|
 |
- Search
|
|
||
Abstract
The management of osteoporotic vertebral fractures (OVFs) in the elderly includes nonoperative treatment and vertebroplasty, but has not been established due to the diversity of patient backgrounds. The purpose of this study was to compare the impact of 3 treatment modalities for the management of OVF: orthotic treatment, percutaneous vertebroplasty (PVP), and balloon kyphoplasty (BKP). The method was based on an analysis of the latest RCTs, meta-analyses, and systematic reviews on these topics. No study showed a benefit of bracing with high level of evidence. Trials were found that showed comparable outcomes without orthotic treatment. Only 1 randomized controlled trial (RCT) showed an improvement in pain relief up to 6 months compared with no orthosis. Rigid and nonrigid orthoses were equally effective. Four of 5 RCTs comparing vertebroplasty and sham surgery were equally effective, and one RCT showed superior pain relief with vertebroplasty within 3 weeks of onset. In open trials comparing vertebroplasty with nonoperative management, vertebroplasty was superior. PVP and BKP were comparable in terms of pain relief, improvement in quality of life, and adjacent vertebral fractures. BKP does not affect global sagittal alignment, although BKP may restore vertebral body height. An RCT was published showing that PVP was effective in chronic cases without pain relief. Vertebroplasty improved life expectancy by 22% at 10 years. The superiority of orthotic therapy for OVF was seen only in short-term pain relief. Soft orthoses proved to be a viable alternative to rigid orthoses. Vertebroplasty within 3 weeks may be useful. There is no significant difference in clinical efficacy between PVP and BKP. Vertebroplasty improves life expectancy.
Osteoporotic vertebral fractures (OVFs) is a common disease with a large number of patients in an aging society, but its treatment is controversial [1,2]. The reasons include the following: vertebral fractures may be painful or unnoticeable to the patient (accounting for about one-third of fractures), healing is often achieved by rest and external fixation after fracture, some rare patients may develop neurological symptoms or kyphosis without healing, and patients may be elderly and in various general conditions. Patients are elderly and their general condition varies widely. The treatment of OVF varies greatly depending on the institution and the initial treating physician, including whether the patient is treated on an outpatient or inpatient basis, with or without external fixation, external fixation methods, medications, surgical intervention, and surgical procedures. The purpose of this study is to analyze the most recent systematic review and meta-analysis of orthotics and vertebroplasty for OVFs and to discuss current evidence-based recommendations.
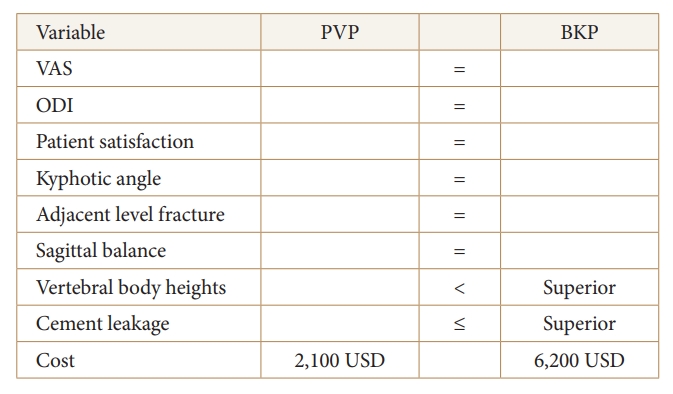
When considering the management of OVFs, the morphologic classification proposed by the Working Group ŌĆ£Osteoporotic FracturesŌĆØ of the Spine Section of the German Society of Orthopaedics and Trauma (DGOU) is considered a useful classification [3] (Fig. 1). Its development process follows the concept of validation of fracture classification by Audige et al. [4] and is considered reliable and reproducible. Based on this classification, it is described that OF4 and OF5 are clear indications for surgical treatment, OF3 is indicated for surgical or conservative treatment, and OF1 and OF2 are indicated for conservative treatment. Although the morphological OF classification of the DGOU group is very useful, we present our classification in consideration of fracture age and clinical symptoms (Fig. 2).
Immediately after fracture, pain during movement is the most intense, not only in sitting, but also in turning over or coughing, in which case the patient is almost bedridden.
The pain of the acute phase is relieved, but the fractured vertebrae have not yet fused, and back pain occurs with each change in posture, such as sitting or standing. Pain is relieved with rest, such as lying down.
