). The total complication rate in SP-OLIF group was 10.0% (6 of 60 cases), significantly less than 21.1% (16 of 76 cases) in posterior-only group. In SP-OLIF group, intraoperative peritoneal tear had been detected in 1 case during corridor establishment and immediately sutured without obvious abdominal symptom in follow-up. Five cases had reported transient thigh numbness after surgery, which had been significantly ameliorated after 2-week symptomatic treatment. In posterior-only group, 2 cases had postoperative cerebrospinal fluid (CSF) leakage and were required to receive 48-hour bed rest, without obvious symptoms presented afterward. Twelve patients demonstrated transient nerve root irritation after surgery, presented as lower limb numbness, all of which had been significantly mitigated after 4-week symptomatic treatment. In addition, 2 cases had experienced poor wound healing and been treated with timely subcutaneous debridement and suturing.
Clinical efficacy evaluation was shown in Table 3. The median preoperative VAS-back score and ODI in SP-OLIF group were 5.0 (6.0–5.0) and 48 (55–45), without marked difference compared with posterior-only group (5.0 [6.0–5.0] and 52 [58–45], p > 0.05). Notably, the median postoperative VAS-back in SP-OLIF group was significantly lower than posterior-only group in 1 day (3.0 [3.0–2.0] vs. 4.0 [4.0–3.0], p < 0.05) and 7 days (2.0 [2.0–2.0] vs. 3.0 [3.0–2.0], p < 0.05), without marked distinction in further follow-up. Furthermore, the median ODI in SP-OLIF group was significantly decreased compared with posterior-only group in 1 month postoperatively (25 [27–22] vs. 35 [35–32], p < 0.05), without significant difference in further follow-up. In addition, though no significant difference was detected in preoperative baseline, the median postoperative CRP in SP-OLIF group was 40 (45–35) mg/L after 3 days and declined to 27.5 (30–22) mg/L after 7 days, which was significantly lower than posterior-only group after 3 days (68 [85–60] mg/L) and 7 days (43.5 [48–34] mg/L) postoperatively. Similarly, the postoperative ESR in SP-OLIF group was also markedly less than posterior-only group in the first week (p < 0.05). All laboratory indicators had decreased to normal in 3 months without difference between the 2 groups. No recurrence or drug-resistant tuberculosis had been reported in any group throughout the whole follow-up.
As shown in Table 4, a total of 240 and 304 screws had been placed in SP-OLIF group and posterior-only group respectively. The overall accuracy in SP-OLIF group was 93.3% (224 of 240 screws) with 16 minor perforations (< 2 mm) detected by postoperative CT scan including 4 medial, 10 lateral, and 2 superior orientations, comparable with 92.1% in posterior-only group (280 of 304 screws), without significant difference in perforation distribution between the 2 groups (p > 0.05). No medial perforation in any group had been shown to exceed 4 mm, indicating limited risk of neurological injury or strength loss. In fusion assessment according to Bridwell criteria [14], of 60 cases in SP-OLIF group, 58 cases had achieved grade I fusion with 2 case rated grade II in 12 months postoperatively. Comparably, in posterior-only group, 72 cases were rated as grade I with 4 cases as grade II. No obvious instrument failure or recurrence had been detected in the follow-up in any group.
