|
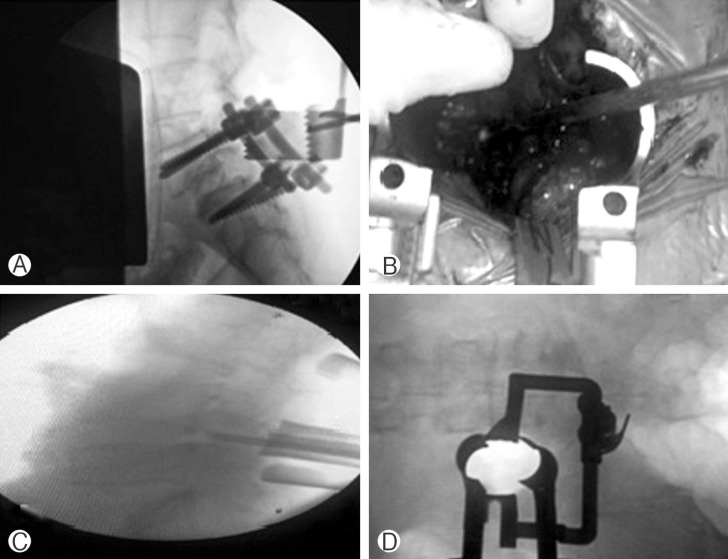
 |
- Search
Abstract
Objective
Mini-transforaminal lumbar interbody fusion (Mini-TLIF) and other minimally invasive approaches introduced for the purpose of treating lumbar degenerative disc disease and instability are achieving high success and safety rates as the conventional approaches. Moreover, it has less soft tissue damage, minimal blood loss, and less hospital stay.
Methods
A prospective study was conducted from 2012 to 2014 on 28 patients who were subjected to Mini-open TLIF combined with transpedicular screw fixation for spondylolisthesis and degenerative disc disease. Two paramedian approaches were done, 4 cm for each, to insert the pedicular screws, along with inserting unilateral TLIF cage with autologous bone graft. Decompression was done either unilateral or bilateral according to the patient side of radiculopathy. Sixteen patients (57.2%) were diagnosed with degenerative spondylolisthesis, 7 patients (25%) were diagnosed with isthmic type spondylolisthesis, and 5 patients (17.8%) were diagnosed with degenerative disc disease, 2 of them(7.1%) had previous operations at the same level. Twenty patients (71.4%) were operated at the L4/5 level, and 8 patients (28.6%) at the L5/S1 level.
Results
All patients were able to ambulate the next day of surgery. The mean estimated blood loss was 251.79mL. The average hospital stay was 4.14 days. The average follow-up was 9 months. The mean visual analog scale was 1.86 at discharge, 1.68 after 3 months, and 1.38 after 6 months. After 6 months of the operation, MacNab's criteria were good in 23 patients and excellent in 5 patients. We had one case with transient weakness, 2 cases of screw malposition without clinical manifestations, and one case of infection.
In 1968, Wiltse et al.20) first described paraspinal sacrospinalis muscle-splitting approach to lumbar spine. This approach decreased bleeding and provided more direct access to the transverse processes and pedicles.
Mini-transforaminal lumbar interbody fusion (Mini-TLIF) is a powerful minimally invasive surgical (MIS) technique that achieves many goals e.g., decompression, interbody fusion, posterolateral fusion, pedicle screw instrumentation, and low-grade spondylolisthesis reduction; as well as minimum incision size and muscle devitalization as other MIS techniques10). This technique is performed in patients with refractory mechanical low back and radicular pain associated with spondylolisthesis, degenerative disc disease, and recurrent disc herniation12).
The Mini-TLIF technique is performed via microscopic visualization and specially designed retractor; providing an excellent exposure as conventional TLIF. The nerve roots can be decompressed with two paramedian small incisions, followed by interbody fusion and transpedicular screws' fixation16).
Decreased both blood loss and muscle trauma, along with shorter hospital stay are associated with TLIF procedures when using minimally invasive approaches9).
The aim of this study is to demonstrate the surgical technique and advantages of the mini-open transforaminal approach for lumbar interbody fusion (Mini-TLIF); combined with transpedicular screw fixation. Clinical and radiographic results will be assessed to determine the clinical outcomes in twenty eight patients selected for mini-open technique for TLIF.