Progressive disintegration of the vertebral body causes the posterior wall fragments of the fractured body to protrude into the spinal canal, resulting in neuropathy due to direct compression of nerve tissue or indirect compression due to vertebral instability.
The fractured vertebrae become significantly wedged and fuse in a kyphotic deformity, shifting the sagittal balance forward, causing severe postural back pain originating from the erector spinae, and sometimes difficulty in holding a standing position. The significant kyphosis deformity may cause gastrointestinal and respiratory symptoms due to thoracoabdominal pressure. Section headings 3 (delayed neurological deficit) and 4 (kyphotic deformity type) may coexist.
This paper discusses treatment options for section headings 1 (acute phase with severe pain) and 2 (subacute phase, with vertebral instability) above, specifically orthotics and vertebroplasty.
Previous reviews of the use of orthoses in OVF have recommended the use of spinal orthoses, but the level of evidence is low [5,6].
The analysis of Pieroh et al. [7] from 13 studies (n= 5 randomized controlled trials, n = 3 nonrandomized controlled trials, n= 5 uncontrolled prospective studies) and 8 systematic reviews, found that 5 uncontrolled prospective studies found improvements in pain, function, and quality of life during follow-up.
Studies comparing different types of orthoses favor nonrigid orthoses. Of the 5 studies comparing orthotic and nonorthotic patients, 3 studies failed to detect a beneficial effect of orthotic treatment over nonorthotic treatment, and 2 industry-sponsored studies reported significant improvement with orthotic wear. Wearing an orthosis, regardless of type, did not result in significant improvements in quality of life, pain, reduction in increased x-ray pressure, or minimization of opioid use compared to patients who did not wear an orthosis. Although the level of evidence is not high, no definitive recommendations can be made regarding the use of spinal orthoses.
In addition, a meta-analysis by Squires et al. [8] of three studies evaluating orthotic therapy for thoracic and lumbar compression fractures (a total of 447 patients [96% female] in a randomized trial) found that 54 patients were treated without orthoses and 393 were treated with orthoses (195 rigid and 198 soft). Moderate-quality evidence indicated that rigid bracing for vertebral compression fractures may significantly reduce pain up to 6 months after injury compared with no bracing (standardized mean difference= -1.32, 95% confidence interval [CI], -1.89 to -0.76, p < 0.05, I2= 41%) (Fig. 3).
However, this trend was attenuated after 48 weeks of long-term follow-up. There were no significant differences in radiographic kyphosis, opioid use, function, or quality of life at any time point. Rigid orthoses may put patients at risk for dyspnea and pressure ulcers and have low compliance rates. Given that both rigid and soft orthoses significantly reduced pain at 6 months, soft orthoses may be an alternative method to rigid orthoses [8-17].
Vertebroplasty has been the treatment of painful OVFs for the past 30 years, but there is much debate about its usefulness [18-21]. There are many comparative trials of vertebroplasty, but awareness of what is being compared is very important in interpreting them, as the meaning of the trial will depend on the choice of the intervention being compared [22].
Most open trials comparing vertebroplasty with usual care concluded that vertebroplasty was superior, but sensitivity analyses confirmed that these are likely to have overestimated any benefit of vertebroplasty. Correcting for these biases might drive any benefits observed with vertebroplasty towards the null.
While 4 of the 5 trials comparing vertebroplasty to placebo surgery failed to show significant differences between the groups, and in the remaining one, when performed primarily only within 3 weeks of fracture occurrence, vertebroplasty was shown to be more effective than placebo (Fig. 4). At present, only a blinded randomized trial comparing sham surgery to early vertebroplasty in patients with acute osteoporotic fractures with severe pain might demonstrate a benefit in relieving pain [23].