Due to the additionally dealing with rib and diaphragm in upper lumbar (L1/2) cases, we had also conducted subgroup analysis of upper lumbar between SP-OLIF and posterior-only group in clinical safety and efficacy indicators. Consequently, despite extra time and effort in dissecting the rib and diaphragm, SP-OLIF group still manifested obvious advantages in decreased operative time and intraoperative blood loss compared with posterior-only group (Supplementary Table 1). Meanwhile, Significant difference had also been detected in VAS (1 and 7 days postoperative) and ODI (1 month postoperative), along with lab indicators in CRP and ESR (3 and 7 days postoperative) (Supplementary Table 2).
Surgical management for lumbar tuberculosis had undergone profound development since the advent of anterior debridement and arthrodesis by Hodgson in 1960s [15]. Excellent visualization and efficient debridement had once been the main contributors to the technique’s wide application in treating tuberculous spondylitis. Nevertheless, despite retroperitoneal access to the lesion, large oblique incisions combined with unignorable access-associated morbidities were obviously against the trend of minimal invasiveness [16,17]. In addition, inadequate deformity correction combined with paucity of rigid anterior fixation had furtherly restricted the technique’s application. Alternatively, posterior approach gradually attained popularity owing to reliable alignment reconstruction and rigid fixation [18-20]. Nevertheless, though studies advocating posterior advantages had claimed favorable results in clinical and radiographic evaluation, controversaries remained whether posterior-only approach would achieve thorough debridement, due to inconvenient operation routine and obstructed visualization, with risk of infection spreading into the canal [21], especially in cases with copious lesion around anterior-middle column. Moreover, excessive tissue dissection in open posterior surgeries was reported to be associated with multiple postoperative morbidities [22]. Therefore, neither traditional anterior-only nor posterior-only approach could be regarded the optimal protocol in the trend of minimal invasiveness. The last decade had witnessed rapid advances of minimal invasive lateral approach, especially OLIF technique in treating degenerative diseases with advantages of reduced blood loss, less postoperative pain, earlier mobilization, and shorter hospital stay [23,24]. Nevertheless, typical OLIF could not achieve thorough debridement, reliable reconstruction and rigid instrumentation simultaneously in single position, which would warrant staged posterior instrumentation in prone position to provide reliable 3-column fixation. Therefore, staged surgical procedure and complex position administration had limited the protocol in wider application. To cope with the drawbacks above, single-position OLIF combined with unilateral percutaneous pedicle screw fixation was gradually performed in our department, achieving efficient debridement and rigid instrumentation simultaneously without intraoperative reposition, which had been rarely reported in treating tuberculous spondylitis.
The first advantage of SP-OLIF technique over traditional posterior-only approach in treating single-level lumber tuberculosis was the enhanced efficiency in debridement, which was directly reflected in the discrepant operative time between the 2 groups (160 [180–150] vs. 207.5 [230–180] minutes, p < 0.05). Through an orthogonal operation routine rather than an oblique one, under direct visualization instead of being obstructed in posterior approach, lesions including sequestrum, caseous necrosis, pus and other affected tissues could be removed with enhanced efficiency. In addition, the obviation