A prospective cross sectional study was performed throughout the period from March 2012 to December 2014, on 28 patients who were subjected to one level Mini-TLIF with transpedicular screw fixation, and unilateral or bilateral decompression. Our selection was directed towards patients with refractory cases (failure of conservative treatment for 3 months), mechanical low back, radicular pain associated with spondylolisthesis, degenerative disc disease, and recurrent disc herniation. All patients were assessed preoperatively with full history and clinical examination, radiological assessment with magnetic resonance imaging (MRI) and plain erect radiographs (static, dynamic, and oblique views) of the lumbosacral spine, and routine preoperative laboratory investigation for general anesthesia.
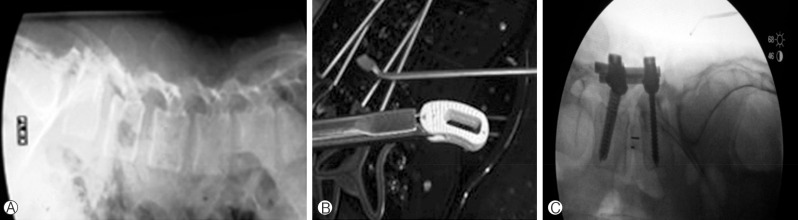
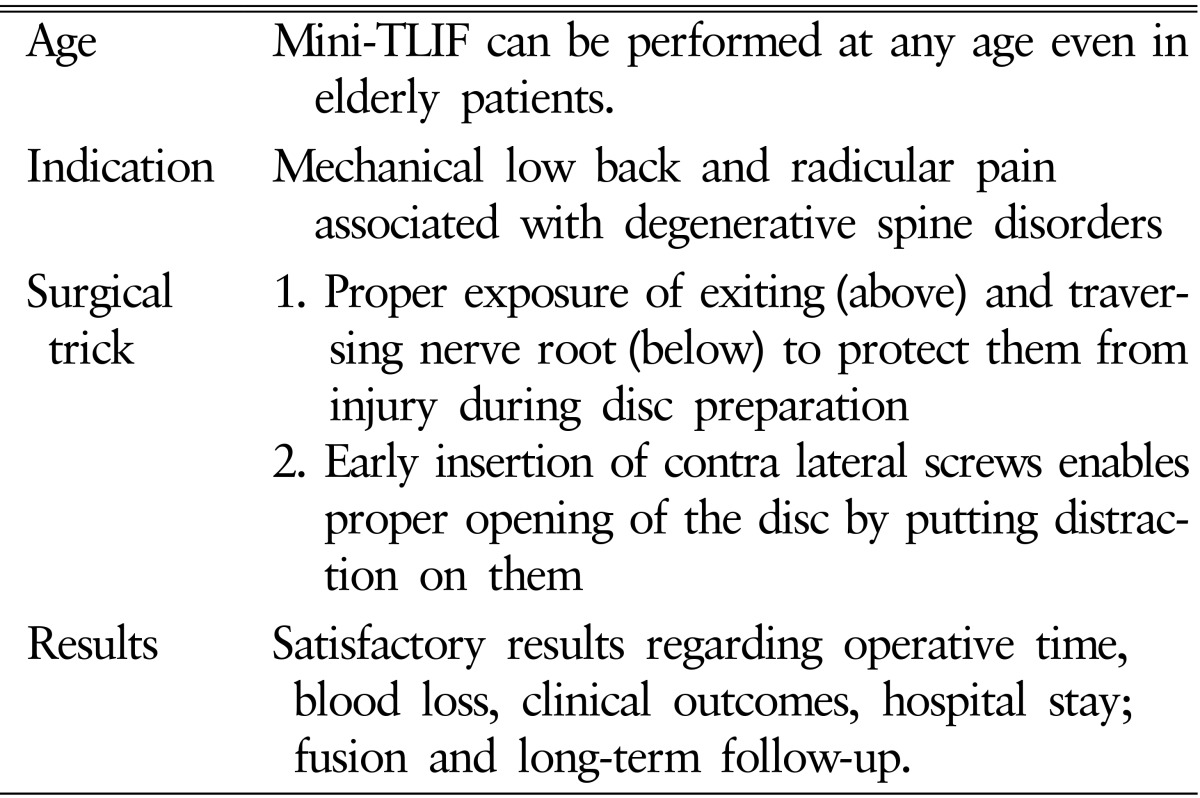
The procedure is done under general anesthesia in prone position on a radiolucent table. The skin incision is leveled and fashioned using the C arm by marking the pedicle entry points on both sides using both anterior-posterior and lateral views; and connecting a line between the 2 marks. The skin incision is usually 2 finger breadth off the midline and about 4 cm in length (Fig. 1).
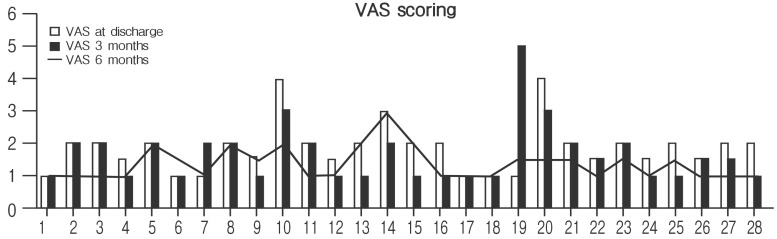
Once incision is done, the paraspinal muscles are dissected in blunt fashion using the index fingers, and then we try to feel the facet of interest and the one above. We use special retractors designed for this approach if available, or we use regular Williams retractor (Fig. 2). After proper positioning of the retractor, we use the C arm to confirm the appropriate level and the facet of interest. We used to put the screws in the cranial vertebra (of both sides) and one at the caudal vertebra at the contralateral side of facetectomy. Care should be taken not to open or injure the facet joints of the cranial vertebra.
Once that is established, we track the last screw and put a mark inside so not to interfere with the insertion of the cage, and also to avoid excessive drilling that might reach the pedicle of the last screw.
We found that, putting the screws early before preparing the disk disc space and putting the cage, can help in opening the disc space by putting distraction on the contralateral screws, especially when the disc space is very narrow and in second degree slippage.
After that, we go on facetectomy using high speed drill if available or otherwise using osteotome and a mallet. Care should be taken in order not to injure or weaken the pedicle. We first free the inferior facet from the lamina, and then we free it from the pars interarticularis. Ligamentum flavum is then removed to identify the disc space and to clear out the exiting and traversing nerve roots to protect them from injury during preparation of the disc space and insertion of the cage. We open the disc space with a scalpel and evacuate its content with pituitary roungeurs. The cartilaginous end plates are then removed using special instrumentation. Care should be taken not to injure the bony endplates as this may increase the chance of vertebral subsidence against the interbody cage. After preparing the disc space and removing the cartilaginous end plates, we use trials to measure the appropriate size and length of the interbody cage (Fig. 3). We pack the floor of the disc space with bone taken from the facetectomy before insertion of the TLIF cage which is also filled with bone to enhance fusion.
