 |
 |
- Search
|
|
||
Abstract
Osteoporotic vertebral fractures (OVFs) can hinder physical motor function, daily activities, and the quality of life in elderly patients when treated conservatively. Vertebral augmentation, which includes vertebroplasty and balloon kyphoplasty, is a commonly used procedure for OVFs. However, there have been reports of complications. Although serious complications are rare, there have been instances of adjacent vertebral fractures, cement dislocation, and insufficient pain relief due to cement failure, sometimes necessitating revision surgery. This narrative review discusses the common risks associated with vertebral augmentation for OVFs, such as cement leakage and adjacent vertebral fractures, and highlights the risk of revision surgery. The pooled incidence of revision surgery was 0.04 (0.02–0.06). The risks for revision are reported as follows: female sex, advanced age, diabetes mellitus, cerebrovascular disease, dementia, blindness or low vision, hypertension, hyperlipidemia, split type fracture, large angular motion, and large endplate deficit. Various treatment strategies exist for OVFs, but they remain a subject of controversy. Current literature underscores the lack of substantial evidence to guide treatment strategies based on the risks of vertebral augmentation. In cases with a high risk of failure, other surgeries and conservative treatments should also be considered as treatment options.
Osteoporotic vertebral fractures (OVFs) can cause low back pain and inhibit physical motor function, activities of daily living, and quality of life in elderly patients treated conservatively [1-3]. Furthermore, OVFs increase the risk of mortality in elderly women [4]. Therefore, OVFs exert a significant health burden, especially in an aging society [5]. While a decreasing trend in the incidence of hip fractures is observed in many countries, occurrence of OVFs is increasing [6,7]. Recently, a declining trend in osteoporotic medication after OVFs is reported in the United States [8]. The treatment for osteoporosis should be improved to preserve population health by increasing the medication rate. There is no universal conservative treatment including bed rest, spinal orthosis, and physical therapy. Basically, immobilization owing to bed rest can be harmful because of the deterioration in bone loss, progressive muscle weakness, thromboembolic disease, joint contracture, and skin ulcer in elderly population [4]. Therefore, physical therapy under spinal orthosis is recommended after short immobilization period, although a recent prospective cohort study [9]. demonstrated that better compression ratio of vertebral body and lower surgical rate were obtained following 2 weeks of bed rest for patients with risk factors of poor prognosis. Physical therapy is effective to improve osteoporosis and prevent osteoporotic fracture (OF) [10,11]. In most cases, conservative treatment employing brace treatment is effective for the healing process of fractures. However, there is no apparent evidence regarding the type of spinal orthosis between soft and rigid brace [12]. Despite conservative treatment, residual back pain and neurological deficit are observed due to nonunion, severe deformity, and global spinal imbalance [13-15]. Particularly, nonunion is strongly associated with residual back pain compared to local alignment [16].
Vertebral augmentation comprising vertebroplasty and balloon kyphoplasty is a widely used procedure for OVFs, and its safety and usefulness have been reported in many papers [17-19]. Vertebral augmentation provides pain relief and vertebral heigh restoration [20]. As the population ages, cement augmentation is being considered as a treatment for patients who are increasingly older, specifically those who are more than 80 or 90 years old [21]. Additionally, a database study demonstrated that vertebral augmentation can improve the survival rate [22]. Cochrane systematic review [23]. shows weak evidence of vertebral augmentation for vertebral fracture in acute or subacute phase because randomized controlled studies could not find the difference between vertebroplasty and placebo procedure. Therefore, we considered the risk of vertebral augmentation to minimize the harm among elderly patients, which may improve the outcomes of this procedure. The timing of vertebral augmentation is important for surgical outcomes because there are changes in low back pain and compression ratio especially during the first 3 months. A prospective study demonstrated that the quality of life and low back pain improved until 3 months after injury and did not change thereafter until a mean follow-up of 5 years [24].
Previous papers suggest that late intervention worsen the severity of fracture [25,26] as compared to early intervention. However, early intervention may include unnecessary cases with OVFs, which recovery by conservative treatment. Therefore, several papers demonstrated the predicting factors for poor prognosis after conservative treatments to minimize the surgical invasiveness in elderly patients [3,13,18]. There have also been some reports of complications following surgery. Serious complications, which occur in less than 1% of cases [27], include cement leakage into the spinal canal, spinal cord injury, infection, and pulmonary embolization, which may require emergency treatment. Apart from serious complications, there have been cases of adjacent vertebral fractures or dislocation of cement and poor pain relief due to cement failure [28], which sometimes require revision surgery [29-32]. To the authors’ knowledge, there have been no reviews on the incidence and risk of revision surgeries after vertebral augmentation.
The purpose of this study was to investigate the incidence of revision after vertebral augmentation. In addition, we discuss the common risks of vertebral augmentation for OVFs, including cement leakage and adjacent vertebral fractures, and outline the risk of vertebral augmentation.
We conducted a systematic review of the literature identifying revision surgery after vertebral augmentation in patients with vertebral fractures according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines and with guidance from the Cochrane Handbook for Systematic Reviews of Interventions.
For the identification of eligible articles, the individual steps of title and abstract screening, full-text review, and data extraction were performed independently using the MEDLINE database, Cochrane library, and Scopus database. The search strategy included combinations of the terms “vertebroplasty” or “balloon kyphoplasty” or “vertebral augmentation” and “revision” or “reoperation” and “vertebral fracture.” To optimize data mining, word variations and exploded medical subject headings were included whenever feasible. The last literature search was performed on January 9, 2023.
First, incomplete articles and non-English language articles were removed (Fig. 1). Next, review articles and case reports were excluded. Additionally, the articles that included only vertebral augmentation with instrumentations, only trauma cases, ankylosing spondylitis, pathological fracture, cervical spine, and sacral fracture were excluded. Next, the articles on only revision cases after vertebral augmentation were excluded because of lacking revision rate. Finally, we evaluated prospective or retrospective cohort studies to assess the incidence of revision surgery and the risks [31,33-45] (Table 1). The initial screening of titles and abstracts for relevance was conducted by a single reviewer (ST). Full texts of the remaining articles were obtained and assessed for eligibility by comparison with the inclusion criteria. Data were extracted from the included studies by 2 independent reviewers (ST and MI). Any discrepancies during the screening or extraction process were resolved by consensus agreement or adjudication with another author (KT). The risk of bias in each study was evaluated by 2 reviewers (ST and KT). The post intervention biases for selection and reporting were judged using the Risk Of Bias In Non-randomized Studies of Interventions tool as follows: low, moderate, serious, and critical [34] (Table 2). Confounding and information biases were excluded from the assessment because the reviewed articles were not compatible.