of intraoperative position flipping eliminated the necessity of resterilization and redraping, which could greatly smooth the surgical procedure and significantly decrease operative time compared with traditional lateral-then-prone procedure [25]. Meanwhile, the advantage of decreased operative time was still valid compared with previous literature about treating single-level lumbar tuberculosis via posterior approach which reported the mean operative time to be ranging from 161.8 ± 24.6 minutes by Xu et al. to 247.9 ± 59.8 minutes by Du et al. [7,21,26,27]. Therefore, SP-OLIF technique had a significant advantage over both traditional lateral-thenprone OLIF surgery and posterior-only surgery on operative time, which should be ascribed to enhance efficiency in debridement combined with 1-stage procedure.
Previous studies of posterior-only approach in treating singlelevel tuberculosis had reported the average bleeding to be over 500 mL [26-29], consistent with our result in posterior approach. In contrast, the median blood loss in SP-OLIF group was significantly reduced (320 [450–290] mL vs. 500 [600–400] mL, p<0.05), which should be ascribed to the following aspects. Firstly, due to a small incision along with retroperitoneal access by blunt dissection, approach-related injury was significantly reduced compared with traditional open procedures. Furthermore, direct access to lesion through retroperitoneal approach without irritation to canal and dural sac could avoided epidural venous hemorrhage, which might be intractable in posterior approach. Meanwhile, operation under direct vision would greatly facilitate rapid hemostasis during debridement and reconstruction. Lastly, shorter operative time also contributed to less interoperative bleeding. Nevertheless, precaution should be taken in developing the retroperitoneal space for the risk of artery injury.
Direct access to lesion via lateral approach also obviated irritation to posterior nerve structure, greatly decreasing risk of postoperative neurological dysfunction. Consequently, in posterior-only group, nerve root irritation had been detected in 12 cases presented as transient limb numbness due to root distraction during debridement and reconstruction, which was significantly relieved after 4-week symptomatic treatment. Meanwhile, 2 cases had shown postoperative CSF leakage without obvious symptom. In contrast, transient thigh or psoas pain/weakness had been reported in 5 cases in SP-OLIF group and alleviated after 1-week symptomatic treatment, which might be ascribed to overtraction of psoas during debridement. Therefore, the decreased neurological morbidities should be regarded another advantage of the minimal invasive lateral approach over posterior approach. Nevertheless, it should be noted that the study did not involve cases with severe neurological compression necessitating direct decompression. Given the obvious discrepancy in direct circumferential decompression between lateral and posterior approach, whether the advantage remained valid in such cases remained to be confirmed in further research.