After checking the proper placement of interbody cage, we place the rods and tighten the screws in compression to restore the normal lordosis and prevent cage migration (Fig. 4). The wound is irrigated with antibiotic solution and then closed in layers. We rarely use subfascial drain that is removed after 24 hours. We have the option to do a single paramedian incision if we have to decompress one side and putting the screws on the contralateral side by a percutaneous technique, or doing 2 paramedian skin incisions for bilateral decompression. However we prefer using two paramedian incisions for most of the cases as it is significantly cheaper than the percutaneous systems.
Both intraoperative blood loss and postoperative pain score on a 10-point visual analogue scale (VAS) were assessed right before discharge, 3 months, and 6 months postoperative. Mac-Nab's criteria were used to assess the clinical outcome six months postoperative. According to MacNab's criteria, the results were described as excellent (completely pain free), good (minor intermittent discomfort, not interfering with normal activities), fair (improvement in symptoms but persistent backache or sciatica interfering with capacity to engage in full normal activities) and poor (no change in symptoms). The fusion rate was assessed 6 to 15 months after the operation. We judged the fusion in the form of solid construct without change in the dynamic plain radiographs, absent system failure or pseudoarthrosis in the form of black hallows around the screws, and lucency around the interbody cage.
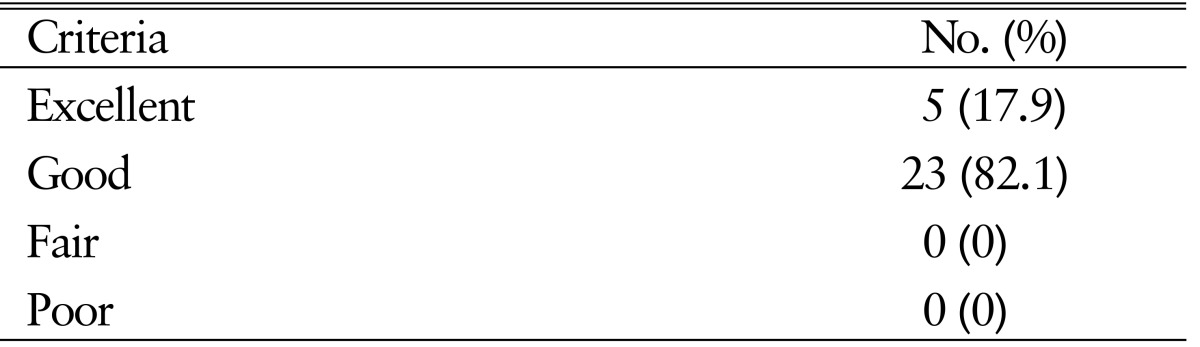
We operated 28 patients with the youngest was 30 years and the oldest was 71 years old with mean age of 48.29 years. They were 16 female (57.1%) and 12 male patients (42.9%), 16 out of the 28 patients (57.2%) had degenerative spondylolisthesis, 7 patients (25%) were diagnosed with isthmic type spondylolisthesis, and 5 patients (17.8%) were diagnosed with degenerative disc disease; 2 of them(7.1%) had previous operation at the same level. All patients in the study were complaining of back pain (100%). Fifteen patients (53.6%) had unilateral radiculopathy, 13 (46.4%) had bilateral radiculopathy, and only 1 patient had weakness (3.6%).
Twenty patients (71.4%) were operated at the L4/5 level and 8 patients (28.6%) at L5/S1 level. The minimum estimated blood loss intraoperative was 150mL and the maximum amount was 300mL, with mean blood loss 251.79mL. The minimum hospital stay was 3 days and the maximum was 6 days; with an average hospital stay 4.14 days.