Information on the study population, type of intervention, original sample size, average or median age, follow-up period, outcome of the study, revision rate, and risk of revision was collected. Revision surgery included failure of vertebral augmentation, repeated vertebral fracture for new fractures, and salvage for cement leakage. The authors’ main conclusions regarding revision or repeated surgery were summarized.
Pooled incidence of revision after vertebral augmentation was obtained by random-effect meta-analysis using a normal-binomial generalized linear mixed model method in the R packages “meta” (version 4.2.3, R Foundation for Statistical Computing, Vienna, Austria) [46].
A flow diagram of the systematic literature search is provided in Fig. 1. The database search yielded 206 eligible articles after the removal of incomplete, duplicated and non-English articles. During the title and abstract screening, 206 articles were excluded for not meeting the inclusion criteria or for meeting the exclusion criteria. Of the remaining 19 articles, a further 5 records were excluded during full-text screening because they analyzed only revision cases. Finally, 14 articles were used for qualitative synthesis.
Six articles were nationwide or insurance database studies. Five studies were retrospective cohort and 2 were prospective cohort studies. One article was a randomized controlled trial that evaluated KIVA system, which is a novel polyether ether ketone implant, and balloon kyphoplasty [34]. Several studies confirmed osteoporosis as the cause of vertebral fractures, while the other studies included patients who underwent vertebral augmentation for vertebral fracture. The median age in most studies was > 70 years. Although the definition of revision surgery was different due to differences in the purpose of the studies, it was divided into revision surgery, repeat vertebral augmentation, and salvage surgery for cement leakage. In several articles, revision surgery included repeat vertebral augmentation and salvage surgery. The rate of revision ranged from 1.1% to 13%. Repeat vertebral augmentation was relative frequent [35-37]. Repeat vertebral augmentation was performed for new fractures. Salvage surgery was rarely performed for infection (0.36%). The frequency of salvage surgery for cement leakage was 1.7% to 2.3% [34,40]. The pooled incidence of revision surgery was 0.04 (0.02–0.06) (Fig. 2).
The risk factors for revision were reported in several studies [36,39,42]. Chou et al. [42] demonstrated location of fracture at the thoracolumbar junction, fracture type of intravertebral cleft, or wedge-type fracture, and material with nonintegrating properties injected into the fractured vertebra were risk factors associated with the occurrence of progressive kyphosis and neurological complications. Database study demonstrated the following other risk factors for repeat vertebral augmentation: female sex, advanced age, diabetes mellitus, cerebrovascular disease, dementia, blindness or low vision, hypertension, and hyperlipidemia. Patients taking calcium/vitamin D, bisphosphonates, or calcitonin were less likely to undergo repeat vertebral augmentation. Another study [39] showed that split type fracture, greater angular motion, and large endplate deficit increased the risk for revision surgery. Additionally, frailty, elevated creatinine levels, and American Society of Anesthesiologists physical status classification grade IV were independently associated with mortality and complications [38,45]; treatment of osteoporosis, an experienced surgeon, and prophylactic vertebral augmentation may reduce the risk [36,37]. Vertebroplasty and kyphoplasty showed similar revision rates [43].
Revisions following vertebral augmentation have been reported previously. However, few reports have investigated the risk factors for revision. The risks for revision are as follows: female sex, advanced age, diabetes mellitus, cerebrovascular disease, dementia, blindness or low vision, hypertension, hyperlipidemia, split type fracture, angular motion ≥ 14°, and large endplate deficit [36,39,42]. Furthermore, intradiscal leakage may lead to secondary adjacent vertebral fractures [29,47] and a greater angular motion of the fractured vertebra may be associated with greater vertebral height reduction in vertebral augmentation [39]. A significant reduction in vertebral height is also known to be a risk factor for adjacent vertebral fracture [48]. Additionally, the presence of an intravertebral cleft with angular motion has been reported as a poor prognostic indicator after vertebroplasty [49]. A greater angular motion might indicate breakage or dysfunction of the anterior spinal elements, including the anterior longitudinal ligament and annulus, which may lead to failure in retaining the cement with the vertebral body. Anterior dislodgment of cement causes a loss of vertebral height and stability.
There is no standard classification of OVFs. Genant grading has been used for screening and evaluating the impact of OVFs on population health based on a semiquantitative assessment [50]. AO spine classification for thoracolumbar injury is also widely used to evaluate the fracture type and to aid therapeutic and surgical decision making [51]. However, the classification is adequate for trauma because OVFs are fragile fractures caused by minor injury. Recently, the new classification of OVFs, the OF classification, which is a morphologic classification of different types of OVF, was developed by the German Orthopedic and Trauma Society and was also adopted by AO Spine [51]. The classification comprises 5 subgroups as per the OVF severity including endplate fracture and posterior wall injury assessment: OF 1, no deformation (vertebral body edema in MRI-STIR); OF 2, deformation of one endplate without or with only minor posterior wall involvement; OF 3, deformation of one endplate with distinct posterior wall involvement; OF 4, deformation of both endplates with/without posterior wall involvement; and OF 5, injuries with anterior or posterior tension band failure. Additionally, a scoring system was developed for making decisions regarding surgical intervention using the information on severity of osteoporosis, deformity progression, pain, neurological symptoms, mobilization, and health status. The severity of OF was associated with the frequency of surgery and 2% patients required revision surgery. Further research is necessary to investigate the surgical outcome depending on this new classification.