A systematic review by Halvachizadeh et al. [24] focused on RCTs and examined differences in outcomes (e.g., pain relief, adjacent level fractures, quality of life) between vertebroplasty and nonoperative therapy. Patients were assigned to 3 groups according to treatment: percutaneous vertebroplasty (PVP), balloon kyphoplasty (BKP), and nonoperative management (NOM). Short-term (weeks), medium-term (months), and long-term (more than one year) effects were compared; 16 trials were included; 11 (68.8%) compared PVP to NOM, 1 (6.3%) compared BKP to NOM, and 4 (25.0%) compared BKP to PVP. At short-term follow-up, pain improvement was 1.31 points (95% CI, 0.41ŌĆō2.21; p < 0.001) better when PVP was compared to NOM. The pain effect was similar for PVP and BKP (difference at midterm, 0.0 point; 95% CI, -0.25 to 0.25). The risk of adjacent level fracture did not increase after either treatment (log OR, -0.16; 95% CI, -0.83 to 0.5; NOM vs. PVP or BKP). Quality of life, as measured by RDQ, was not significantly different between the PVP or BKP and NOM groups except in the short term. This meta-analysis also provides evidence in support of vertebroplasty for OVF [24]. Vertebroplasty was associated with greater improvement in pain but was unrelated to the occurrence of adjacent level fractures or quality of life. Improvement in sagittal balance after surgery has not been well reported, but improvement in pain may justify vertebroplasty.
A meta-analysis of 6 studies with data from a total of 644 patients (330 in the PVP group and 284 in the BKP group) comparing PVP and BKP showed that the visual analogue scale (VAS) score (mean difference [MD]= 0.17; 95% CI, -0.39 to 0.73; p = 0.56), risk of cement leakage (odds ratio [OR], 1.31; 95% CI, 0.62ŌĆō2.74; p = 0.47), and Oswestry Disability Index (ODI) score (MD = 0.51; 95% CI, -1.87 to 2.88; p = 0.68) were not significantly different between the 2 groups. However, the volume of cement injected in the VP group (MD = -0.52; 95% CI, -0.88 to -0.15; p = 0.005) had a significantly lower statistically significant trend compared to the KP group, which may indicate a bias in favor of PVP regarding the risk of cement leakage.
Further high-quality multicenter randomized controlled trials with longer follow-up and larger sample sizes are needed, but at this time indicate that there are no significant differences between PVP and BKP in terms of VAS score, ODI score, or cement leakage, and that both are useful treatments for patients with OVF [25-34].
On the other hand, a systematic review comparing BKP and PVP, focusing on the primary outcome of height restoration and the secondary outcomes of pain relief and function (33 total randomized controlled trials; 20 BKP, 7 PVP, and 6 comparing PVP to BKP), suggested that BKP may be superior in restoring vertebral height, but both procedures restored some vertebral height reduction, kyphosis, Cobb angle, and wedge angle, and showed benefit in pain reduction and patient-reported functional improvement. However, it is not possible to definitively conclude whether BKP or PVP is superior in reducing pain and restoring function because many studies that examined all 3 variables did not report statistically significant results, and more definitive studies and data analysis are needed to confirm this finding (Figs. 5ŌĆō7) [35-43].
Although a meta-analysis by Daher et al. [36] also showed favorable recovery of vertebral body height after KP surgery, the improvement in kyphosis angle was not statistically significant between the PVP and BKP groups [37]. A systematic review by Najjar et al. [44] of the effect of BKP on sagittal balance shows that it does not affect sagittal balance. This review evaluated the relevant literature on the effect of BKP on global spinal sagittal alignment. Radiological parameters included pelvic incidence (PI), pelvic tilt (PT), lumbar lordosis (LL), thoracic kyphosis (TK), sagittal vertical axis (SVA), spinosacral angle (SSA). A statistical analysis comparing the pre/postoperative global sagittal alignment (111 patients, 3 studies with standard deviations) showed no statistical difference in PT (24.1┬░ vs. 23.5┬░, p = 0.93), TK (42.3┬░ vs. 42.4┬░, p = 0.57), PI-LL (14.4┬░ vs. 12.4┬░, p = 0.4), SVA (6.1 cm vs. 5.5 cm, p = 0.19), SSA (114.8┬░ vs. 116.7┬░, p = 0.36). BKP did not significantly affect overall sagittal alignment in patients with osteoporotic vertebral compression fractures.