The complications, on the other hand, were assessed and the results came as follows; 1 case of infection (3.6%) after 1 month of good improvement postsurgery as symptoms recurred with elevated both C-reactive protein and erythrocyte sedimentation rate levels. After 2 months of treatment with parenteral antibiotics, symptoms improved and laboratory investigations returned to normal values. One case of adjacent segment failure (3.6%) presented with back pain 18 months postoperative, the diagnosis was proved by MRI that showed disc degeneration at the level above the fused segment. The patient showed satisfactory improvement with medical treatment and physiotherapy without a need for fusion extension. We had 2 cases (7.1%) diagnosed with malposition of pedicular screws, using regular postoperative computed tomography. The malposition, however, was not associated with any clinical manifestation; thus needed no further operative correction. There was 1 case of immediate weakness postoperative (grade 3 weakness of the dorsiflexion of the ankle) that showed improvement with steroids and completely gained back power within 3 months postoperative. The weakness may be attributed to complete reduction of the slippage or rough manipulation of the root during cage insertion.
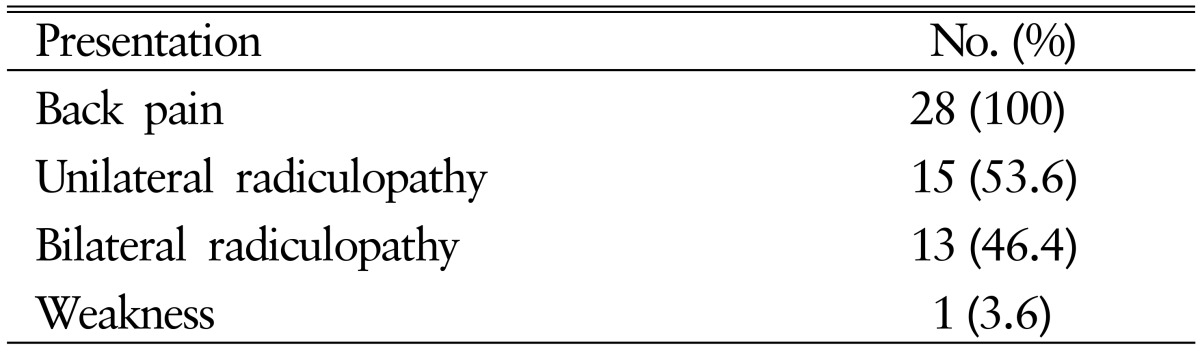
It was assessed using VAS scoring at discharge, 3 months, and 6 months postoperative (Fig. 5). The results came as follows, the mean VAS was 7.5 preoperatively, 1.86 at discharge, 1.68 after 3 months, and 1.38 after 6 months.
The MacNab's criteria was used to assess the clinical outcomes 6 months after the operation, and results came as follows; good in 23 and excellent in 5 cases.
All patients have probably fused, as we have, in an average period of 15 months of follow-up postsurgery no system failure, no pseudoarthrosis, or any movement in the construct in dynamic films in average period of 9 months of follow-up postoperative. All cases showed radiological evidence of increased disc height and foraminal height in comparison to preoperative films.
The aim of surgical treatment in lumbar spine surgery (when indicated) is to decompress the neural tissue and immobilize unstable parts of the spine. This is done with elimination of motion through the facet joint and the intervertebral disc through fusion18,22). All fusion techniques are augmented with instrumentation (anterior plates, posterior pedicle screws, various materials and cages for interbody fusion)3). Posterolateral fusion is performed through traditional midline posterior approach with decortication of transverse process, facets and pars to enhance fusion with allo or autograft bone, and supplemented with transpedicular screws3). However, persistence of discogenic pain was reported and explained by the presence of micromotion in the involved disc. For this reason and in addition to the fact that lumbar vertebral body account for most of surface area and support load to the spine (90% and 80%, respectively), lumbar interbody fusion is recommended by many studies for better correction and maintenance of sagittal and coronal plane2).
There are several varieties of lumbar interbody fusion which include: Anterior lumbar interbody fusion in which the intervertebral disc is approached anteriorly via either intra abdominal or retroperitoneal routes7), extreme lateral lumbar interbody fusion in which access is done through psoas muscle to the retroperitoneal space6), and posterior lumbar interbody fusion (PLIF) in which the disc is approached posteriorly through laminectomy, partial facetectomy and retraction of the dura. Finally there is TLIF in which the disc is approached