In clinical efficacy evaluation, the study had manifested greater improvement in SP-OLIF group in terms of VAS in the first week and ODI in 1 month postoperatively, without marked distinction in 3 months or longer follow-up. Similar phenomena had also been detected in laboratory tests including CPR and ESR. Analyzing the impressive discrepancy in the indicators above between early and late stage, iatrogenic trauma might be the main cause responsible for the difference. Longer surgical incision with excessive tissue dissection inevitably produced stronger postoperative pain around surgical sites in traditional posterior approach, which was a common postoperative complaint [30]. In addition, excessive iatrogenic trauma with increased intraoperative bleeding and postoperative complications would result in delayed off-bed mobilization, adversely affecting rehabilitation at early stage. Compared with posterior-only surgery, SP-OLIF technique could reduce iatrogenic trauma to a minimal level due to minimally invasive debridement and percutaneous fixation. The decreased intraoperative iatrogenic trauma, combined with improved postoperative pain and disability substantially promoted the implementation of Enhanced Recovery After Surgery (ERAS), a concept prevailing worldwide aiming to improve early rehabilitation and physical functions with decreased hospital stay [31]. As was well-documented, adequate analgesic medication laid the foundation for ERAS while the prolonged usage was reported associated with increased incidence of complications including gut dysfunction and nausea/vomiting. Therefore, the significantly decreased pain score after operation could greatly reduce analgesic medication including opioids and nonsteroidal anti-inflammatory drugs in dosage and duration. Furthermore, due to the less iatrogenic trauma and complications, early off-bed mobilization and diet resumption were more prone to be achieved in SP-OLIF group, leading to less intravenous fluid during hospital stay. Such advantage would be more obvious in elderly patients with complicated cardio-cerebrovascular complications, as longer bed rest had been confirmed a vital contributor to postoperative morbidities associated with enhanced mortality. Meanwhile, the discrepancy in hospital stay not only reflected the rehabilitation difference between the 2 groups, but also associated with differentiated medical cost which had been considered an serious issue in developing countries. Therefore, the significant difference in early clinical improvement had produced substantial and comprehensive benefits to patients from medical and socioeconomical perspectives. Notably, though no marked discrepancy was illustrated between the 2 groups in further follow-up, it was difficult to conclude 2 protocols were undistinguishable on long-term prognosis, given the standardized drug susceptibility-based chemotherapy (no drug resistance detected in any group) through the whole follow-up in both groups. Nevertheless, with advantages including enhanced debridement efficiency, decreased blood loss, shortened operative time and reduced complication profile considered, SP-OLIF should be regarded preferable to traditional posterior-only surgery achieving equivalent clinical improvement with more advantages.
Minimally invasive percutaneous instrumentation under fluoroscopy guidance was the common practice in SP-OLIF group. Different from traditional single-position surgery adopting posterior dual pedicle fixation, SP-OLIF technique adopted hybrid fixation combining lateral instrument with unilateral pedicle instrument to constitute dual rod-screw instrumentation. The combination provided adequate mechanical rigidity close to traditional dual pedicle fixation without the need of dealing with contralateral pedicle, given the trouble of contralateral pedicle fixation in lateral position. It should be noted that dual pedicle screw placement in single lateral position was also feasible, only if patients should be placed close to the edge of operation table and elevated higher than the normal [32], which might result in unnecessary inconvenience and security concern. Lastly, it had to be admitted that a learning curve existed before surgeons got accustomed to unilateral posterior instrumentation in lateral position. Nevertheless, prior experience of percutaneous fixation in prone position would shorten the time required and render the transformation smooth.