Progressive kyphosis after vertebroplasty is a risk factor for revision surgery and the incidence is reported as 1.5% in a retrospective study [42]. There are risk factors associated with the occurrence of progressive kyphosis and neurological complications after vertebral augmentation, including location of fracture at the thoracolumbar junction, fracture type of intravertebral cleft, or wedge-type fracture, and material of nonintegration properties injected into the fractured vertebra [42,52]. Additionally, significant associations were found between cement distribution patterns and progressive kyphosis in cemented vertebrae, which affected the clinical outcome in patients after vertebral augmentation. The cement distribution included uninterlocked solid pattern, discontiguous trabecular pattern, and solid lump cement pattern [53,54]. The distribution of cement in vertebrae contributes to noncemented cancellous bones without load transfer causing recollapse. Another report stated that [55] insufficient cement distribution is responsible for unrelieved pain. Location of the fractured area is an independent risk factor for the occurrence of insufficient cement distribution; if the fracture is located in the superior portion of the index vertebra, there is a higher incidence of insufficient cement distribution. The recollapse after vertebral augmentation may lead to recurrent back pain and revision surgery; the latter is sometimes necessary to avoid serious consequences. Multiple balloon dilation, location of cement and cement volume may be important to avoid the recollapse.
A previous study [31] summarized the possible revision strategies for failed vertebral augmentation. The surgical strategy to treat cement leakage into the spinal canal causing neurological deficit is urgent laminectomy and fusion. Cement dislodgement or fragmentation also requires anterior or posterior surgery. For infection, extensive debridement is necessary, with combined anterior and posterior surgery being the safest method to treat this complication. Augmentation of pedicle screw fixation, using various bone cements, is less evident, although its use as an initial procedure to improve fatigue strength of instrumentation among patients with severe osteoporosis has been previously investigated [56]. Major complications are rare. However, since severe acute complications requiring emergency treatment may occur, the procedure should be performed by a qualified spinal surgeon [33]. Additionally, for patients with symptomatic failed vertebral augmentation, posterior transpedicular approach surgery with circumferential removal of leaked cement and anterior reconstruction show low complication rate and good clinical outcomes; this can be considered as an alternative method combining anterior and posterior approaches [57].
Vertebral augmentation carries the risk of bone cement leakage and pulmonary embolism [58,59]. Although symptomatic pulmonary embolism is a rare condition [60], pulmonary cement embolism leading to death can occur after uncontrolled leakage [61]. Pedicle violation caused by epidural cement leakage further carries the potential risk of neurological deficit [62]. Therefore, vertebral augmentation should only be performed by experienced surgeons following the identification of critical indications under fluoroscopic or computed tomography (CT) monitoring [61].
Minor cement leakage is frequently noted on CT but is asymptomatic in most cases [63]. Indeed, leakage has been reported to occur in 30%–65% of cases [64]. Decreased integrity of vertebral walls and the volume of injected cement significantly boost the potential risk of cement leakage [65]. Cement leakage adjacent to a disc is frequently encountered, while symptomatic neurological complications due to compression of a nerve root or the spinal cord are less frequent. Vertebral augmentation is also a viable option for the treatment of OVFs, even with posterior wall involvement [66]. High-viscosity cement results in lower bone cement leakage rate and better VAS score improvement compared with low-viscosity cement [58,67]. Application of a large void volume using the balloon and the smaller injected cement than that void might be useful to avoid leakage [66]. The unilateral approach may decrease the incidence of cement leakage due to lower cement dosage [68]. Symptomatic bone cement displacement, which causes poor outcomes after vertebral augmentation is reported to be approximately 2% along with the risks of intravertebral cleft, anterior leakage, and cement distribution [55].
Several reports have investigated the difference between vertebroplasty and kyphoplasty. A meta-analysis [69] that evaluated 121 reports demonstrated that the rate of asymptomatic cement leaks per treated patient was significantly higher for vertebroplasty than for kyphoplasty, although both procedures were effective in symptomatic vertebral compression fractures and there was no difference in mortality. Another meta-analysis further demonstrated that kyphoplasty has a reduced risk of cement leakage and it increases the postoperative vertebral height compared to vertebroplasty; however, it is more expensive and requires longer operative time durations [70]. However, several papers in the current review showed no differences in clinical outcomes and complications between vertebroplasty and kyphoplasty [43,44,71].
The incidence ratio of adjacent vertebral fracture after vertebral augmentation has been calculated as approximately 10%–40% in previous reports [28,72-80]. Most fractures occur within a few months. Vertebral augmentation is known to reduce vertebral kyphotic deformity at the fractured vertebrae, as reported in several previous studies [49,81]. However, correction after vertebral augmentation should be considered in the area including the upper and lower spinal segments. Even if correction can be achieved by kyphoplasty, correction loss may occur following adjacent vertebral fracture or correction loss of the vertebral body. Hard cement may further result in increased mechanical pressure, eventually causing a new fracture of the endplate in the adjacent vertebral body [79]. More severe wedge angle before surgery, correction degree, old OVF presence, and thoracolumbar levels were identified as predictive factors of adjacent vertebral fracture in previous studies [65,82]. Furthermore, a change in Cobb angle after operation and diabetes have been reported as a risk factor for postoperative adjacent vertebral fracture [65]. A correction degree of > 10° was further reported as an independent risk factor for adjacent vertebral fracture [82]. Several papers [73,75,83] have shown that decreased bone mineral density (BMD) increases the risk of adjacent vertebral fracture following vertebroplasty. Furthermore, cement leakage has been reported as the primary risk factor for new vertebral compression fractures [79,84]. However, if the cement is not in close contact with the endplates, it does not increase endplate deformation in the adjacent vertebrae, thereby minimizing the risk of adjacent vertebral fracture [85]. Several studies have developed scoring systems to predict adjacent vertebral fracture based on the identified risk factors [82,86,87]. The usefulness of these scoring systems may be revealed in the future.
Most adjacent vertebral fractures heal by conservative treatment [82]. The application of smaller volumes of cement has been shown to be effective in decreasing the risk of adjacent vertebral fractures, while maintaining sufficient stability [88]. Prophylactic augmentation into non-fractured vertebra may be effective to prevent further fractures and minimize the risk of revision surgery in osteoporotic patients [89]. However, several studies indicated that the cause of adjacent fracture was mainly related to the progression of osteoporosis rather than the vertebral augmentation [90] and the efficacy is inconsistent across the studies. Recent meta-analysis suggested that prophylactic augmentation could not reduce the risk of revision surgery [91]. The therapeutic effects of teriparatide were better than those of the combined vertebroplasty and an antiresorptive agent in fracture prevention, BMD increase, and sustained pain relief [74]. However, considering that most of the adjacent vertebral fractures occur within a few months, and the effect of increasing BMD appeared at least 3 months after the start of teriparatide use [92], teriparatide should be administered at least before surgery. A randomized controlled trail [93] showed that teriparatide might prevent adjacent vertebral fracture due to stimulation of bone formation and faster improvement of bone strength and quality than antiresorptive agents. Teriparatide may offset the pharmacy cost due to the reduction of the inpatient admission and repeat vertebral augmentation [94]. In addition, a reduced BMD might be a surrogate marker in patients with reduced activity of daily living because mechanical loading can inhibit bone resorption and increase bone formation [95].