There is debate as to whether different time frames for cement augmentation affect clinical outcomes. A comprehensive systematic review of 11 studies aimed at comparing pain relief and complication rates between early and late cement augmentation was conducted. Two analyses were conducted: 1 study grouped patients into ŌĆ£earlyŌĆØ and ŌĆ£lateŌĆØ groups based on a cutoff period of 2 to 4 weeks (Analysis 1), and the other study grouped patients into ŌĆ£earlyŌĆØ and ŌĆ£lateŌĆØ groups using 6 to 8 weeks as the cutoff (Analysis 2). The total number of cohorts was 712 for Analysis 1 and 775 for Analysis 2. Mean follow-up was 12.9┬▒ 3.7 months and 11┬▒ 0.6 months, respectively. The change in VAS at the final follow-up was significantly greater in the early group in both analyses (MD = -0.5 and -0.5, respectively) (MD = -0.66, p = 0.01; MD = -1.18, p < 0.005, respectively). There were no significant differences in postoperative VAS absolute scores, number of cement leaks, number of adjacent compression fractures, or local kyphosis angles in both analyses. Both groups had a decrease in VAS score that exceeded the minimum clinically important difference. In conclusion, postoperative absolute pain scores, kyphosis angles, cement leakage, and adjacent vertebral fractures were similar. Early surgery may provide substantial pain relief in patients presenting with pain as early as 2 to less than 4 weeks after VCF onset, according to the author Similarly, we have not found a consensus on the appropriate surgical timing of BKP.
With regard to the relationship between timing of BKP and clinical outcomes, a latest systematic review and meta-analysis of 13 studies concluded that early BKP intervention was associated with similar or better outcomes in terms of pain relief, functional improvement, restoration of vertebral height, and correction of kyphosis deformity when compared to delayed BKP intervention [45]. A meta-analysis showed no significant difference in cement leak rates between early and late BKP (OR, 1.60; 95% CI, 0.97ŌĆō2.64; p = 0.07), while delayed BKP was associated with a higher risk of adjacent vertebral fracture than early BKP (OR, 0.31; 95% CI, 0. 13ŌĆō0.76; p = 0.01). Early BKP may achieve similar or better clinical and radiological outcomes in the treatment of OVF compared to delayed BKP. Furthermore, early BKP interventions had a lower incidence of adjacent vertebral fractures and a similar incidence of cement leakage compared to delayed BKP. Based on current evidence, early BKP intervention may be more beneficial to patients.
Current treatment algorithms based on established appropriateness criteria may change recommendations to support early vertebral augmentation for the most clinically challenging OVF.
Although the prevailing opinion has been that VP is not useful in the chronic phase of OVF, the results of a prospective randomized clinical trial on the usefulness of VP in the chronic phase have recently been reported (VERTOS V). The primary outcome was pain severity, assessed by VAS (range, 0ŌĆō10) at 12 months after treatment. Secondary outcomes were quality of life and disability.
Patients were randomized to VP or anesthesia-only infusion. The results showed that the VP group was superior to the local anesthetic group in pain relief and improvement in quality of life, although both groups were similar in disability at 12 months [46].
The pain of most patients in the chronic phase of OVF originates from poor spinal alignment or kyphotic deformity, and not all are considered eligible for treatment. of this study. The patient background is relatively young, around 70 years of age, with a VAS of at least 7 points and bone marrow edema on MRI, and the indication for VP for patients in the chronic phase should be fully considered.