Due to the innovative combination of lateral debridement and reconstruction with posterior fixation, single-level lumbar pathology was the main indication for the present technique, including infectious and degenerative diseases. Notably, in treating tuberculous spondylitis, the technique was not feasible in all situations. Firstly, the intactness of posterior articular structure obviated the possibility of effective deformity correction as in posterior approach via osteotomy. Even the partial correction by intervertebral distraction via a large expandable anterior cage could not be achieved as in degenerative cases, secondary to severe destruction to the anterior endplate and vertebrae. Therefore, SP-OLIF technique was not suitable for cases with obvious kyphosis requiring correction. Secondly, multilevel cases were not suitable either secondary to the difficulty in performing multi-segment percutaneous screw fixation in lateral position. Thirdly, the technique was not recommended in cases involving severe radiopathology or cauda equina symptom. Compared with posterior approach in which debridement was performed from the visible posterior to the invisible anterior with dural sac and nerve roots in view, the operation order in lateral approach was just the reverse, from the visible anterior lesion to the invisible posterior neurological structure, carrying with it potential risk during neurological decompression. Other contraindications included (1) prior vascular reconstructive surgery; (2) prior intra-abdominal or retroperitoneal surgery; (3) history of severe pelvic inflammatory disease.
In cases involving upper lumbar vertebrae (L1–2), special attention should be paid in dealing with rib and diaphragm before retroperitoneal space was developed. As a rule, the 12th rib was to be partially resected for adequate surgical field with L1–2 involved [33]. In dissection of diaphragm, meticulous blunt separation was critical in protecting the thin muscle from unnecessary damage. In mobilizing the peritoneum anteriorly, gauze soaked in saline solution was recommended as a buffer layer against potential risk of tear, which may lead to infection spreading during debridement. Doubtlessly, extra effort in dealing with the rib and diaphragm would moderately increase operation time and blood loss. Nevertheless, from the results (Supplementary Tables 1, 2) in our study, SP-OLIF still showed significant advantage in indicators including operative time, blood loss, hospital stay, and lab indicators including CRP and ESR at early stage (p < 0.05), indicating the validity of minimal invasiveness advantage in upper lumbar despite the extra effort.