As the limitation of this study, the criteria for revision surgery is not consistent according to the study population and surgeon’s decision. The lack of uniform definition in a heterogeneous topic can limit the generalizability of the study findings. However, it is important to recognize the possibility and risk for revision surgery after vertebral augmentation in OVF. Furthermore, the follow-up period is relatively short, and the long-term outcomes of the revision surgery are not evaluated. Additionally, publication bias may exist in this review. The investigators who did not identify the revision cases might not submit their data. Finally, this study did not assess the cost-effectiveness of revision surgery, which could have provided valuable information for healthcare providers and policy makers.
There are numerous treatment strategies for OVFs, which remain controversial. Current reviews have documented the low level of evidence currently available to inform the treatment strategy based on the risk of vertebral augmentation. Therefore, it is necessary to carefully evaluate the fracture to determine all relevant surgical indications. In cases with a high risk of failure, other surgeries and conservative treatments should also be considered as treatment options. However, implant complications such as cage subsidence, screw loosening, pull-out, and junctional failure are common in older patients with osteoporosis. Therefore, further investigation is necessary to create treatment strategies for OVFs.
NOTES
Fig. 1.
Flow chart of the literature search for systematic review of revision surgery after vertebral augmentation. VA, vertebral augmentation.
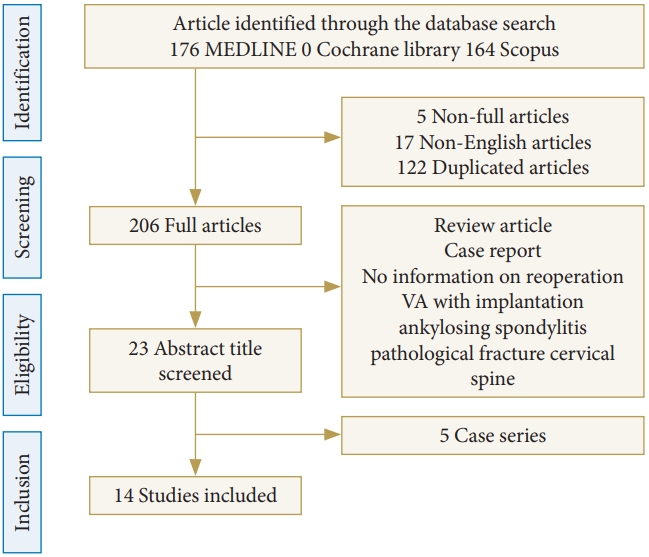
Fig. 2.
Random effects meta-analysis of the incidence of revision surgery after vertebral augmentation. CI, confidence interval.
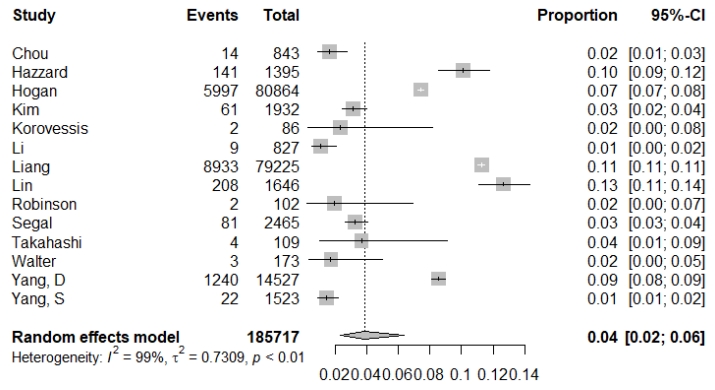
Table 1.
Demographic data and characteristics for revision surgery of the included studies
| Study | Study design | Study population | Procedure | Sample size | Age (yr) | Follow-up | Outcome | Revision rate | Author conclusion |
|---|---|---|---|---|---|---|---|---|---|
| Chou et al. [42] | Retrospective cohort study | Patients with VF in a single center | VP | 843 | 75 | > 2 Years | Revision | 1.70% | Location of fracture at the thoracolumbar junction, fracture type of intravertebral cleft, or wedge-type fracture, and material with nonintegrating properties injected into the fractured vertebra are risk factors associated with the occurrence of progressive kyphosis and neurological complications. |
| Hazzard et al. [43] | Retrospective propensity score-matched cohort study | Thomson Reuters MarketScan database | VP/KP | KP (n = 696), VP (n = 699) | 78 | 2 Years | Revision | VP 11.4%, KP 8.9% | KP and VP have equivalent long-term costs to nonsurgical management. |
| Hogan et al. [44] | Retrospective cohort study | PearlDiver | VP/KP | 80,864 | 73 | 1–5 Years | Revision | 15% | Patients with procedures performed by surgeons experienced lower odds of reoperation at 30 days and 1 year but the 5-year and overall rates were not significantly different. |
| Kim et al. [45] | Retrospective cohort analysis | ACS-NSQIP dataset | VP/KP | 1,932 | 74.9 | < 30 Days | Revision | 3.2% | Elevated creatinine levels and ASA PS classification grade IV were independently associated with mortality after VP/KP. |
| Korovessis et al. [34] | Controlled comparative randomized study | Patients with OVF in a hospital | KP | 86 | 72.3 | 14 Months | Salvage for cement leakage | 2.3% in KP | KIVA, which is a novel polyether ether ketone implant, was followed by significantly lower and harmless always extra canal leakage rate than balloon kyphoplasty. |
| Li et al. [35] | Retrospective cohort study | Patients with OVF in 2 hospitals | VP | 827 | 74.1 | 3 Months | Repeat VP | 1.1% | Repeat PV is an effective option for patients with OVFs with recurrent pain at the previously treated level. |
| Liang et al. [36] | Retrospective population-based longitudinal observation study | National Health Insurance Research Database of Taiwan | VP/KP | 79,225 | > 40 | 4–7 Years | Repeat VP/KP | 11.3% | Patients with the following characteristics were at a greater risk for repeat VP/KP: female sex, advanced age, diabetes mellitus, cerebrovascular disease, dementia, blindness or low vision, hypertension, and hyperlipidemia. Patients taking calcium/vitamin D, bisphosphonates, or calcitonin were less likely to undergo repeat VP/KP. |
| Lin et al. [37] | Retrospective cohort study | Patients with VF in a single center | VP | 1,646 | 76.7 | 1.16 Years | Repeat VP | 4%–13% | The results indicate that patients with osteoporosis who undergo VP are significantly less likely to require a reoperation if treated with zoledronic acid infusion. |
| Robinson et al. [33] | Prospective cohort study | Patients with VF in a single center | KP | 102 | 69 | 6 Months | Revision | 2.0% | Major complications are rare. However, since severe acute complications requiring emergency treatment may occur, the procedure should be performed by a qualified spinal surgeon. |
| Segal et al. [38] | Retrospective cohort study | Nationwide population | KP | 2,465 | 74 | 30 Days | Revision | 3.4% | Frailty was associated with increased total complications, Clavien-Dindo IV complications, length of stay, and 30-day readmission rates. |
| Takahashi et al. [39] | Prospective cohort study | Patients with OVF in multiple centers | KP | 109 | 74.0 | 6 Months | Revision | 3.8% | Split type fracture, angular motion ≥ 14°, and large endplate deficit increased the risk for revision surgery. |
| Walter et al. [40] | Retrospective cohort analysis | Patients with OVF in a single center | KP | 173 | Male, 70.1; Female, 77.8 | 6 Months | Salvage for cement leakage | 1.7% | KP can be considered a safe procedure, even in the treatment of painful OVFs of AO type A3.1. |
| Yang et al. [41] | Population-based medical claims database | Population-based medical claims database | VP/KP | 14,527 | 75 | 2 Years | Revision | 7.9% | PVP/PKP procedures for OVF place a high economic burden for both the healthcare system and patients. Early detection and treatment of patients with osteoporosis is critical in China. |
| Yang et al. [31] | Retrospective study | Patients with OVF in multiple centers | VP | 1,523 | 69.2 | NA | Revision | 1.4% | Combined anterior and posterior surgery seems to be the most secure salvage method to treat patients with severe osteoporosis in whom percutaneous VP initially failed. |
Table 2.
Evaluation of postintervention biases
| Study | Selection | Reporting |
|---|---|---|
| Chou et al. [42] | Moderate | Low |
| Hazzard et al. [43] | Moderate | Moderate |
| Hogan et al. [44] | Moderate | Moderate |
| Kim et al. [45] | Moderate | Moderate |
| Korovessis et al. [34] | Low | Low |
| Li et al. [35] | Moderate | Moderate |
| Liang et al. [36] | Moderate | Moderate |
| Lin et al. [37] | Moderate | Moderate |
| Robinson et al. [33] | Moderate | Low |
| Segal et al. [38] | Moderate | Moderate |
| Takahashi et al. [39] | Moderate | Low |
| Walter et al. [40] | Moderate | Moderate |
| Yang et al. [41] | Moderate | Moderate |
| Yang et al. [31] | Moderate | Moderate |
REFERENCES
1. Tosteson ANA, Gabriel SE, Grove MR, et al. Impact of hip and vertebral fractures on quality-adjusted life years. Osteoporos Int 2001;12:1042-9.