According to a meta-analysis of 19 studies reporting mortality and morbidity after VP/BKP in patients with OVF, compared to NOM, VP/BKP reduces the 12-month risk of all-cause mortality and morbidity by 19% and 36%, respectively. Moreover, VP/BKP reduces by 77% the 12-month risk of infection from any origin [47]. A meta-analysis by Hinde et al. [48] summarizing 16 references comparing mortality outcomes in patients with OVF treated with vertebroplasty versus NOM found that of the 16 included studies, 8 showed a benefit, 7 showed no difference in mortality, and 1 had mixed results. A meta-analysis of more than 2 million patients with OVF (vertebroplasty= 382,070, NOM= 1,707,874) found a pooled HR of 0.78 (95% CI, 0.66ŌĆō0.92; p = 0.003) comparing vertebroplasty with NOM, mortality was improved at 2 and 5 years (HR, 0.70; 95% CI, 0.69ŌĆō0.71; p < 0.001; and HR, 0.79; 95% CI, 0.62ŌĆō0.9999; p = 0.05; respectively). BKP was more beneficial than PVP in reducing mortality, with HRs of 0.77 (95% CI, 0.77ŌĆō0.78; p < 0.001) and 0.87 (95% CI, 0.87ŌĆō0.88; p < 0.001), respectively. In conclusion, in a meta-analysis of more than 2 million patients, patients with OVF who underwent vertebroplasty were 22% less likely to die up to 10 years after treatment than those who received NOM.
NOTES
Fig.┬Ā1.
The osteoporotic fracture classification (OF classification) proposed by the Spine Section of the German Society of Orthopedics and Trauma (DGOU) [3]. OF1: X-ray and computed tomography scans show no spinal deformity, and only MRI-STIR sequences clearly show vertebral edema. OF2: Minor deformity with no or less than 1/5 posterior wall involvement and fracture of only one endplate. OF1 and OF2 are stable injuries. OF3: Deformity with more than 1/5 posterior wall damage. Damage to the anterior and posterior walls that can be called incomplete ruptured fractures. Fractures may be unstable. OF4: Loss of the vertebral frame structure, vertebral body collapse, pincer-type fracture. OF5: Injuries with distraction or rotation. MRI-STIR, magnetic resonance imaging short inversion time inversion recovery.
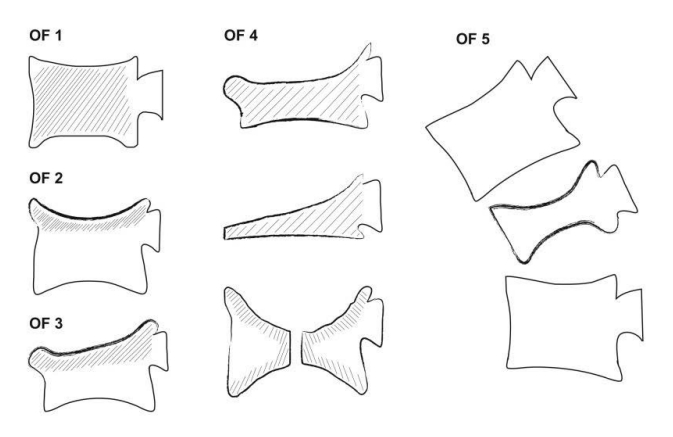
Fig.┬Ā2.
ŌæĀ Acute phase with severe pain. Severe pain occurs immediately after onset of symptoms and difficulty in moving the body. ŌæĪ Subacute phase, with vertebral instability. Back pain always occurs during body movement, although the acute pain has improved slightly. Ōæó Delayed neurological deficit Delayed onset of neurological symptoms in the lower extremities sometime after fracture. ŌæŻ Kyphotic deformity type A kyphotic deformity resulting in musculoskeletal pain in the back.
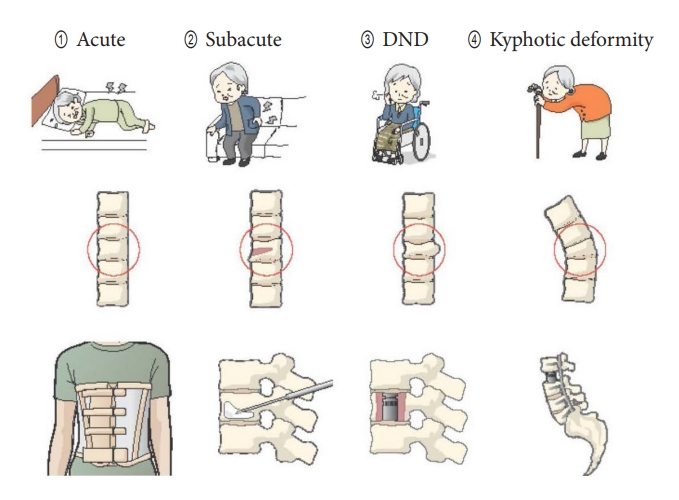
Fig.┬Ā3.
Subgroup analysis Forest plot for standardized mean difference in pain up to 6-month postinjury between brace (rigid and soft) and no brace groups. Statistically significant decrease in pain in patients treated with any brace compared to those treated with no brace [8]. SD, standard deviation; IV, inverse variance; df, degrees of freedom; CI, confidence interval.
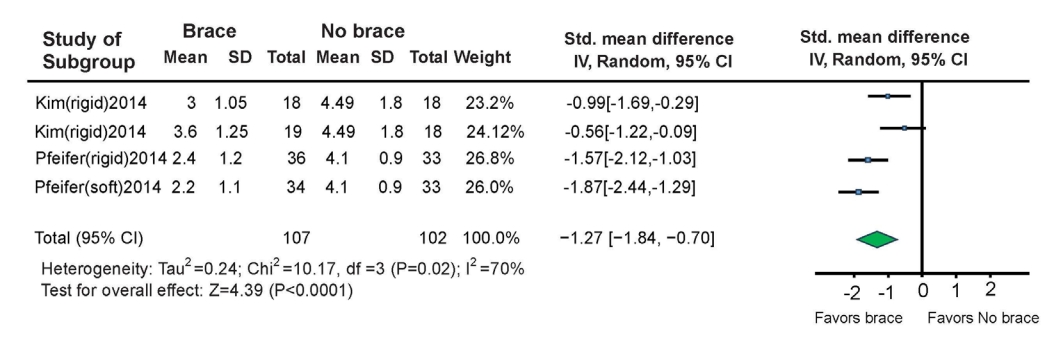
Fig.┬Ā4.
Five double-blind trials (DBTs) on PVP and sham surgery. ├Ś indicates that PVP could not be shown to be useful. ╬ö indicates that PVP was useful in some cases. BMD, bone mineral density; FX duration, duration of procedure from fracture; Early VP, percentage of all patients who underwent vertebroplasty within 3 weeks; Inpatients, percentage of patients who required hospitalization; PMMA, polymethyl methacrylate; NR, not reported.
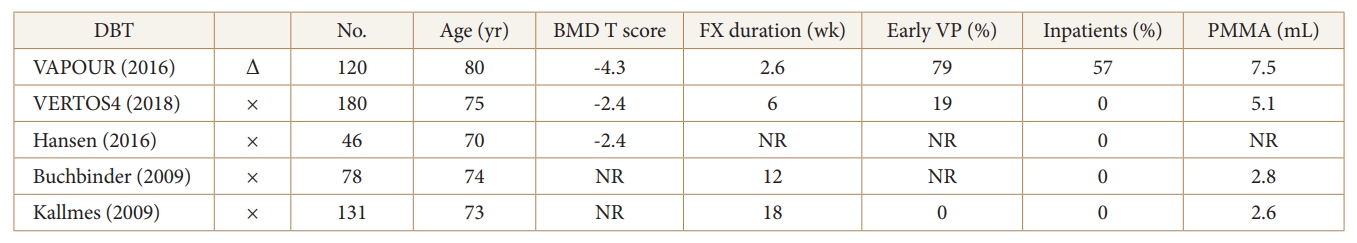
Fig.┬Ā5.
Forest plot showing the delta visual analogue scale in vertebroplasty and kyphoplasty [36]. SD, standard deviation; IV, inverse variance; df, degrees of freedom; CI, confidence interval.
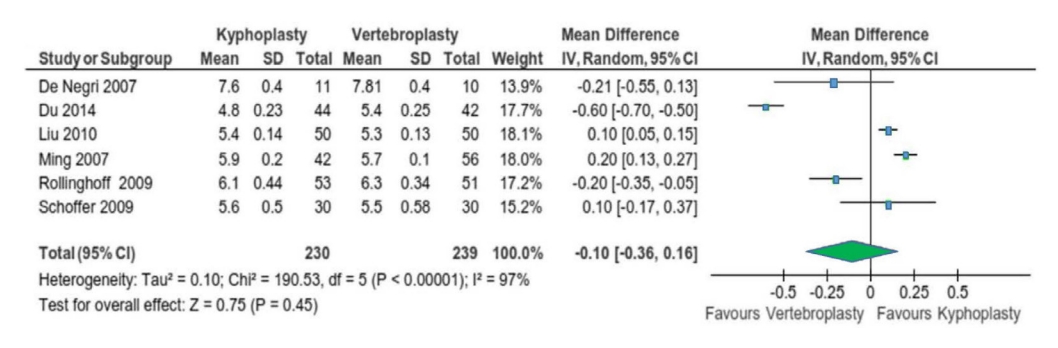
Fig.┬Ā6.
Forest plot showing the delta Oswestry Disability Index in vertebroplasty and kyphoplasty [36]. SD, standard deviation; IV, inverse variance; df, degrees of freedom; CI, confidence interval.