To cope with the significant destruction to vertebrae and endplate, our team had adopted various measures to achieve anterior reconstruction including biocages/titanium mesh loaded with autograft particles, or allograft blocks with autograft particles according to individualized situations. As for large columnar defect after radical debridement, titanium mesh loaded with autograft particles was a standard option [34], which, however, would necessitate large amounts of autogenic resource from iliac crest with risk of donor site morbidity [35]. Therefore, besides titanium mesh and biocage applied in the study, an allograft block with autograft particles was also a common alternative we adopted to decrease the requirement of autograft. Rigid structural support by an allograft block combined with surrounding autogenic particles prone to rapid osteogenesis facilitated satisfactory bony fusion along with alignment maintaining. As for cases with cavernous defect, we recommended placing loaded cages on residual surface as structural support with autogenous particles filling the cavity. Compared with traditional titanium mesh loaded with autogenous particles emphasizing central placement, the methods above allowed eccentric placement on residual surface and laid more emphasis on sufficient filling with autogenous particles. Long-term follow-up of these implants had manifested satisfactory fusion compared with traditional titanium mesh, which we are looking forward to reporting in near future.
Though the study had provided preliminary evidence on the advantages of SP-OLIF technique over traditional posterior-only approach in treating single-level lumber tuberculosis, it was worth noting that the protocol had only been performed in a single center. Further multi-center prospective studies were warranted to further assess the technique’s validity and feasibility.
SP-OLIF was a reliable minimally invasive protocol for single-level lumbar tuberculosis, facilitating efficient anterior debridement and rigid posterior instrumentation simultaneously free from intraoperative reposition, with decreased blood loss, shorter operative time, and hospital stay compared with posterior-only approach.
Supplementary Material
Supplementary Tables 1 and 2 can be found via https://doi.org/10.14245/ns.2346692.346.
Supplementary Table 1.
Subgroup clinical comparison in upper lumbar between the 2 groups
Supplementary Table 2.
Subgroup clinical efficacy evaluation in patient-reported and lab test
ACKNOWLEDGEMENTS
The authors would like to thank Jianzhong Xu for valuable assistance with the research.
Fig. 1.
Illustration of single-position oblique lateral interbody fusion technique in single-level lumbar tuberculosis. (A) Right lateral decubitus position. (B, C) Unilateral percutaneous fixation under fluoroscopy in lateral decubitus position. (D) Initial establishment of retroperitoneal space. (E) Lateral instrumentation in presence of posterior fixation.
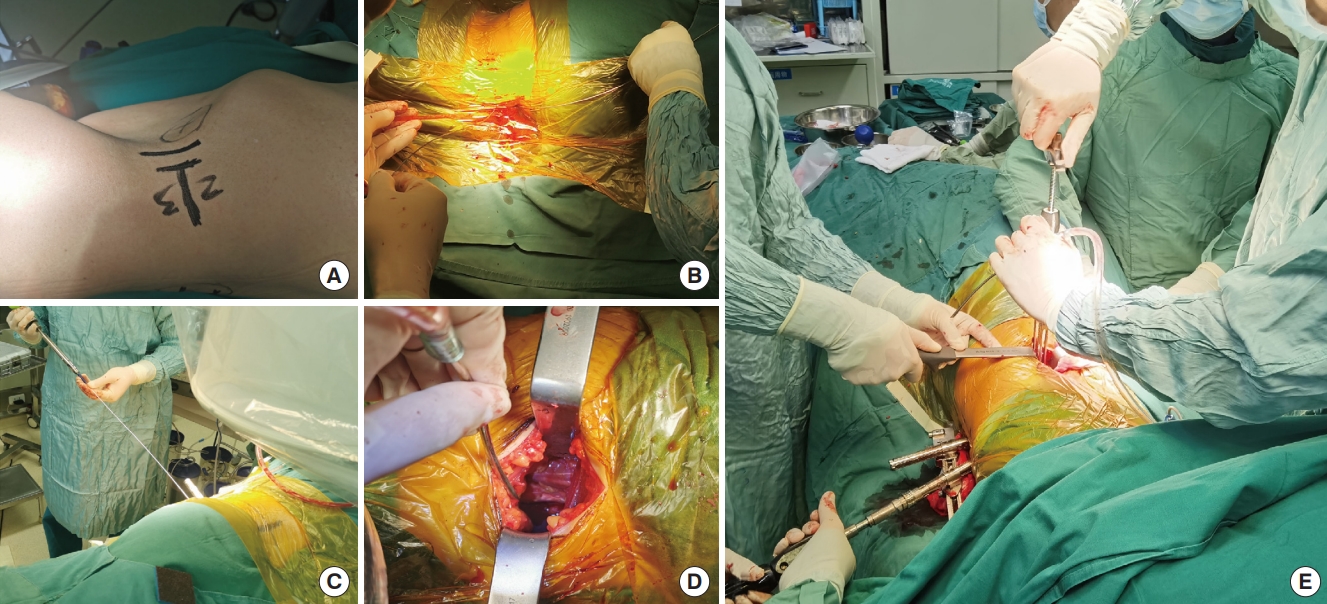
Fig. 2.
Perioperative radiographic images of a representative case diagnosed as L3/4 tuberculosis in single-position oblique lateral interbody fusion group applying a biocage as implant. (A, B) Preoperative x-ray in coronal and lateral view. (C, D) Preoperative computed tomography (CT) scan in lateral and transverse view. (E, F) Magnetic resonance imaging in transverse and lateral view. (G, H) The postoperative x-ray in coronal and lateral view. (I-L) Postoperative CT scan after 1 year in lateral, coronal and transverse view.
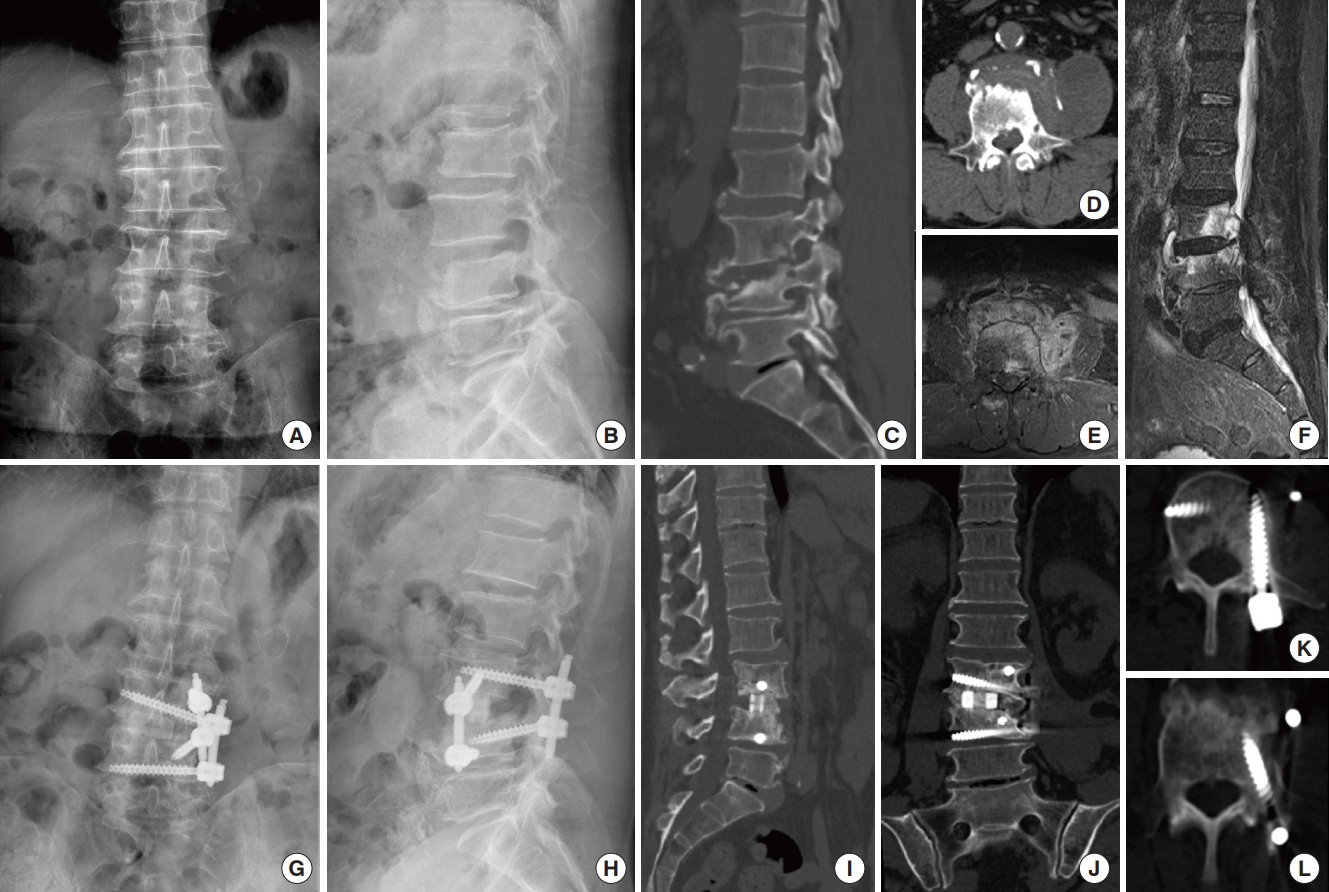
Fig. 3.
Perioperative images of a representative case diagnosed as L3/4 tuberculosis in single-position oblique lateral interbody fusion group adopting titanium mesh as implant. (A, B) Preoperative x-ray in coronal and lateral view. (C) Preoperative computed tomography (CT) scan in lateral view. (D, E) The postoperative x-ray in lateral and coronal view. (F–I) The postoperative CT scan in lateral, coronal and transverse view. (J, K) The 1-year postoperative x-ray in lateral and coronal view.