2. Ahmadi SA, Takahashi S, Hoshino M, et al. Association between MRI findings and back pain after osteoporotic vertebral fractures: a multicenter prospective cohort study. Spine J 2019;19:1186-93.


3. Inose H, Kato T, Ichimura S, et al. Factors affecting the quality of life in the chronic phase of thoracolumbar osteoporotic vertebral fracture managed conservatively with a brace. Spine J 2023;23:425-32.


4. Kado DM, Browner WS, Palermo L, et al. Vertebral fractures and mortality in older women: a prospective study. Arch Intern Med 1999;159:1215-20.


5. Lorentzon M, Johansson H, Harvey NC, et al. Osteoporosis and fractures in women: the burden of disease. Climacteric 2022;25:4-10.


6. Lippuner K, Rimmer G, Stuck AK, et al. Hospitalizations for major osteoporotic fractures in Switzerland: a long-term trend analysis between 1998 and 2018. Osteoporos Int 2022;33:2327-35.




7. Abtahi S, Driessen JHM, Vestergaard P, et al. Secular trends in major osteoporotic fractures among 50+ adults in Denmark between 1995 and 2010. Arch Osteoporos 2018;13:1-7.
8. Malik AT, Retchin S, Phillips FM, et al. Declining trend in osteoporosis management and screening following vertebral compression fractures - a national analysis of commercial insurance and medicare advantage beneficiaries. Spine J 2020;20:538-46.