by complete facetectomy (unilateral). PLIF and TLIF have become popular among neurosurgeons who are accustomed to posterior approach11,15). The laminectomy and bilateral partial facetectomy that needed in PLIF are unnecessary in TILF. Thus TLIF shortens surgical time and decreases blood loss, risk of conus injury, dural tear, and epidural scarring. Moreover, the posterolateral access through TLIF is thought to decrease postoperative pain and preserve the supraspinous and interspinous processes19). The efficiency of TLIF has been reported by many studies12,15,16,17,18,19,20,21,22). Advances in this approach have led to three subtypes of TILF12); namely, opening using conventional posterior midline approach (first introduced by Harms and Rolinger in 1982)8), miniopen (initially described by Foley et al. in 2003)5) by using bilateral skin incision 3.5-4 cm in length followed by application of expandable tubular retractors, and most recently, the minimally invasive subtype with nonexpandable or expandable tubular retractor with all screws are percutaneously placed. In this study the miniopen subtype is prefered as it is more compatible with financial resources of our hospital as well as providing the same benefits of the minimally invasive TILF.
The surgical technique used in this work is the same as other studies except that some of them are related to our financial resources whilst others were done to achieve better surgical outcomes. We use the special retractors designed for this approach but when they are not available, the regular Williams retractors were used with sufficient exposure results. Most of the studies recommend insertion of the cage before the transpedicular screws to avoid narrowing and limitation of working access to more disc space by screw heads. However, we found that earlier screw insertion can help more in the opening of the disc space and insertion of the cage by performing disraction on the contralateral side. This will be very helpful in cases when disc space is significantly narrowed or in case of second degree slippage. One of the most important points that were stressed during our surgical work is the proper exposure of the exiting root (above) and the emerging root (below) to avoid any neurological injury during disc opening and evacuation especially toward the above exiting root that can be hidden and injured with insufficient exposure or experience.
The selection criteria in this work follow the same lumbar fusion guidelines mentioned in other studies5,9,12). We included cases with mechanical low back pain resulting from degenerative disc disease as well as spinal instability resulting from scoliosis or spondylithesis. The contraindications for this approach are usually relative which include cases that need fusion at three or more segments, deep exposure more than 9 cm as the maximum retractor length, high grade spondylithesis and deformity that requires osteotomies and multiple reductions beyond the working space provided by this approach, and also patients with distorted anatomical landmarks for pedicular screws insertion. In addition TLIF is not recommended in severe osteoprosis12).