REFERENCES
1. Cha KH, Cho TG, Kim CH, et al. Comparative study on the period of absolute bed rest of vertebral compression fracture. Korean J Spine 2013;10:144-8.



2. Kim SD, Park JY. Pain management for osteoporosis. Korean J Spine 2005;2:93-100.
3. Schnake KJ, Blattert TR, Hahn P, et al. Classification of osteoporotic thoracolumbar spine fractures: recommendations of the Spine Section of the German Society for Orthopaedics and Trauma (DGOU). Global Spine J 2018;8(2 Suppl):46S-49S.




4. Audige L, Bhandari M, Hanson B, et al. A concept for the validation of fracture classifications. J Orthop Trauma 2005;19:401-6.

5. Ameis A, Randhawa K, Yu H, et al. The Global Spine Care Initiative: a review of reviews and recommendations for the non-invasive management of acute osteoporotic vertebral compression fracture pain in low- and middle-income communities. Eur Spine J 2018;27:861-9.



6. Rzewuska M, Ferreira M, McLachlan AJ, et al. The efficacy of conservative treatment of osteoporotic compression fractures on acute pain relief: a systematic review with meta-analysis. Eur Spine J 2015;24:702-14.



7. Pieroh P, Spiegl UJA, Volker A, et al. Spinal orthoses in the treatment of osteoporotic thoracolumbar vertebral fractures in the elderly: a systematic review with quantitative quality assessment. Global Spine J 2023;13(1_suppl):59S-72S.




8. Squires M, Green JH, Patel R, et al. Clinical outcomes after bracing for vertebral compression fractures: a systematic review and meta-analysis of randomized trials. J Spine Surg 2023;9:139-48.