9. Funayama T, Tatsumura M, Fujii K, et al. Therapeutic effects of conservative treatment with 2-week bed rest for osteoporotic vertebral fractures: a prospective cohort study. J Bone Joint Surg Am 2022;104:1785-95.

10. Sinaki M, Pfeifer M, Preisinger E, et al. The role of exercise in the treatment of osteoporosis. Curr Osteoporos Rep 2010;8:138-44.



11. Sinaki M, Mikkelsen BA, Beth A. Postmenopausal spinal osteoporosis: flexion versus extension exercises. Arch Phys Med Rehabil 1984;65:593-6.

12. Kato T, Inose H, Ichimura S, et al. Comparison of rigid and soft-brace treatments for acute osteoporotic vertebral compression fracture: a prospective, randomized, multicenter study. J Clin Med 2019;8:198.



13. Takahashi S, Hoshino M, Takayama K, et al. Predicting delayed union in osteoporotic vertebral fractures with consecutive magnetic resonance imaging in the acute phase: a multicenter cohort study. Osteoporos Int 2016;27:3567-75.



14. Hoshino M, Nakamura H, Terai H, et al. Factors affecting neurological deficits and intractable back pain in patients with insufficient bone union following osteoporotic vertebral fracture. Eur Spine J 2009;18:1279-86.




15. Ensrud KE, Black DM, Harris F, et al. Correlates of kyphosis in older women. J Am Geriatr Soc 1997;45:682-7.


16. Inose H, Kato T, Ichimura S, et al. Factors contributing to residual low back pain after osteoporotic vertebral fractures. J Clin Med 2022;11:1566.



17. Clark W, Bird P, Gonski P, et al. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet 2016;388:1408-16.


18. Hoshino M, Takahashi S, Yasuda H, et al. Balloon kyphoplasty versus conservative treatment for acute osteoporotic vertebral fractures with poor prognostic factors: propensity score matched analysis using data from two prospective multicenter studies. Spine (Phila Pa 1976) 2019;44:110-7.

19. Wardlaw D, Cummings SR, Van Meirhaeghe J, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet 2009;373:1016-24.


20. Hulme PA, Krebs J, Ferguson SJ, et al. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine (Phila Pa 1976) 2006;31:1983-2001.


21. Galivanche AR, Toombs C, Adrados M, et al. Cement augmentation of vertebral compression fractures may be safely considered in the very elderly. Neurospine 2021;18:226-33.




22. Edidin AA, Ong KL, Lau E, et al. Mortality risk for operated and nonoperated vertebral fracture patients in the medicare population. J Bone Miner Res 2011;26:1617-26.


23. Buchbinder R, Johnston RV, Rischin KJ, et al. Percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Cochrane Database Syst Rev 2018;4:CD006349.


24. Inose H, Kato T, Shirasawa S, et al. Time course of acute vertebral fractures: a prospective multicenter cohort study. J Clin Med 2021;10:5961.



25. Takahashi S, Hoshino M, Terai H, et al. Differences in short-term clinical and radiological outcomes depending on timing of balloon kyphoplasty for painful osteoporotic vertebral fracture. J Orthop Sci 2018;23:51-6.


26. Minamide A, Maeda T, Yamada H, et al. Early versus delayed kyphoplasty for thoracolumbar osteoporotic vertebral fractures: the effect of timing on clinical and radiographic outcomes and subsequent compression fractures. Clin Neurol Neurosurg 2018;173:176-81.


27. McGraw JK, Cardella J, Barr JD, et al. Society of interventional radiology quality improvement guidelines for percutaneous vertebroplasty. J Vasc Interv Radiol 2003;14(9 Pt 2):S311-5.


28. Pflugmacher R, Schroeder RJ, Klostermann CK. Incidence of adjacent vertebral fractures in patients treated with balloon kyphoplasty: two years' prospective follow-up. Acta radiol 2006;47:830-40.



29. Baumann C, Fuchs H, Kiwit J, et al. Complications in percutaneous vertebroplasty associated with puncture or cement leakage. Cardiovasc Intervent Radiol 2007;30:161-8.



30. Yang SC, Chen HS, Kao YH, et al. Clinical evaluation of percutaneous vertebroplasty for symptomatic adjacent vertebral compression fracture. J Spinal Disord Tech 2013;26:E130-6.


31. Yang SC, Chen WJ, Yu SW, et al. Revision strategies for complications and failure of vertebroplasties. Eur Spine J 2008;17:982-8.




32. Park JW, Park SM, Lee HJ, et al. Infection following percutaneous vertebral augmentation with polymethylmethacrylate. Arch Osteoporos 2018;13:47.



33. Robinson Y, Tschöke SK, Stahel PF, et al. Complications and safety aspects of kyphoplasty for osteoporotic vertebral fractures: a prospective follow-up study in 102 consecutive patients. Patient Saf Surg 2008;2:2.




34. Korovessis P, Vardakastanis K, Repantis T, et al. Balloon kyphoplasty versus KIVA vertebral augmentation-comparison of 2 techniques for osteoporotic vertebral body fractures: a prospective randomized study. Spine (Phila Pa 1976) 2013;38:292-9.

35. Li L, Lu Y, Li M, et al. Repeat percutaneous vertebroplasty for recurrent pain arising from previously treated vertebrae in patients with osteoporotic vertebral compression fractures. Clin Spine Surg 2016;29:399-404.


36. Liang C, Wang HK, Syu FK, et al. Repeated vertebral augmentation for new vertebral compression fractures of postvertebral augmentation patients: a nationwide cohort study. Clin Interv Aging 2015;10:635-42.


37. Lin TY, Yang SC, Tsai TT, et al. Correlation between zoledronic acid infusion and repeat vertebroplasty surgery in osteoporotic patients. Curr Med Res Opin 2016;32:921-7.


38. Segal DN, Wilson JM, Staley C, et al. The 5-item modified frailty index is predictive of 30-day postoperative complications in patients undergoing kyphoplasty vertebral augmentation. World Neurosurg 2018;116:e225-31.