This minimally invasive technique can be done even in old age. In our study we had 28 patients having mean age of 48.28 years, with the youngest was 30 years and the oldest was 71 years old. This technique was performed in older ages more than in other studies11,16).
As with other minimal invasive techniques, this technique has minimal intraoperative blood loss, shorter surgery time, and shorter hospital stay with early ambulation. The minimum estimated intraoperative blood loss was 150mL, whilst the maximum was 300mL, with mean blood loss 251.79mL. This goes with Wang et al.17) who reported that the average intraoperative blood loss was 264±89mL and Tangviriyapaiboon16) who reported 398.3mL. Our results were slightly more than Oh et al.13) who reported 163mL, Dhall et al.4) 194mL and Peng et al.14) 150mL.
The minimum hospital stay was 3 days and the maximum was 6 days; with an average hospital stay of 4.14 days. All patients in our study started to ambulate next day after surgery. These results coincide with what was reported in other studies1,4,14,16,17).
Clinical outcomes were assessed using VAS scoring at discharge, 3 months, and 6 months postoperative. The mean VAS was 7.5 preoperatively, 1.86 at discharge, 1.68 after 3 months, and 1.38 after 6 months. Tangviriyapaiboon16) (VAS at discharge 1.5, 3 months 1.6, 6 months 1.28), and Wang et al.17) who reported that VAS scoring at the third day after surgery was 1.34±0.5 and latest VAS after 6 months postoperative was 0.92±0.5. It is noticed that our results regarding VAS are slightly lower than other studies in the direct postoperative time, but are comparable to them after 3 and 6 months. This is attributed to our surgical technique with open screw system that necessitates more paraspinal incisions and subsequently more postoperative pain in comparison with percutaneous screw system. However, this is tolerated by our patient because of marked improvement in VAS score pre- and postoperative, especially on the long term.
The MacNab's criteria, 6 months after the operation, were good in 23 patients and excellent in 5 patients. All these results are comparable with other studies1,4,14,16,17).
Taking a look to the complications reported in our study (1 infection that responds well to antibiotic, 1 adjacent segment failure, 2 cases with acceptable screw malposition, and 1 case of temporary weakness) and other authors' results, we will find that the overall complications related to this procedure were acceptable, which means that the mini-open TLIF procedure appears to be a safe way to treat degenerative lumbar spine diseases in selective cases1,4,14,16,17).
All patients were probably fused, as we have no system failure, no pseudarthrosis, or any movement in the construct in dynamic films in average period of 9 months of follow-up postoperative. Dhall et al.4) reported 1 case (4.7%) of pseudoarthrosis in his study of 21 patients subjected to mini-open TLIF. All patients showed radiological evidence of increased both disc and foraminal height, in comparison with preoperative films.
NOTES
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
1. Adogwa O, Parker SL, Bydon A, Cheng J, McGirt MJ. Comparative effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion: 2-year assessment of narcotic use, return to work, disability, and quality of life. J Spinal Disord Tech 2011 24:479-484. PMID: 21336176.