Table 1.
Demographic data between SP-OLIF and posterior group
Table 2.
Clinical safety evaluation between the 2 groups
Table 3.
Clinical efficacy evaluation between the 2 groups in patient-reported and lab test
REFERENCES
1. Dunn RN, Ben Husien M. Spinal tuberculosis: review of current management. Bone Joint J 2018;100-B:425-31.

2. Pan Z, Cheng Z, Wang JC, et al. Spinal tuberculosis: always understand, often prevent, sometime cure. Neurospine 2021;18:648-50.




3. Muheremu A, Niu X, Wu Z, et al. Study on anterior and posterior approaches for spinal tuberculosis: a meta-analysis. Eur J Orthop Surg Traumatol 2015;25 Suppl 1:S69-76.



4. Long W, Gong L, Cui Y, et al. Single posterior debridement, interbody fusion, and fixation on patients with continuous multivertebral lumbar spine tuberculosis (CMLSTB). BMC Musculoskelet Disord 2020;21:606.




5. Wang X, Pang X, Wu P, et al. One-stage anterior debridement, bone grafting and posterior instrumentation vs. single posterior debridement, bone grafting, and instrumentation for the treatment of thoracic and lumbar spinal tuberculosis. Eur Spine J 2014;23:830-7.




6. Zhang X, Wang Y, Zhang W, et al. Perioperative clinical features and long-term prognosis after oblique lateral interbody fusion (OLIF), OLIF with anterolateral screw fixation, or OLIF with percutaneous pedicle fixation: a comprehensive treatment strategy for patients with lumbar degenerative disease. Neurospine 2023;20:536-49.




7. Zhu HF, Fang XQ, Zhao FD, et al. Comparison of oblique lateral interbody fusion (OLIF) and minimally invasive transforaminal lumbar interbody fusion (MI-TLIF) for treatment of lumbar degeneration disease: a prospective cohort study. Spine (Phila Pa 1976) 2022;47:E233-42.

8. Kim H, Chang BS, Chang SY. Pearls and pitfalls of oblique lateral interbody fusion: a comprehensive narrative review. Neurospine 2022;19:163-76.




9. Pham MH, Diaz-Aguilar LD, Shah V, et al. Simultaneous robotic single position oblique lumbar interbody fusion with bilateral sacropelvic fixation in lateral decubitus. Neurospine 2021;18:406-12.




10. Du X, Ou Y, Luo W, et al. Evaluation of the efficacy of OLIF combined posterior internal fixation for single-segment lumbar tuberculosis: a single-center retrospective cohort study. BMC Surg 2022;22:54.




11. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007;370:1453-7.


12. Wu W, Li Z, Lin R, et al. Single-stage posterior-only debridement, decompression and interbody fusion for the treatment of thoracolumbar spinal tuberculosis complicated with psoas abscesses. BMC Surg 2021;21:84.




13. He J, Luo F, Wang H, et al. SAP principle guided free hand technique: a secret for T1 to S1 pedicle screw placement. Orthop Surg 2022;14:2995-3002.


14. Bridwell KH, Lenke LG, McEnery KW, et al, Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976) 1995;20:1410-8.

15. Hodgson AR, Stock FE. The classic: anterior spinal fusion: a preliminary communication on the radical treatment of Pott’s disease and Pott’s paraplegia. 1956. Clin Orthop Relat Res 2006;444:10-5.