9. Kato T, Inose H, Ichimura S, et al. Comparison of rigid and soft-brace treatments for acute osteoporotic vertebral compression fracture: a prospective, randomized, multicenter study. J Clin Med 2019;8:198.



10. Li M, Law SW, Cheng J, et al. A comparison study on the efficacy of SpinoMed(R) and soft lumbar orthosis for osteoporotic vertebral fracture. Prosthet Orthot Int 2015;39:270-6.

11. Meccariello L, Muzii VF, Falzarano G, et al. Dynamic corset versus three-point brace in the treatment of osteoporotic compression fractures of the thoracic and lumbar spine: a prospective, comparative study. Aging Clin Exp Res 2017;29:443-9.



12. Kim HJ, Yi JM, Cho HG, et al. Comparative study of the treatment outcomes of osteoporotic compression fractures without neurologic injury using a rigid brace, a soft brace, and no brace: a prospective randomized controlled non-inferiority trial. J Bone Joint Surg Am 2014;96:1959-66.

13. Abe T, Shibao Y, Takeuchi Y, et al. Initial hospitalization with rigorous bed rest followed by bracing and rehabilitation as an option of conservative treatment for osteoporotic vertebral fractures in elderly patients: a pilot one arm safety and feasibility study. Arch Osteoporos 2018;13:134.




14. Murata K, Watanabe G, Kawaguchi S, et al. Union rates and prognostic variables of osteoporotic vertebral fractures treated with a rigid external support. J Neurosurg Spine 2012;17:469-75.


15. Liaw MY, Chen CL, Chen JF, et al. Effects of Knight-Taylor brace on balance performance in osteoporotic patients with vertebral compression fracture. J Back Musculoskelet Rehabil 2009;22:75-81.


16. Jacobs E, Senden R, McCrum C, et al. Effect of a semirigid thoracolumbar orthosis on gait and sagittal alignment in patients with an osteoporotic vertebral compression fracture. Clin Interv Aging 2019;14:671-80.


17. Valentin GH, Pedersen LN, Maribo T. Wearing an active spinal orthosis improves back extensor strength in women with osteoporotic vertebral fractures. Prosthet Orthot Int 2014;38:232-8.



18. Diamond T, Clark W, Bird P, et al. Early vertebroplasty within 3 weeks of fracture for acute painful vertebral osteoporotic fractures: subgroup analysis of the VAPOUR trial and review of the literature. Eur Spine J 2020;29:1606-13.



19. Clark W, Diamond T. Early vertebroplasty for severely painful acute osteoporotic compression fractures: a critical review of the literature. Cardiovasc Intervent Radiol 2023;46:1439-46.




20. Galivanche AR, Toombs C, Adrados M, et al. Cement augmentation of vertebral compression fractures may be safely considered in the very elderly. Neurospine 2021;18:226-33.




21. Han S, Park HS, Pee YH, et al. The clinical characteristics of lower lumbar osteoporotic compression fractures treated by percutaneous vertebroplasty: a comparative analysis of 120 cases. Korean J Spine 2013;10:221-6.



22. Eneling J, Darsaut TE, Veilleux C, et al. Understanding the choice of control group: a systematic review of vertebroplasty trials for osteoporotic vertebral compression fractures. Neurochirurgie 2023;69:101401.


23. Buchbinder R, Busija L. Why we should stop performing vertebroplasties for osteoporotic spinal fractures. Intern Med J 2019;49:1367-71.



24. Halvachizadeh S, Stalder AL, Bellut D. Systematic review and meta-analysis of 3 treatment arms for vertebral compression fractures: a comparison of improvement in pain, adjacent-level fractures, and quality of life between vertebroplasty, kyphoplasty, and nonoperative management. JBJS Rev 2021 Oct 25 9(10):doi: 10.2106/JBJS.RVW.21.00045.

25. Zhu HT, Ding DG, Wang S, et al. Comparison between percutaneous kyphoplasty and percutaneous vertebroplasty in terms of efficacy in osteoporotic vertebral compression fractures: a meta-analysis. Altern Ther Health Med 2022;28:49-53.

26. Zhou Y, Jiang J, Gu F, et al. Comparison of therapeutic effects of PVP and PKP combined with triple medication on mild and moderate osteoporotic vertebral compression fracture in the elderly. Front Surg 2021;8:663099.



27. Zhang J, Fan Y, He X, et al. Is percutaneous kyphoplasty the better choice for minimally invasive treatment of neurologically intact osteoporotic KummellŌĆÖs disease? A comparison of two minimally invasive procedures. Int Orthop 2018;42:1321-6.