2. Barrick WT, Schofferman JA, Reynolds JB, Goldthwaite ND, McKeehen M, Keaney D, et al. Anterior lumbar fusion improves discogenic pain at levels of prior posterolateral fusion. Spine (Phila Pa 1976) 2000 25:853-857. PMID: 10751297.


3. Bono CM, Lee CK. Critical analysis of trends in fusion for degenerative disc disease over the past 20 years: influence of technique on fusion rate and clinical outcome. Spine (Phila Pa 1976) 2004 29:455-463. PMID: 15094543.


4. Dhall SS, Wang MY, Mummaneni PV. Clinical and radiographic comparison of mini-open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up. J Neurosurg Spine 2008 9:560-565. PMID: 19035748.


5. Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine (Phila Pa 1976) 2003 28(15 suppl):S26-S35. PMID: 12897471.


6. Fritzell P, Högg O, Wessberg P, Nordwall A. Swedish Lumbar Spine Study Group: Chronic low back pain and fusion: a comparison of three surgical techniques: a prospective multicenter randomized study from the Swedish lumbar spine study group. Spine (Phila Pa 1976) 2002 27:1131-1141. PMID: 12045508.


7. Hackenberg L, Liljenqvist U, Halm H, Winkelmann W. Occlusion of the left common iliac artery and consecutive thromboembolism of the left popliteal artery following anterior lumbar interbody fusion. J Spinal Disord 2001 14:365-368. PMID: 11481562.


8. Harms J, Rolinger H. A one-stager procedure in operative treatment of spondylolistheses: dorsal traction-reposition and anterior fusion (author's transl). Z Orthop Ihre Grenzgeb 1982 120:343-347. PMID: 7113376.


9. Holly LT, Schwender JD, Rouben DP, Foley KT. Minimally invasive transforaminal lumbar interbody fusion: indications, technique, and complications. Neurosurg Focus 2006 20:E6.

10. Kim KT, Lee SH, Suk KS, Bae SC. The quantitative analysis of tissue injury markers after mini-open lumbar fusion. Spine (Phila Pa 1976) 2006 31:712-716. PMID: 16540878.


11. Lowe TG, Tahernia AD, O'Brien MF, Smith DA. Unilateral transforaminal posterior lumbar interbody fusion (TLIF): indications, technique, and 2-year results. J Spinal Disord Tech 2002 15:31-38. PMID: 11891448.


12. Meyer SA, Wu JC, Mummaneni PV. Mini-open and minimally invasive transforaminal lumbar interbody fusion: technique review. Semin Spine Surg 2011 23:45-50.