39. Takahashi S, Hoshino M, Yasuda H, et al. Characteristic radiological findings for revision surgery after balloon kyphoplasty. Sci Rep 2019;9:18513.




40. Walter J, Haciyakupoglu E, Waschke A, et al. Cement leakage as a possible complication of balloon kyphoplasty--is there a difference between osteoporotic compression fractures (AO type A1) and incomplete burst fractures (AO type A3.1)? Acta Neurochir (Wien) 2012;154:313-9.



41. Yang D, Zhang Y, Ma X, et al. Resources utilisation and economic burden of percutaneous vertebroplasty or percutaneous kyphoplasty for treatment of osteoporotic vertebral compression fractures in China: a retrospective claim database study. BMC Musculoskelet Disord 2020;21:255.




42. Chou KN, Lin BJ, Wu YC, et al. Progressive kyphosis after vertebroplasty in osteoporotic vertebral compression fracture. Spine (Phila Pa 1976) 2014;39:68-73.


43. Hazzard MA, Huang KT, Toche UN, et al. Comparison of vertebroplasty, kyphoplasty, and nonsurgical management of vertebral compression fractures and impact on us healthcare resource utilization. Asian Spine J 2014;8:605-14.



44. Hogan WB, Philips A, Alsoof D, et al. Kyphoplasty and vertebroplasty performed by surgeons versus nonsurgeons: trends in procedure rates, complications, and revisions. World Neurosurg 2022;164:e518-24.


45. Kim HJ, Zuckerman SL, Cerpa M, et al. Incidence and risk factors for complications and mortality after vertebroplasty or kyphoplasty in the osteoporotic vertebral compression fracture—analysis of 1,932 cases from the american college of surgeons national surgical quality improvement. Glob Spine J 2022;12:1125-34.


46. Stijnen T, Hamza TH, Özdemir P. Random effects meta-analysis of event outcome in the framework of the generalized linear mixed model with applications in sparse data. Stat Med 2010;29:3046-67.


47. Trout AT, Kallmes DF, Lane JI, et al. Subsequent vertebral fractures after vertebroplasty: association with intraosseous clefts. AJNR Am J Neuroradiol 2006;27:1586-91.


48. Fahim DK, Sun K, Tawackoli W, et al. Premature adjacent vertebral fracture after vertebroplasty: a biomechanical study. Neurosurgery 2011;69:733-44.



49. Ha KY, Lee JS, Kim KW, et al. Percutaneous vertebroplasty for vertebral compression fractures with and without intravertebral clefts. J Bone Joint Surg Br 2006;88:629-33.



50. Genant HK, Wu CY, van Kuijk C, et al. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 1993;8:1137-48.


51. Vaccaro AR, Oner C, Kepler CK, et al. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976) 2013;38:2028-37.

52. Mozaffari K, Foster CH, Rosner MK. Practical use of augmented reality modeling to guide revision spine surgery: an illustrative case of hardware failure and overriding spondyloptosis. Oper Neurosurg (Hagerstown) 2022;23:212-6.



53. He D, Lou C, Yu W, et al. Cement distribution patterns are associated with recompression in cemented vertebrae after percutaneous vertebroplasty: a retrospective study. World Neurosurg 2018;120:e1-7.


54. Ma YH, Tian ZS, Liu HC, et al. Predictive risk factors for recollapse of cemented vertebrae after percutaneous vertebroplasty: a meta-analysis. World J Clin Cases 2021;9:2778-90.



55. Ye LQ, Liang D, Jiang XB, et al. Risk factors for the occurrence of insufficient cement distribution in the fractured area after percutaneous vertebroplasty in osteoporotic vertebral compression fractures. Pain Physician 2018;21:E33-42.

56. Chang MC, Liu CL, Chen TH. Polymethylmethacrylate augmentation of pedicle screw for osteoporotic spinal surgery: a novel technique. Spine (Phila Pa 1976) 2008;33:E317-24.

57. Chiu YC, Yang SC, Chen HS, et al. Posterior transpedicular approach with circumferential debridement and anterior reconstruction as a salvage procedure for symptomatic failed vertebroplasty. J Orthop Surg Res 2015;10:28.




58. Li Y, Tan Z, Cheng Y, et al. High-viscosity versus low-viscosity cement for the treatment of vertebral compression fractures: a meta-analysis of randomized controlled trials. Medicine (Baltimore) 2022;101:e31544.



59. Tsoumakidou G, Too CW, Koch G, et al. CIRSE guidelines on percutaneous vertebral augmentation. Cardiovasc Intervent Radiol 2017;40:331-42.



61. Krueger A, Bliemel C, Zettl R, et al. Management of pulmonary cement embolism after percutaneous vertebroplasty and kyphoplasty: a systematic review of the literature. Eur Spine J 2009;18:1257-65.




62. Park SY, Modi HN, Suh SW, et al. Epidural cement leakage through pedicle violation after balloon kyphoplasty causing paraparesis in osteoporotic vertebral compression fractures - a report of two cases. J Orthop Surg Res 2010;5:54.




63. Martin DJ, Rad AE, Kallmes DF. Prevalence of extravertebral cement leakage after vertebroplasty: procedural documentation versus CT detection. Acta Radiol 2012;53:569-72.



64. Zhan Y, Jiang J, Liao H, et al. Risk factors for cement leakage after vertebroplasty or kyphoplasty: a meta-analysis of published evidence. World Neurosurg 2017;101:633-42.


65. Chen C, Fan P, Xie X, et al. Risk factors for cement leakage and adjacent vertebral fractures in kyphoplasty for osteoporotic vertebral fractures. Clin Spine Surg 2020;33:E251-5.


66. Abdelgawaad AS, Ezzati A, Govindasamy R, et al. Kyphoplasty for osteoporotic vertebral fractures with posterior wall injury. Spine J 2018;18:1143-8.