28. Wang F, Wang LF, Miao DC, et al. Which one is more effective for the treatment of very severe osteoporotic vertebral compression fractures: PVP or PKP? J Pain Res 2018;11:2625-31.




29. Kim P, Kim SW. Balloon kyphoplasty: an effective treatment for kummell disease? Korean J Spine 2016;13:102-6.




30. Cheng J, Muheremu A, Zeng X, et al. Percutaneous vertebroplasty vs balloon kyphoplasty in the treatment of newly onset osteoporotic vertebral compression fractures: a retrospective cohort study. Medicine (Baltimore) 2019;98:e14793.


31. Chang JZ, Bei MJ, Shu DP, et al. Comparison of the clinical outcomes of percutaneous vertebroplasty vs. kyphoplasty for the treatment of osteoporotic KummellŌĆÖs disease: a prospective cohort study. BMC Musculoskelet Disord 2020;21:238.


32. Li Y, Feng X, Pan J, et al. Percutaneous vertebroplasty versus kyphoplasty for thoracolumbar osteoporotic vertebral compression fractures in patients with distant lumbosacral pain. Pain Physician 2021;24:E349-56.

33. Bae IS, Moon BG, Kang HI, et al. Difference in the Cobb angle between standing and supine position as a prognostic factor after vertebral augmentation in osteoporotic vertebral compression fractures. Neurospine 2022;19:357-66.




34. Gan M, Zou J, Song D, et al. Is balloon kyphoplasty better than percutaneous vertebroplasty for osteoporotic vertebral biconcave-shaped fractures? Acta Radiol 2014;55:985-91.



35. Patel N, Jacobs D, John J, et al. Balloon kyphoplasty vs vertebroplasty: a systematic review of height restoration in osteoporotic vertebral compression fractures. J Pain Res 2022;15:1233-45.




36. Daher M, Kreichati G, Kharrat K, et al. Vertebroplasty versus kyphoplasty in the treatment of osteoporotic vertebral compression fractures: a meta-analysis. World Neurosurg 2023;171:65-71.


37. Du J, Li X, Lin X. Kyphoplasty versus vertebroplasty in the treatment of painful osteoporotic vertebral compression fractures: two-year follow-up in a prospective controlled study. Acta Orthop Belg 2014;80:477-86.

38. Ming JH, Zhou JL, Zhou PH, et al. Comparison of therapeutic effect between percutaneous kyphoplasty and pedicle screw system on vertebral compression fracture. Chin J Traumatol 2007;10:40-3.

39. Rollinghoff M, Siewe J, Zarghooni K, et al. Effectiveness, security and height restoration on fresh compression fractures--a comparative prospective study of vertebroplasty and kyphoplasty. Minim Invasive Neurosurg 2009;52:233-7.


40. Schofer MD, Efe T, Timmesfeld N, et al. Comparison of kyphoplasty and vertebroplasty in the treatment of fresh vertebral compression fractures. Arch Orthop Trauma Surg 2009;129:1391-9.



41. Vogl TJ, Pflugmacher R, Hierholzer J, et al. Cement directed kyphoplasty reduces cement leakage as compared with vertebroplasty: results of a controlled, randomized trial. Spine (Phila Pa 1976) 2013;38:1730-6.

42. De Negri P, Tirri T, Paternoster G, et al. Treatment of painful osteoporotic or traumatic vertebral compression fractures by percutaneous vertebral augmentation procedures: a nonrandomized comparison between vertebroplasty and kyphoplasty. Clin J Pain 2007;23:425-30.

43. Liu JT, Liao WJ, Tan WC, et al. Balloon kyphoplasty versus vertebroplasty for treatment of osteoporotic vertebral compression fracture: a prospective, comparative, and randomized clinical study. Osteoporos Int 2010;21:359-64.



44. Najjar E, Mardashti A, Komaitis S, et al. Does kyphoplasty affect the global sagittal alignment in patients with osteoporotic vertebral fractures? A systematic review and meta-analysis. Eur Spine J 2023;32:38-45.



45. Liu D, Xu J, Wang Q, et al. Timing of percutaneous balloon kyphoplasty for osteoporotic vertebral compression fractures. Pain Physician 2023;26:231-43.

46. Carli D, Venmans A, Lodder P, et al. Vertebroplasty versus active control intervention for chronic osteoporotic vertebral compression fractures: the VERTOS V randomized controlled trial. Radiology 2023;308:e222535.