13. Oh CH, Hyun D, Yoon SH, Park H. Mini-open and conventional-open transforaminal lumbar interbody fusion augmented by pedicle screw fixation: comparisonal result of clinical, perioperative parametric, functional and radiological assessments. J Spine 2013 2:136.
14. Peng CW, Yue WM, Poh SY, Yeo W, Tan SB. Clinical and radiological outcomes of minimally invasive versus open transforaminal lumbar interbody fusion. Spine (Phila Pa 1976) 2009 34:1385-1389. PMID: 19478658.


15. Salehi SA, Tawk R, Ganju A, LaMarca F, Liu JC, Ondra SL. Transforaminal lumbar interbody fusion: surgical technique and results in 24 patients. Neurosurgery 2004 54:368-374. PMID: 14744283.


16. Tangviriyapaiboon T. Mini-open transforaminal lumbar interbody fusion. J Med Assoc Thai 2008 91:1368-1376. PMID: 18843866.

17. Wang J, Zhou Y, Zhang ZF, Li CQ, Zheng WJ, Liu J. Comparison of one-level minimally invasive and open transforaminal lumbar interbody fusion in degenerative and isthmic spondylolisthesis grades 1 and 2. Eur Spine J 2010 19:1780-1784. PMID: 20411281.



18. Weinstein JN, Lurie JD, Tosteson TD, Hanscom B, Tosteson AN, Blood EA, et al. Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med 2007 356:2257-2270. PMID: 17538085.



19. Whitecloud TS 3rd, Roesch WW, Ricciardi JE. Transforaminal interbody fusion versus anterior-posterior interbody fusion of the lumbar spine: a financial analysis. J Spinal Disord 2001 14:100-103. PMID: 11285420.


20. Wiltse LL, Bateman JG, Hutchinson RH, Nelson WE. The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Joint Surg Am 1968 50:919-926. PMID: 5676831.


21. Wu RH, Fraser JF, Härtl R. Minimal access versus open transforaminal lumbar interbody fusion: meta-analysis of fusion rates. Spine (Phila Pa 1976) 2010 35:2273-2281. PMID: 20581757.


22. Yan DL, Pei FX, Li J, Soo CL. Comparative study of PILF and TLIF treatment in adult degenerative spondylolisthesis. Eur Spine J 2008 17:1311-1316. PMID: 18685873.



Fig. 1
Skin marking (A) using fluoroscopy (B, C) and surgical incisions (D). The arrow is directed to the paramedian needle put for level localization.
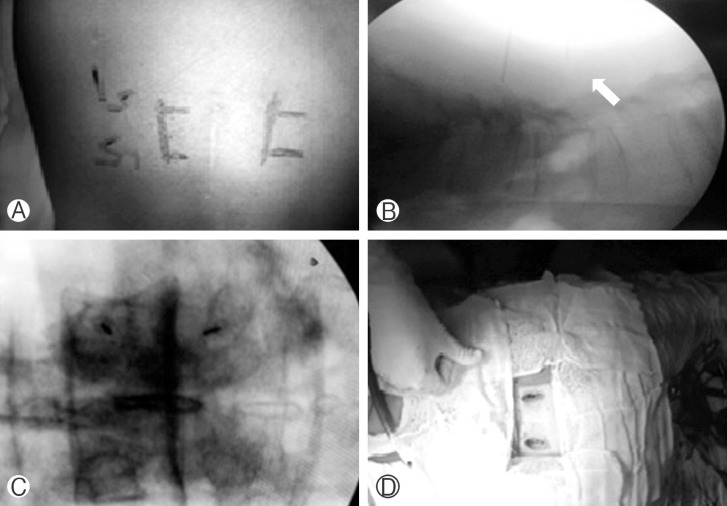
Fig. 2
Intraoperative images of different retractors used in the procedure: (A, B) during facet exposure and removal; (C, D) after facetectomy.

- TOOLS
-
METRICS

-
- 2 Crossref
- Scopus
- 8,469 View
- 159 Download