67. Nieuwenhuijse MJ, Van Erkel AR, Dijkstra PD. Cement leakage in percutaneous vertebroplasty for osteoporotic vertebral compression fractures: identification of risk factors. Spine J 2011;11:839-48.


68. Chen W, Xie W, Xiao Z, et al. Incidence of cement leakage between unilateral and bilateral percutaneous vertebral augmentation for osteoporotic vertebral compression fractures: a meta-analysis of randomized controlled trials. World Neurosurg 2019;122:342-8.


69. Lee MJ, Dumonski M, Cahill P, et al. Percutaneous treatment of vertebral compression fractures: a meta-analysis of complications. Spine (Phila Pa 1976) 2009;34:1228-32.

70. Daher M, Kreichati G, Kharrat K, et al. Vertebroplasty versus kyphoplasty in the treatment of osteoporotic vertebral compression fractures: a meta-analysis. World Neurosurg 2023;171:65-71.


71. Zhu JJ, Zhang DS, Lou SL, et al. Surgical treatment of secondary fractures after percutaneous vertebroplasty: a retrospective study. Indian J Orthop 2017;51:269-72.




72. Campbell PG, Harrop JS. Incidence of fracture in adjacent levels in patients treated with balloon kyphoplasty: a review of the literature. Curr Rev Musculoskelet Med 2008;1:61-4.



73. Lu K, Liang CL, Hsieh CH, et al. Risk factors of subsequent vertebral compression fractures after vertebroplasty. Pain Med 2012;13:376-82.


74. Su CH, Tu PH, Yang TC, et al. Comparison of the therapeutic effect of teriparatide with that of combined vertebroplasty with antiresorptive agents for the treatment of new-onset adjacent vertebral compression fracture after percutaneous vertebroplasty. J Spinal Disord Tech 2013;26:200-6.


75. Takahara K, Kamimura M, Moriya H, et al. Risk factors of adjacent vertebral collapse after percutaneous vertebroplasty for osteoporotic vertebral fracture in postmenopausal women. BMC Musculoskelet Disord 2016;17:1-7.




76. Staples MP, Howe BM, Ringler MD, et al. New vertebral fractures after vertebroplasty: 2-year results from a randomised controlled trial. Arch Osteoporos 2015;10:2-11.


77. Li YA, Lin CL, Chang MC, et al. Subsequent vertebral fracture after vertebroplasty: incidence and analysis of risk factors. Spine (Phila Pa 1976) 2012;37:179-83.

78. Lee KA, Hong SJ, Lee S, et al. Analysis of adjacent fracture after percutaneous vertebroplasty: does intradiscal cement leakage really increase the risk of adjacent vertebral fracture? Skeletal Radiol 2011;40:1537-42.



79. Lin EP, Ekholm S, Hiwatashi A, et al. Vertebroplasty: cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. Am J Neuroradiol 2004;25:175-80.


80. Civelek E, Cansever T, Yilmaz C, et al. The retrospective analysis of the effect of balloon kyphoplasty to the adjacent-segment fracture in 171 patients. J Spinal Disord Tech 2014;27:98-104.


81. Fourney DR, Schomer DF, Nader R, et al. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg 2003;98:21-30.

82. Takahashi S, Hoshino M, Yasuda H, et al. Development of a scoring system for predicting adjacent vertebral fracture after balloon kyphoplasty. Spine J 2019;19:1194-201.


83. Syed MI, Patel NA, Jan S, et al. Intradiskal extravasation with low-volume cement filling in percutaneous vertebroplasty. AJNR Am J Neuroradiol 2005;26:2397-401.


84. Rho YJ, Choe WJ, Chun YI. Risk factors predicting the new symptomatic vertebral compression fractures after percutaneous vertebroplasty or kyphoplasty. Eur Spine J 2012;21:905-11.



85. Hulme PA, Boyd SK, Heini PF, et al. Differences in endplate deformation of the adjacent and augmented vertebra following cement augmentation. Eur Spine J 2009;18:614-23.




86. Hijikata Y, Kamitani T, Itaya T, et al. Development and internal validation of a clinical prediction model for acute adjacent vertebral fracture after vertebral augmentation: the AVA score. Bone Joint J 2022;104-B:97-102.

87. Li Q, Long X, Wang Y, et al. Development and validation of a nomogram for predicting the probability of new vertebral compression fractures after vertebral augmentation of osteoporotic vertebral compression fractures. BMC Musculoskelet Disord 2021;22:957.




88. Ryu KS, Park CK, Kim MC, et al. Dose-dependent epidural leakage of polymethylmethacrylate after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Neurosurg 2002;96:56-61.


89. Diel P, Freiburghaus L, Röder C, et al. Safety, effectiveness and predictors for early reoperation in therapeutic and prophylactic vertebroplasty: short-term results of a prospective case series of patients with osteoporotic vertebral fractures. Eur Spine J 2012;21 Suppl 6(Suppl 6):S792-9.



90. Zhang H, Xu C, Zhang T, et al. Does percutaneous vertebroplasty or balloon kyphoplasty for osteoporotic vertebral compression fractures increase the incidence of new vertebral fractures? A meta-analysis. Pain Physician 2017;20:E13-28.


91. Chen Z, Song C, Lin H, et al. Does prophylactic vertebral augmentation reduce the refracture rate in osteoporotic vertebral fracture patients: a meta-analysis. Eur Spine J 2021;30:2691-7.



92. Body JJ, Gaich GA, Scheele WH, et al. A randomized double-blind trial to compare the efficacy of teriparatide [recombinant human parathyroid hormone (1-34)] with alendronate in postmenopausal women with osteoporosis. J Clin Endocrinol Metab 2002;87:4528-35.



93. Tseng YY, Su CH, Lui TN, et al. Prospective comparison of the therapeutic effect of teriparatide with that of combined vertebroplasty with antiresorptive agents for the treatment of new-onset adjacent vertebral compression fracture after percutaneous vertebroplasty. Osteoporos Int 2012;23:1613-22.



- TOOLS
- Related articles in NS
-
Journal Impact Factor 3.2



