16. Bateman DK, Millhouse PW, Shahi N, et al. Anterior lumbar spine surgery: a systematic review and meta-analysis of associated complications. Spine J 2015;15:1118-32.


17. Kondo S, Hamano K, Kamijo M, et al. Transperitoneal approach to the lower lumbar and the lumbosacral vertebra for the treatment of tuberculous spondylitis. Bull Osaka Med Sch 1964;10:79-88.

18. Chen RS, Liao X, Xiong ML, et al. One-stage posterior approach for treating multilevel noncontiguous thoracic and lumbar spinal tuberculosis. Postgrad Med 2019;131:73-7.


19. Liu Z, Zhang P, Li W, et al. Posterior-only vs. combined posterior-anterior approaches in treating lumbar and lumbosacral spinal tuberculosis: a retrospective study with minimum 7-year follow-up. J Orthop Surg Res 2020;15:99.




20. Xu Z, Wang X, Liu Z. One-stage posterior debridement and single-segment interbody fusion for treating mono-segmental lumbar and lumbosacral spinal tuberculosis in adults following minimum 5-year follow-up. J Orthop Surg Res 2020;15:473.




21. Wang T, Ma Z, Lei W, et al. Clinical efficacy of different open approaches in the surgical treatment of thoracolumbar tuberculosis: a single-center retrospective comparative study. J Orthop Surg Res 2023;18:352.




22. Fan W, Yang G, Zhou T, et al. One-stage freehand minimally invasive pedicle screw fixation combined with mini-access surgery through OLIF approach for the treatment of lumbar tuberculosis. J Orthop Surg Res 2022;17:242.




23. Li R, Li X, Zhou H, et al. Development and application of oblique lumbar interbody fusion. Orthop Surg 2020;12:355-65.




24. Phan K, Maharaj M, Assem Y, et al. Review of early clinical results and complications associated with oblique lumbar interbody fusion (OLIF). J Clin Neurosci 2016;31:23-9.


25. Ziino C, Konopka JA, Ajiboye RM, et al. Single position versus lateral-then-prone positioning for lateral interbody fusion and pedicle screw fixation. J Spine Surg 2018;4:717-24.



26. Du X, Ou YS, Zhu Y, et al. Oblique lateral interbody fusion combined percutaneous pedicle screw fixation in the surgical treatment of single-segment lumbar tuberculosis: a single-center retrospective comparative study. Int J Surg 2020;83:39-46.

27. Jiang L, Sheng X, Deng Z, et al. A comparative study of one-stage posterior unilateral limited laminectomy vs. bilateral laminectomy debridement and bone grafting fusion combined with internal fixation for the treatment of aged patients with single-segment spinal tuberculosis. BMC Musculoskelet Disord 2022;23:619.




28. Zheng B, Hao D, Guo H, et al. Anterior versus posterior surgical approach for lumbosacral tuberculosis. J Int Med Res 2018;46:2569-77.




29. Xu Z, Wang X, Zhang Z, et al. A comparison of three bone graft struts for interbody fusion using a posterior approach for lower lumbar spinal tuberculosis in adults: a midterm follow-up study. BMC Musculoskelet Disord 2022;23:590.




30. Waelkens P, Alsabbagh E, Sauter A, et al. Pain management after complex spine surgery: a systematic review and procedure-specific postoperative pain management recommendations. Eur J Anaesthesiol 2021;38:985-94.


31. Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg 2017;152:292-8.


32. Cheng P, Zhang XB, Zhao QM, et al. Efficacy of single-position oblique lateral interbody fusion combined with percutaneous pedicle screw fixation in treating degenerative lumbar spondylolisthesis: a cohort study. Front Neurol 2022;13:856022.



33. Dakwar E, Ahmadian A, Uribe JS. The anatomical relationship of the diaphragm to the thoracolumbar junction during the minimally invasive lateral extracoelomic (retropleural/retroperitoneal) approach. J Neurosurg Spine 2012;16:359-64.



- TOOLS
- Related articles in NS
-
Journal Impact Factor 3.2



























